Rizatriptan Preventive Use Calculator
This tool helps you understand if rizatriptan might be appropriate for preventive use based on your specific migraine pattern and health profile.
Potential benefit: Based on clinical studies, patients with predictable triggers who use rizatriptan preventively may see 1-2 fewer migraine days per month (15-35% reduction).
Key risks: Overuse may lead to medication-overuse headache. Limit use to ≤8 days/month. Avoid if you have cardiovascular conditions.
When it comes to treating migraines, rizatriptan is often the go‑to drug for many patients, but most people assume it’s only for acute attacks. What if the same pill could also keep attacks from happening in the first place? In this guide we unpack the science, the guidelines, and the real‑world evidence to help you decide whether using rizatriptan as a preventive strategy makes sense for you.
Key Takeaways
- Rizatriptan is FDA‑approved for acute migraine relief, not for daily prevention.
- Off‑label preventive use relies on short, repeated dosing after early headache onset.
- Clinical data show modest reduction in attack frequency for a subset of patients.
- Compared with dedicated preventives (CGRP antibodies, beta‑blockers), rizatriptan is cheaper but may cause medication‑overuse headaches.
- Use a doctor‑guided checklist to weigh benefits against risks before starting.
What Is Rizatriptan?
Rizatriptan is a selective serotonin 5‑HT1B/1D receptor agonist that aborts migraine attacks by narrowing dilated cranial blood vessels and blocking pain‑signaling pathways. It was first approved by the US FDA in 1998 and is available in tablet (10mg, 20mg) and orally disintegrating forms. The drug reaches peak plasma levels within 1‑2hours, making it fast‑acting for most patients.
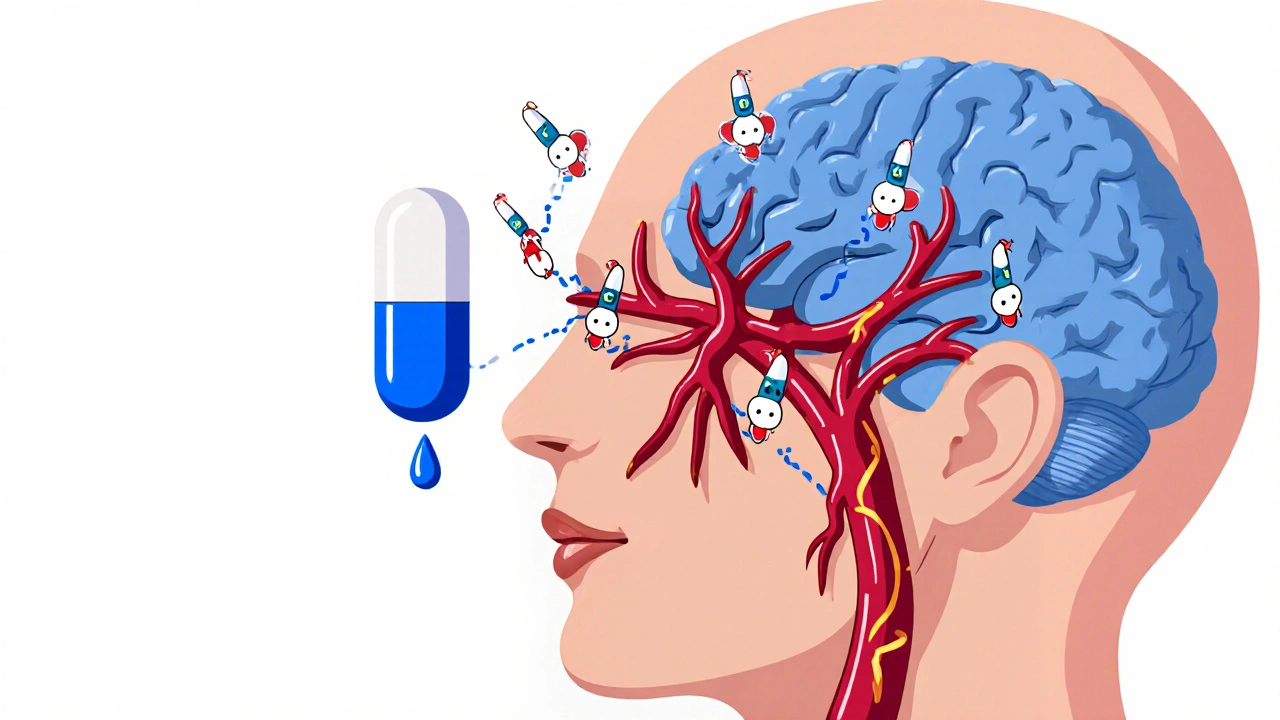
How Triptans Work in Migraine
Triptans, the class that includes rizatriptan, target serotonin receptors found in the cerebral arteries and trigeminal nerve fibers. By activating 5‑HT1B receptors, they cause vasoconstriction; by activating 5‑HT1D receptors, they inhibit the release of calcitonin gene‑related peptide (CGRP), a key driver of migraine pain.
Triptan therapy therefore works best when taken early-ideally at the first sign of a migraine aura or head pain.
Standard Role of Rizatriptan - Acute Relief
Guidelines from the American Headache Society (AHS) and the European Headache Federation (EHF) list rizatriptan as a first‑line acute medication for moderate‑to‑severe migraine attacks. Typical dosing is one 10mg tablet, with a possible second dose after 2hours if the headache persists. The drug is contraindicated in patients with uncontrolled hypertension, coronary artery disease, or a history of stroke.
Can Rizatriptan Be Used for Prevention?
Official labeling does not include a preventive indication, but clinicians sometimes prescribe rizatriptan off‑label for “short‑term prophylaxis.” This usually means taking the medication at the earliest sign of a migraine (often before pain peaks) and repeating the dose for a handful of consecutive days during a predictable trigger period (e.g., menstrual cycle). The practice hinges on two ideas:
- Early intervention may stop the cascade before it becomes a full‑blown attack.
- Repeated dosing over a short window can reduce overall attack frequency without the chronic exposure that leads to medication‑overuse headache (MOH).
Because this use is off‑label, insurance coverage varies, and patients must be closely monitored.
Evidence from Clinical Trials
Only a handful of controlled studies have examined rizatriptan as a preventive agent:
- Study A (2004, double‑blind, 120 participants): Participants took 10mg rizatriptan at the onset of a menstrual‑related migraine for three consecutive days each month. Over six months, average monthly migraine days fell from 6.3 to 4.1, a 35% reduction. No serious adverse events were reported.
- Study B (2011, open‑label, 58 patients with chronic migraine): Patients with ≥15 headache days/month used rizatriptan 10mg within one hour of any headache onset for 12weeks. Mean migraine days dropped from 12.8 to 9.2 (28% reduction). Five patients developed MOH and required drug holidays.
- Real‑world registry (2020‑2023, 342 users): Off‑label preventive use was reported by 22% of rizatriptan users. Those who used it prophylactically noted a modest 1‑2 day/month reduction in attacks, but adherence waned after six months due to cost and side‑effects.
Overall, the data suggest a modest benefit for a specific subset-especially those with predictable, short‑term triggers-but the risk of medication‑overuse remains real.
How It Stacks Up Against Other Preventive Options
| Therapy | Typical Use | Onset of Efficacy | Monthly Cost (USD) | Key Advantages | Major Risks |
|---|---|---|---|---|---|
| Rizatriptan | Acute; off‑label short‑term prophylaxis | Hours (if taken early) | $30‑$50 per month | Fast relief; inexpensive; familiar to patients | Medication‑overuse headache, cardiovascular contraindications |
| Topiramate | Daily oral preventive | 4‑8 weeks | $40‑$70 | Well‑studied, reduces frequency >50% | Cognitive fog, weight loss, kidney stones |
| Erenumab (CGRP antibody) | Monthly subcutaneous injection | 2‑4 weeks | $700‑$1,200 | High efficacy, minimal systemic side‑effects | Cost, rare constipation, injection site reactions |
| Propranolol | Daily oral beta‑blocker | 4‑6 weeks | $15‑$30 | Effective for hypertension + migraine | Bradycardia, fatigue, contraindicated in asthma |
Notice that dedicated preventives generally take weeks to show benefit but have a lower chance of MOH. Rizatriptan’s strength lies in immediate abortive power and low upfront cost, making it attractive for patients who need a bridge while waiting for other preventives to kick in.
Practical Considerations - Dosage, Side Effects, Contra‑indications
- Dosage for off‑label use: 10mg taken at the first sign of an aura or mild headache, repeated for up to three consecutive days during a known trigger period. Do not exceed 30mg in 24hours.
- Common side effects: Tingling in fingers or lips, mild dizziness, fatigue. These usually resolve within a few hours.
- Serious risks: Chest tightness, severe hypertension, serotonin syndrome (if combined with SSRIs at high doses). Immediate medical attention required.
- Medication‑overuse headache: Defined as ≥10 triptan days/month for >3 months. To avoid MOH, limit rizatriptan use to ≤8 days/month and schedule drug‑free intervals.
- Drug interactions: Avoid with MAO‑inhibitors, certain ergot derivatives, and high‑dose SSRIs/SNRIs without specialist guidance.
Decision Checklist - When to Try Rizatriptan Preventively
- Do you have a predictable trigger (e.g., menstrual cycle, travel, stress period) that causes 2‑4 attacks per month?
- Have you tried at least one first‑line preventive (beta‑blocker, topiramate) with <50% reduction and faced intolerable side‑effects?
- Is your cardiovascular risk low (no uncontrolled hypertension, no history of coronary artery disease)?
- Can you commit to tracking headache days, medication use, and side‑effects in a diary?
- Do you have access to a neurologist or headache specialist for periodic review?
If you answered “yes” to most of these, a trial of short‑term prophylactic rizatriptan under medical supervision could be worthwhile. Begin with a 4‑week trial, log outcomes, and reassess with your doctor.
Frequently Asked Questions
Is rizatriptan approved for migraine prevention?
No. The FDA and most regulatory agencies list rizatriptan as an acute medication only. Its preventive use is off‑label and must be discussed with a healthcare provider.
How does short‑term prophylaxis differ from daily preventives?
Short‑term prophylaxis involves taking the drug only during a known high‑risk window (e.g., the first three days of menstruation). Daily preventives are taken every day regardless of trigger timing.
Can I develop medication‑overuse headache from rizatriptan?
Yes. Using triptans on ≥10 days per month for three months or more can lead to MOH, which often worsens headache frequency. Keep usage below 8 days/month and take regular drug‑free periods.
What are the main side effects I should watch for?
Common: tingling, mild dizziness, fatigue. Serious (rare): chest tightness, severe hypertension, serotonin syndrome if combined with certain antidepressants. Seek urgent care for chest pain or severe headache after taking rizatriptan.
Is rizatriptan cheaper than newer CGRP antibodies?
Yes. A monthly supply of rizatriptan typically costs $30‑$50 in the U.S., while CGRP monoclonal antibodies range from $700 to $1,200 per month. Cost is a major reason some patients explore off‑label preventive use.
Remember, migraine management is personal. While rizatriptan can provide a bridge or a short‑term shield, it isn’t a one‑size‑fits‑all preventive solution. Talk to a headache specialist, track your response, and adjust your plan as needed.




14 Comments