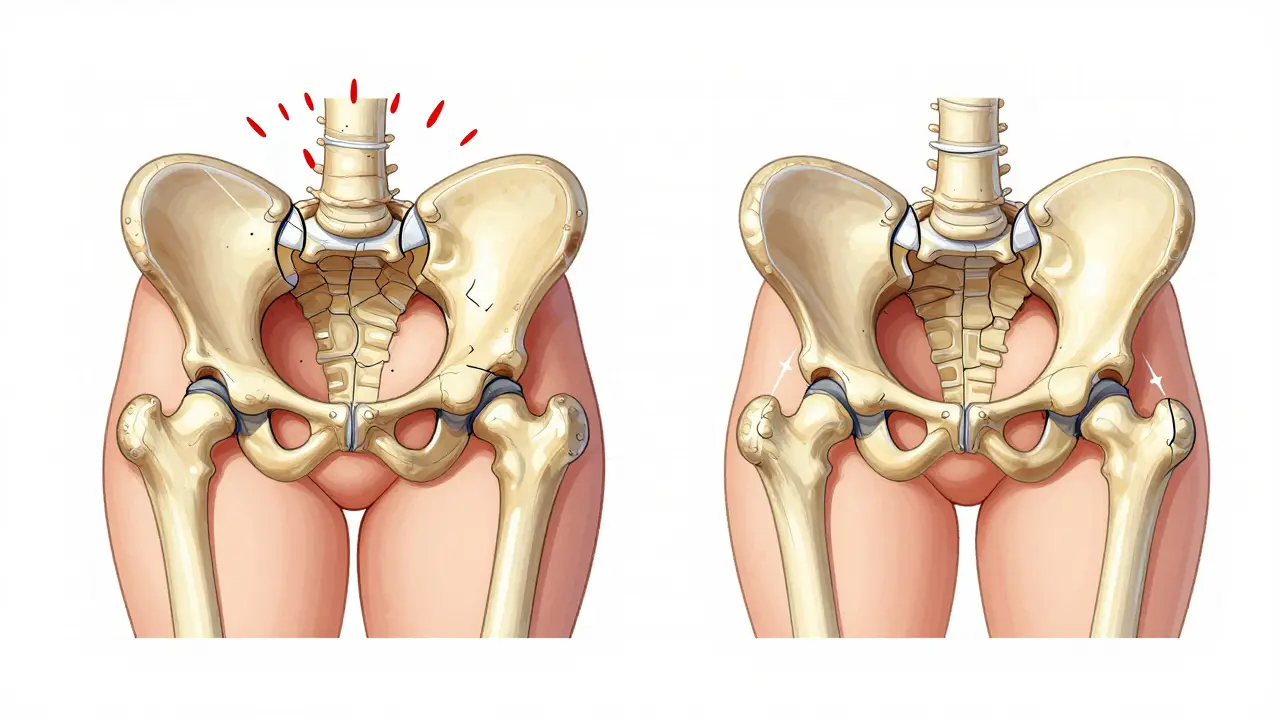
When your hip starts to ache with every step, it’s not just discomfort-it’s your body telling you something’s off. Osteoarthritis of the hip isn’t just aging. It’s wear and tear, inflammation, and cartilage breaking down. And for many people, especially those carrying extra weight, the problem isn’t just in the joint-it’s in the pounds. The good news? Losing weight isn’t just about looking better. For hip osteoarthritis, it can mean less pain, better movement, and even slowing down the damage.
Why Weight Matters So Much for Your Hip
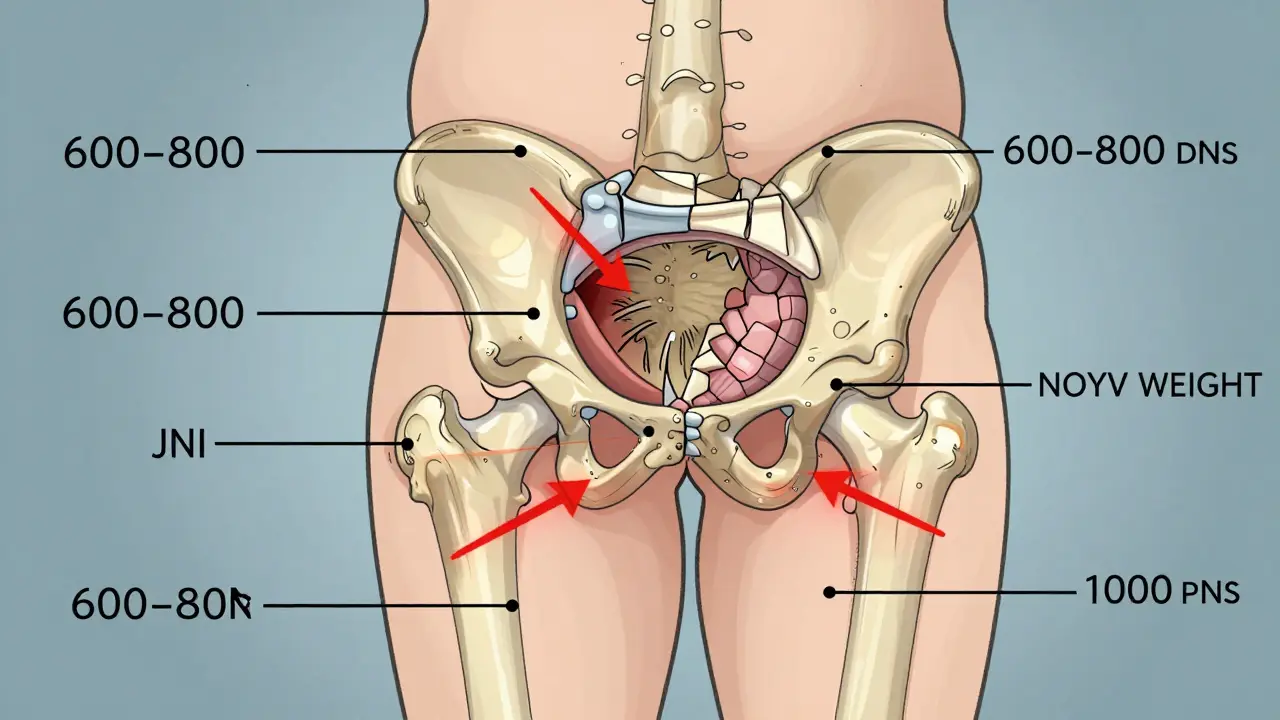
Your hip joint carries your whole body weight with every step. When you weigh 200 pounds, each step puts about 3 to 4 times that force on the joint. That’s 600 to 800 pounds of pressure. Now imagine doing that 5,000 times a day. Over years, that kind of stress wears down cartilage faster. Studies show that obesity increases your risk of developing hip osteoarthritis by up to 70% compared to people with a healthy weight.
But it’s not just mechanical. Fat tissue isn’t just storage-it’s active. It releases chemicals that cause inflammation. That inflammation doesn’t just make your hip hurt more-it actually speeds up the breakdown of cartilage. So even if you’re not overweight, excess body fat can still be working against your joints.
How Much Weight Do You Really Need to Lose?
You’ve probably heard that losing 5% of your body weight helps with joint pain. That’s true for knee osteoarthritis. But for the hip? The story’s different-and more powerful.
A major 2024 study published in Nature followed 65-year-old adults with hip osteoarthritis and obesity. The results showed that those who lost more than 10% of their body weight saw the biggest improvements-not just in pain, but in daily function, ability to move, and quality of life. The biggest jump? A 31% improvement in hip-related quality of life. That’s not a small gain. That’s going from struggling to get out of a chair to doing it without help.
And here’s the kicker: losing 5% helped. Losing 7% helped more. But losing 10% or more? That’s where the real changes happened. The study found a clear dose-response relationship: the more weight lost, the better the outcome. People who lost 15% or 20% didn’t do much better than those who lost 10%, suggesting that 10% is the sweet spot-not a target to rush past, but a goal worth reaching.
Why Hip OA Doesn’t Always Respond Like Knee OA
Here’s where things get confusing. If you search for weight loss and arthritis, you’ll see headlines screaming, “Lose Weight, Kill Knee Pain.” And it’s true-knee osteoarthritis responds strongly to even modest weight loss. But hip osteoarthritis? The evidence is mixed.
A 2023 clinical trial compared a very-low-calorie diet plus exercise to exercise alone in people with hip OA. After six months, there was no big difference in pain levels between the two groups. That led NEJM Journal Watch to publish a blunt take: “Osteoarthritis of the Hips Is Unaffected by Weight Loss.”
But wait. That same study followed people for a full year. At the 12-month mark, the group that lost weight showed clear improvements in pain, function, and overall hip condition. The benefits just took longer to show up.
Why the delay? The hip joint is deeper, more stable, and less directly loaded than the knee. It doesn’t get the same immediate mechanical relief from weight loss. But over time, as inflammation drops and muscle strength improves, the joint begins to heal. That’s why patience matters. This isn’t a quick fix. It’s a long-term reset.
What Actually Works: Diet, Movement, and Support
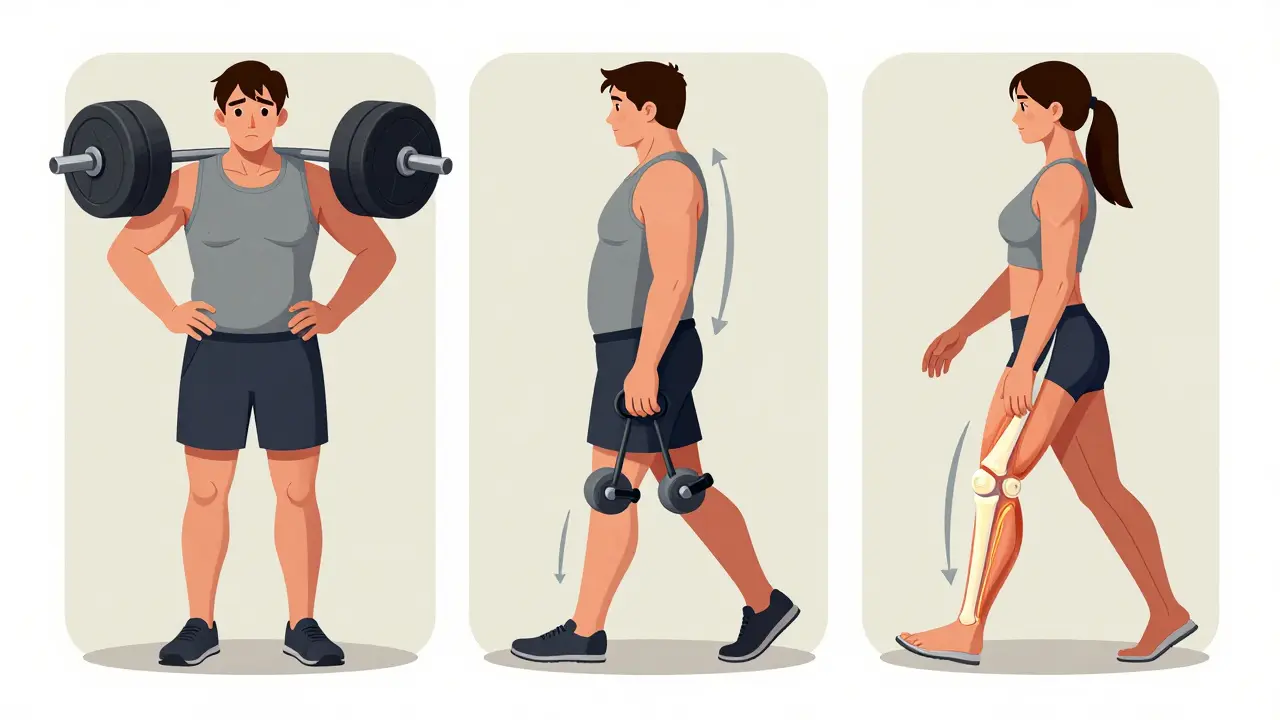
Weight loss alone won’t fix your hip. Neither will exercise alone. You need both-and you need structure.
The Osteoarthritis Healthy Weight For Life (OAHWFL) program, developed in Australia and New Zealand, combines weekly telehealth coaching, personalized meal plans, and targeted hip-strengthening exercises. Participants aim for 7-10% weight loss over 18 weeks. In studies, people who completed the program saw up to a 32% improvement in physical function, measured by the WOMAC index. That’s not just feeling better. That’s being able to walk to the store, climb stairs, or play with your grandkids again.
What kind of diet? Low-carbohydrate plans have shown strong results in reducing inflammation and helping people lose weight sustainably. But the key isn’t the diet name-it’s consistency. Cutting out sugary drinks, processed snacks, and oversized portions makes a bigger difference than any fad diet.
Exercise? Focus on low-impact movement: swimming, cycling, elliptical, and strength training for the glutes, quads, and core. Strong muscles around the hip act like shock absorbers. One study found that even 30 minutes of daily walking improved walking speed and reduced pain in people with hip OA.
When Weight Loss Isn’t Enough
Not everyone can lose 10% of their body weight. Some have mobility issues. Others have medical conditions that make dieting risky. That doesn’t mean you’re out of options.
Even a 3-5% weight loss can reduce pain enough to make daily life easier. And if you can’t lose weight, you can still build muscle. Stronger muscles mean less pressure on the joint. A 2022 study showed that people with hip OA who did 12 weeks of resistance training improved their pain and function as much as those who lost 8% of their weight.
Also, don’t overlook sleep and stress. Poor sleep raises inflammation. Chronic stress increases cortisol, which can make fat harder to lose and joints more sensitive to pain. Addressing these factors can make your weight loss efforts more effective-even if the scale doesn’t move fast.
What About Medications or Surgery?
There are FDA-approved weight loss medications for people with BMI over 30. But they’re not first-line. Guidelines from the American College of Rheumatology say to try lifestyle changes for at least six months before considering drugs. And surgery? Total hip replacement works well-but it’s not a cure. It’s a replacement. And if you’re still overweight after surgery, your new hip is under more stress. Studies show that people with obesity are more likely to need a second surgery within 10 years.
Weight loss before surgery improves outcomes. People who lose 10% before their operation recover faster, have fewer complications, and report higher satisfaction with their results.
Real People, Real Results
In Auckland, a 62-year-old woman named Margaret started the OAHWFL program after being told she’d need a hip replacement in two years. She weighed 98 kg with a BMI of 34. She lost 11 kg in 18 weeks-not by starving herself, but by eating more protein, cutting out late-night snacks, and walking 20 minutes a day. Her HOOS score jumped 22 points. Two years later, she hasn’t had surgery. She hikes on weekends. She says, “I didn’t just lose weight. I got my life back.”
Another man, 68, lost 15% of his body weight after a heart scare. He didn’t start for his hip-but his pain dropped from 8/10 to 2/10. He stopped using his cane. His doctor told him, “You’ve done more for your hip than any pill ever could.”
What You Can Do Today
You don’t need to run a marathon or go on a 1,000-calorie diet. Start small:
- Swap one sugary drink a day for water or unsweetened tea.
- Walk for 15 minutes after dinner-every day.
- Try one strength exercise for your hips: seated leg lifts or standing hip abductions. Do 10 reps, twice a day.
- Track your weight weekly, not daily. Focus on trends, not numbers.
- Ask your doctor about a referral to a dietitian or physiotherapist who specializes in osteoarthritis.
It’s not about perfection. It’s about progress. One less kilo today means one less kilo pressing on your hip tomorrow. And over time, that adds up to less pain, more movement, and more years on your own two feet.
What’s Next for Hip Osteoarthritis?
Researchers are now looking at personalized plans-tailoring diet and exercise based on body type, inflammation markers, and joint damage level. One study is testing whether combining intermittent fasting with hip-specific strength training gives better results than standard programs. Early results are promising.
What’s clear? Weight loss isn’t magic. But for hip osteoarthritis, it’s one of the few tools that actually changes the course of the disease-not just masking symptoms, but giving your joint a chance to heal.





9 Comments