Why Sleep Gets So Hard During Pregnancy
By the third trimester, many pregnant women feel like they’re sleeping on a beach ball with a side of heartburn. It’s not just discomfort-it’s a physiological shift that can trigger serious sleep disorders. Obstructive sleep apnea (OSA) affects 10.5% of pregnant women in their last trimester, and that number jumps to 26.7% if they have a BMI over 30. Snoring isn’t just annoying-it’s a red flag. When your airway collapses during sleep, your oxygen levels drop, your brain wakes you up silently, and you never get deep rest. Over time, this raises your risk of preeclampsia by 2.3 times, gestational diabetes by 1.7 times, and even cesarean delivery by 2.1 times.
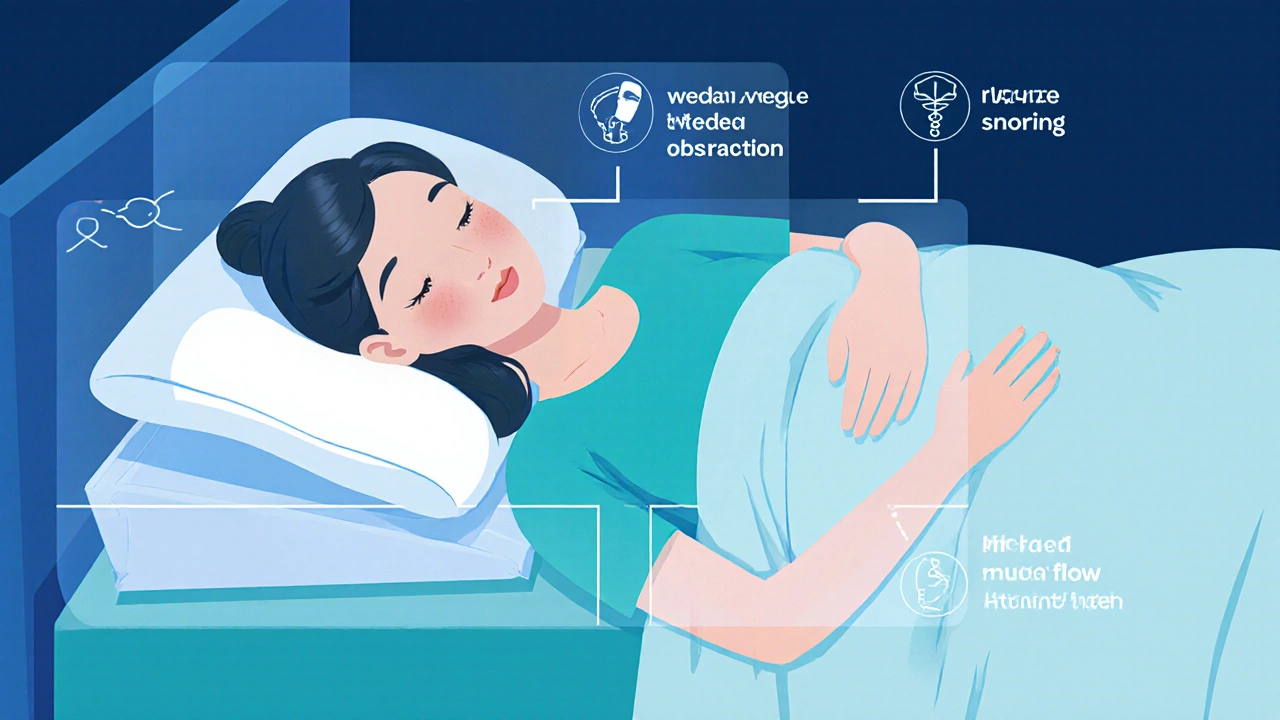
Why does this happen? Your body changes in ways you can’t control. Hormones relax the muscles in your throat. Your neck swells. Your belly pushes up on your diaphragm. Your nose gets congested like you have a cold that never ends. These aren’t quirks-they’re risk factors. And if you’re ignoring loud snoring, gasping at night, or waking up with headaches, you’re not just tired-you might have a medical condition that needs attention.
How to Know If You Have Sleep Apnea (Not Just Snoring)
Not every snorer has sleep apnea. But if you’re doing all three-snoring loudly, stopping breathing briefly during sleep, and waking up exhausted-you should get checked. The American College of Obstetricians and Gynecologists now recommends all pregnant women be screened at their first prenatal visit using a simple questionnaire called the Berlin Questionnaire. If you score high, your doctor may refer you for a sleep study.
The gold standard is an overnight polysomnography in a lab, but home sleep tests are now approved for low-risk patients. These devices track your breathing, oxygen levels, and heart rate while you sleep in your own bed. You don’t need to be diagnosed with severe apnea to benefit from treatment. Even mild cases (AHI 5-14) can increase your risk of high blood pressure. And here’s the thing: many women don’t get diagnosed until it’s too late. A 2022 survey found that women typically wait 14.3 weeks after symptoms start before getting evaluated. Don’t wait. If your partner says you’re stopping breathing at night, take it seriously.
CPAP: The Most Effective Treatment-And How to Make It Work
Continuous Positive Airway Pressure (CPAP) is the first-line treatment for moderate to severe sleep apnea during pregnancy. It works by gently pushing air through a mask to keep your airway open. Studies show it cuts your risk of preeclampsia by 30% and gestational hypertension by 35% when started between 24-28 weeks.
But many women quit because the mask feels uncomfortable. That’s normal. Your face changes during pregnancy-swelling, nasal congestion, even skin sensitivity. The solution? Use nasal pillows instead of full-face masks. They’re smaller, less bulky, and sit under your nose. Look for devices with built-in humidifiers set to 37°C-this prevents dryness. ResMed’s AirSense 11 Pregnancy Mode, cleared by the FDA in 2022, automatically adjusts pressure as your breathing changes through each trimester.
Adherence is the biggest hurdle. Only 62% of pregnant women stick with CPAP beyond four weeks. But in clinics that offer hands-on training-like a 30-minute fitting session with a sleep tech-adherence jumps to 82%. Don’t just get the machine. Get support. Ask your doctor for a referral to a sleep clinic that specializes in pregnancy. And give yourself time. Most women adapt within 7-14 days. One user on SleepAdvisor.org said her AHI dropped from 18 to 6 in two weeks after switching to the Boppy Noggin CPAP pillow, which holds her in a side-lying position without crushing the mask.
Positioning: The Simple Fix That Works for Mild Apnea
If your apnea is mild (AHI under 15), changing how you sleep can make a big difference. Sleeping on your back is the worst position-it lets your tongue and tissues collapse into your airway. Sleeping on your left side is the best. It improves blood flow to your baby and reduces pressure on your diaphragm. A 2022 study from Brown Health found that left-side sleeping reduced the apnea-hypopnea index (AHI) by 22.7% in women with mild OSA.
But staying on your side all night? Hard to do. That’s where pregnancy pillows come in. Full-body pillows like the Leachco Full Body Pillow Pro ($89.99) wrap around you, supporting your belly, back, and legs. They keep you from rolling onto your back. Don’t just use regular pillows-stacking them under your head can actually worsen apnea by bending your neck. Instead, use a wedge pillow to elevate your upper body 7-8 inches. This keeps your airway open and helps with reflux too.
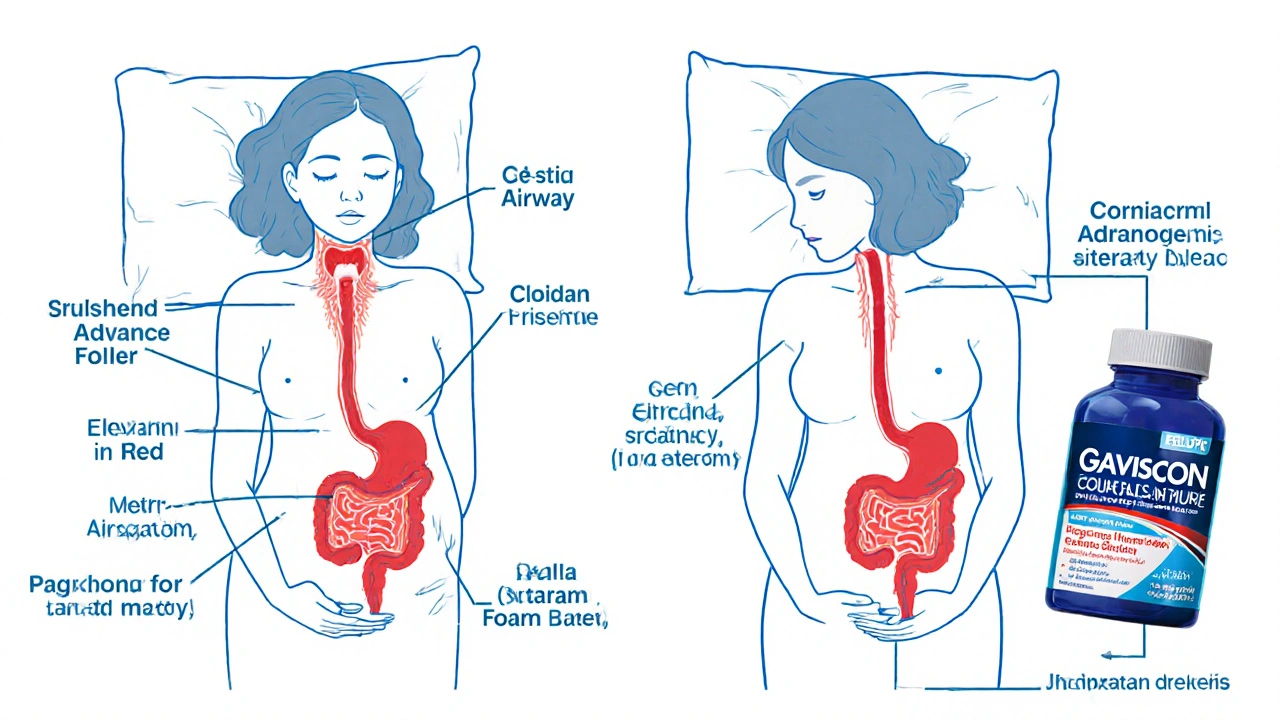
One key tip: don’t sleep flat. Even if you don’t have apnea, elevating your torso helps with heartburn. But here’s the mistake most people make-they prop up just their head. That bends your neck and can block your airway. The right way? Elevate your whole upper body using a wedge under your mattress or a specially designed bed wedge. Studies show this improves oxygen saturation by 3.2% compared to lying flat.
Taming Reflux: It’s Not Just About Antacids
Heartburn during pregnancy isn’t just annoying-it’s linked to poor sleep. When stomach acid flows back, it can trigger coughing, choking, and waking up gasping. But treating it wrong can make apnea worse. Many women take antacids and think they’re fixed. But over-the-counter options like Tums or Maalox don’t always help, and some can interfere with iron absorption.
The most effective solution? Gaviscon Advance ($14.99 for 500ml). It’s an alginate-based antacid that forms a protective foam barrier on top of your stomach contents, preventing acid from rising. Unlike other antacids, it doesn’t get absorbed into your bloodstream, so it’s safe during pregnancy.
But medication alone won’t fix it. Timing matters. Don’t eat within three hours of bed. Avoid spicy, fatty, or acidic foods in the evening. Even a late snack like yogurt or crackers can trigger reflux. And never lie down right after eating. If you need to snack, sit upright for 30 minutes after.
Also, skip the extra pillows under your head. As mentioned, that bends your neck and can narrow your airway. Use a wedge pillow under your torso instead. This elevates your stomach and your head together-keeping acid down and airways open.
What Doesn’t Work (And Why)
There’s a lot of advice out there, and not all of it’s backed by science. Mandibular advancement devices-mouthpieces that push your jaw forward-are popular for non-pregnant adults with apnea. But during pregnancy, your jaw and hormones are changing. There’s no safety data for these devices in pregnant women, and the 2023 SASM/SOAP guidelines specifically advise against them.
Weight loss? It’s tempting to think you should lose weight during pregnancy to fix apnea. But that’s dangerous. The Institute of Medicine recommends gaining 11.5-16 kg if you’re normal weight, and only 5-9 kg if you’re obese. Trying to lose weight can harm your baby’s growth. Instead, focus on staying within those ranges. Eat balanced meals, avoid sugary snacks, and walk daily. Small, steady habits matter more than drastic changes.
And don’t rely on smartphone apps or fitness trackers to diagnose apnea. While the Apple Watch Series 9 now has a sleep apnea detection feature (validated in a 2024 JAMA study), it’s not a diagnostic tool. It can flag possible issues, but it can’t replace a sleep study. Use it as a nudge to talk to your doctor-not as a replacement for medical care.

What to Do After Baby Arrives
Many women think their sleep apnea will vanish after delivery. It often improves-but not always. A 2023 Sleep Cohort Study found that 58% of women who developed OSA during pregnancy went on to develop chronic high blood pressure within 10 years, even if their apnea seemed to disappear after birth.
Some clinics, like Brown Health, recommend a follow-up sleep study at 12 weeks postpartum. Others, like the NIH, say observation is fine if symptoms are gone. The key? Don’t assume it’s over. If you’re still snoring, waking up tired, or feeling foggy during the day after your baby arrives, get tested. Postpartum sleep apnea is often overlooked, but it’s real-and treatable.
Real Stories, Real Results
One woman in Auckland, 34 weeks pregnant, started CPAP after her OB noticed her snoring and elevated blood pressure. Within two weeks, her BP dropped from 145/92 to 120/80. She says the mask felt weird at first, but the humidifier and nasal pillows made all the difference. “I slept like I hadn’t in months,” she said. “And my baby’s movements felt stronger after I started using it.”
Another, who couldn’t tolerate CPAP, switched to a full-body pillow and strict left-side sleeping. Her AHI dropped from 12 to 5. She still gets heartburn, but now she avoids dinner after 6 p.m. and uses Gaviscon Advance. “I don’t wake up choking anymore,” she told her midwife. “I actually feel rested.”
These aren’t outliers. They’re proof that small, targeted changes work. You don’t need to be perfect. You just need to act.
What to Ask Your Doctor
- “Should I be screened for sleep apnea at my next visit?”
- “Do I need a sleep study, or can I start with positional therapy?”
- “What CPAP mask would work best with my face changes?”
- “Is Gaviscon Advance safe for me to use every night?”
- “Will you check my blood pressure again if I start CPAP?”
Don’t be shy. Sleep isn’t a luxury-it’s a medical necessity during pregnancy. And you deserve rest that doesn’t come at the cost of your health-or your baby’s.
Can sleep apnea during pregnancy harm my baby?
Yes. Untreated sleep apnea reduces oxygen flow to your baby, which is linked to a 42% higher risk of fetal growth restriction. It also increases the chance of preterm birth and low birth weight. Studies show that treating apnea with CPAP improves oxygen levels and reduces these risks significantly.
Is it safe to use CPAP while pregnant?
Yes, CPAP is not only safe-it’s recommended for moderate to severe sleep apnea during pregnancy. Modern devices have pregnancy-specific settings, humidifiers to combat nasal dryness, and nasal pillows designed for facial swelling. Studies show it lowers your risk of preeclampsia and gestational diabetes without harming the baby.
What’s the best pillow for sleep apnea during pregnancy?
A full-body pregnancy pillow that supports your belly, back, and legs is ideal. Look for one that helps you stay on your left side and keeps your head and neck aligned. Avoid stacking regular pillows under your head-it can worsen apnea. Wedge pillows that elevate your upper body 7-8 inches are also helpful for both apnea and reflux.
Can I treat reflux without medication?
Yes. Avoid eating within three hours of bedtime, skip spicy or fatty foods at night, and elevate your upper body with a wedge pillow-not just your head. Sleeping on your left side also helps. If you need extra help, Gaviscon Advance is a safe, non-absorbed antacid that forms a protective barrier in your stomach.
Will my sleep apnea go away after I have the baby?
It often improves, but not always. About half of women who develop sleep apnea during pregnancy still have symptoms after delivery. Some go on to develop chronic high blood pressure later. If you’re still snoring, tired, or waking up gasping after 12 weeks postpartum, get checked. Don’t assume it’s gone just because you’re no longer pregnant.
How soon should I start CPAP if I’m diagnosed?
The best time to start is between 24 and 28 weeks. Studies show starting CPAP during this window reduces preeclampsia risk by 30%. Waiting until after 30 weeks may reduce the benefit. If you’re diagnosed earlier, start as soon as possible-especially if you have other risk factors like obesity or high blood pressure.


14 Comments