Antidepressant Safety Calculator for Breastfeeding
Antidepressant Safety Calculator
This tool calculates the relative infant dose (RID) of antidepressants during breastfeeding based on medical research. RID shows the percentage of the mother's dose that transfers to breast milk.
Enter your medication and dose to see the relative infant dose.
When a new mother is struggling with postpartum depression, the decision to take medication isn’t just about feeling better-it’s about protecting her ability to care for her baby. Many women worry that antidepressants will harm their breastfeeding infant. But the truth is, untreated depression carries far greater risks to both mother and child than most medications do. The key is choosing the right drug, at the right dose, with the right monitoring.
Why Untreated PPD Is More Dangerous Than Medication
Postpartum depression affects about 1 in 8 new mothers. It’s not just sadness or fatigue. It’s a persistent low mood, loss of interest in the baby, trouble sleeping even when the baby is asleep, overwhelming guilt, and sometimes thoughts of harming yourself or the baby. Left untreated, PPD can lead to poor bonding, delayed infant development, and even long-term emotional and behavioral problems in children. The CDC, the American College of Obstetricians and Gynecologists (ACOG), and the American Academy of Pediatrics all agree: the harm of untreated depression outweighs the theoretical risk of medication in breast milk.How Antidepressants Enter Breast Milk
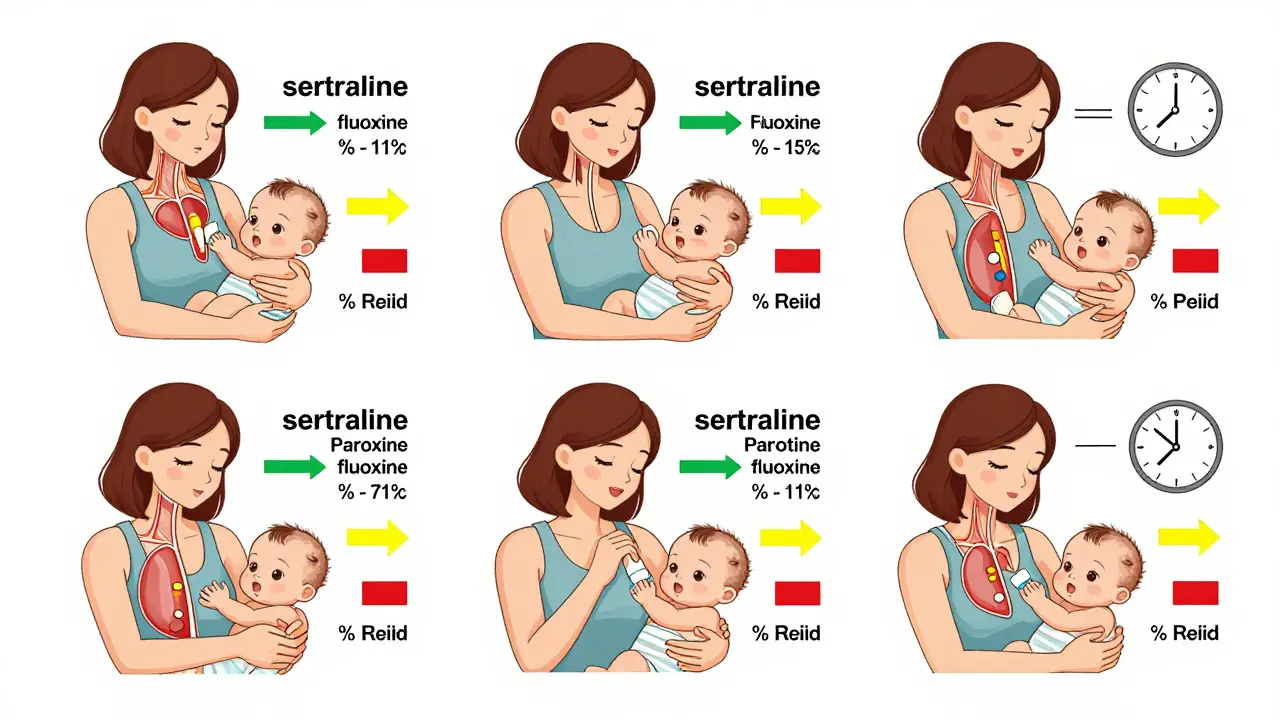
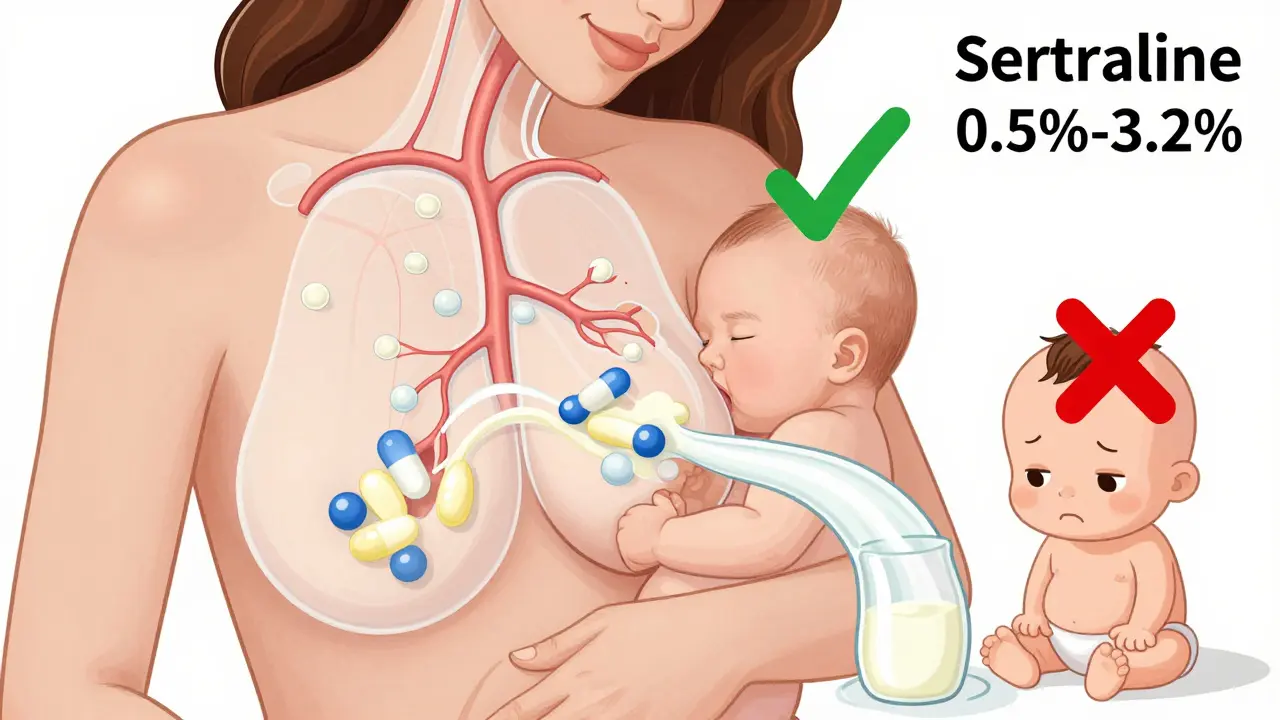
Not all antidepressants behave the same way in breast milk. The amount that reaches the baby depends on how well the drug passes from the mother’s bloodstream into her milk. This is measured as the relative infant dose (RID)-the percentage of the mother’s daily dose that the baby receives through milk. A RID under 10% is generally considered safe. Most SSRIs fall well below that.For example, sertraline transfers at only 0.5% to 3.2% of the mother’s dose. Paroxetine is similar, at 0.9% to 8.6%. That means even if a mother takes 100 mg of sertraline daily, her baby might get less than 3 mg-far below levels known to cause effects. In contrast, fluoxetine transfers at 5.9% to 15.2%, and its active metabolite, norfluoxetine, can build up in the baby’s system over time, especially if the baby is under 2 months old.
Which Antidepressants Are Safest During Lactation?
Based on decades of research and real-world data, here’s the current safety ranking for antidepressants during breastfeeding:- Sertraline - First choice. Lowest transfer, minimal infant effects. Used in over 90% of breastfeeding mothers on antidepressants. Infant serum levels are often undetectable.
- Paroxetine - Very similar to sertraline. Slightly higher transfer but still safe. May be preferred if the mother has anxiety alongside depression.
- Citalopram - Moderate transfer (3.5-8.9%). Avoid doses above 20 mg/day due to potential QT prolongation risk in infants.
- Escitalopram - Limited data, but expected to be similar to citalopram. Use with caution.
- Venlafaxine - Transfer is low (1.4-5.9%), but higher maternal doses (over 150 mg/day) have been linked to infant irritability and poor feeding.
- Mirtazapine - Limited data. May cause drowsiness in infants. Use only if other options fail.
- Fluoxetine - Avoid if possible. High transfer and long half-life. Can cause jitteriness, poor feeding, or sleep issues in newborns.
- Bupropion - Theoretical risk of seizures in infants. Avoid unless no other option exists.
- Doxepin - Avoid completely. Documented cases of infant apnea and cyanosis at low maternal doses.
Tricyclic antidepressants like amitriptyline also have low transfer due to high protein binding, making them a reasonable alternative if SSRIs don’t work. But SSRIs remain the standard because they’re easier to tolerate and have more safety data.
New Treatments: Zuranolone and What We Know
In August 2023, the FDA approved zuranolone (Zurzuvae) as the first oral medication specifically for postpartum depression. It works faster than traditional antidepressants-some women see improvement in as little as 3 days. But here’s the catch: clinical trials required women to stop breastfeeding during treatment. The manufacturer’s label says there’s no data on its presence in breast milk.Still, LactMed (a trusted NIH database) estimates the infant exposure is only 0.5% to 1.5% of the maternal dose-lower than many SSRIs. Experts suggest it’s unlikely to cause harm, but caution remains. The ACOG currently recommends pumping and discarding milk for one week after the last dose. That’s not because zuranolone is dangerous, but because we simply don’t have enough real-world data yet.
What Do Real Mothers Experience?
A 2021 survey of 347 breastfeeding mothers with PPD found that 78% took antidepressants, and 86% reported no noticeable effects on their babies. But 12% did notice changes: fussiness, trouble sleeping, or feeding issues. One mother on Reddit wrote: “My baby turned into a screaming mess after I started fluoxetine. Switched to sertraline-calm baby in 48 hours.” Another shared: “I thought I was failing as a mom until I realized my anxiety was making me feel like I couldn’t bond. Sertraline didn’t fix everything, but it gave me back the ability to hold my baby without crying.”On the other hand, some women stop medication because they believe their baby is reacting-even when there’s no medical evidence. That’s why monitoring matters. Don’t assume every cry or sleepless night is caused by the drug. Babies are unpredictable. But if you notice sudden lethargy, poor feeding, or unusual irritability within the first two weeks of starting a new antidepressant, talk to your doctor.
How to Take Antidepressants Safely While Breastfeeding
If you and your provider decide medication is the right path, here’s how to minimize risk:- Start low - Begin with the lowest effective dose. For sertraline, that’s often 25-50 mg/day. For paroxetine, 10-20 mg/day.
- Time your doses - Take your pill right after a feeding, not before. This gives your body time to metabolize the drug before the next nursing session.
- Watch for signs - Look for excessive sleepiness, poor feeding, unusual crying, or rash in the first 2-4 weeks.
- Don’t rush to quit - It takes 3-4 weeks for antidepressants to work. Stopping too soon increases your risk of relapse by three times.
- Use trusted resources - LactMed (from the National Library of Medicine) updates daily and is free. The InfantRisk Center hotline (806-352-2519) answers questions from clinicians and mothers daily.
What About Long-Term Effects?
Right now, we don’t have solid data on whether antidepressants taken during breastfeeding affect a child’s brain development years later. A major study called B.R.I.D.G.E. is tracking 500 infants whose mothers took SSRIs while breastfeeding. They’ll check development at 6, 12, and 24 months. Preliminary results are expected in late 2024.One emerging area is pharmacogenomics. A 2022 study in JAMA Pediatrics found that babies with a specific gene variant (CYP2D6 poor metabolizer) had over three times higher levels of venlafaxine in their blood. That means some infants are naturally more sensitive. In the future, genetic testing might help personalize treatment-but it’s not standard yet.
Screening and Support Matter Too
The American Academy of Pediatrics recommends screening for depression at every well-baby visit: at 1, 2, 4, and 6 months. If a mother scores 13 or higher on the Edinburgh Postnatal Depression Scale, she should be referred for treatment. But screening alone isn’t enough. Support matters. Therapy, peer groups, and partner involvement are just as important as medication. Many women recover faster when they combine medication with counseling or support groups like Postpartum Support International.Final Thoughts: You’re Not Choosing Between Baby and You
There’s a dangerous myth that taking antidepressants while breastfeeding means you’re harming your child. The science says the opposite. You’re not choosing between your mental health and your baby-you’re choosing to be the mother your child needs. A mother who can sleep, eat, and hold her baby without panic is a mother who can nurture. A mother who’s treated for depression is more likely to continue breastfeeding longer, respond to her baby’s cues, and build a secure attachment.If you’re struggling, don’t wait. Talk to your OB, your pediatrician, or a mental health provider who specializes in perinatal care. There’s no shame in needing help. And there’s no reason to suffer in silence while your baby watches you fade away. You’re not broken. You’re healing. And with the right support, you’ll get back to the mother you know you are.
Can I breastfeed while taking sertraline?
Yes, sertraline is one of the safest antidepressants to take while breastfeeding. It transfers in very low amounts into breast milk-usually less than 3% of the mother’s dose. Most infants show no detectable levels in their blood, and studies have found no increased risk of developmental delays, feeding problems, or behavioral issues. It’s the most commonly prescribed antidepressant for breastfeeding mothers.
What if my baby seems fussy after I start an antidepressant?
Fussiness alone doesn’t mean the medication is the cause. Newborns go through normal developmental changes that can affect sleep and crying patterns. But if the fussiness started right after you began the medication and is severe, talk to your provider. They may suggest switching to a different drug (like switching from fluoxetine to sertraline) or adjusting your dose. Never stop medication without medical guidance-sudden discontinuation can cause withdrawal symptoms in both you and your baby.
Is it safe to take antidepressants right after giving birth?
Yes. Many women begin treatment within days of delivery, especially if symptoms are severe. The first two weeks after birth are the highest risk period for both PPD onset and infant sensitivity to medication. That’s why doctors recommend starting with the lowest possible dose and monitoring closely. If your baby is full-term and healthy, the risk is very low. Premature or medically fragile infants may need more caution, but treatment is still usually recommended.
Why is fluoxetine not recommended during breastfeeding?
Fluoxetine has a very long half-life-both in the mother and the infant. Its active metabolite, norfluoxetine, builds up over time and can reach levels in the baby’s blood up to 30% of the mother’s concentration. This increases the risk of side effects like irritability, poor feeding, and sleep disruption, especially in newborns. While not every baby is affected, the data shows a higher rate of issues compared to sertraline or paroxetine, so it’s not a first-line choice during lactation.
Can I take zuranolone while breastfeeding?
The FDA-approved label for zuranolone does not recommend breastfeeding during treatment due to lack of data. However, early estimates from LactMed suggest the amount passed into milk is very low (0.5-1.5% of maternal dose), and experts believe it’s unlikely to cause harm. Some providers may allow its use with close monitoring and pumping/discarding milk for one week after the last dose. Always follow your doctor’s guidance-this is a new medication, and recommendations may change as more data becomes available.



15 Comments