Elderly Renal Dosing Calculator
When you’re over 65 and your kidneys aren’t working like they used to, even a normal dose of a common medication can become dangerous. It’s not about taking too much-it’s about your body not clearing it the way it should. About 38% of adults 65 and older have moderate to severe kidney impairment, and many of them are on medications that can build up to toxic levels if not adjusted properly. This isn’t rare. It’s happening every day in homes, nursing facilities, and hospitals-and it’s often preventable.
Why Kidney Function Matters More After 65
Your kidneys don’t just filter waste. They handle the cleanup of over 70% of commonly prescribed drugs. As you age, kidney function naturally declines. Glomerular filtration rate (GFR), which measures how well your kidneys filter blood, drops by about 1% per year after age 40. By 70, many people have a GFR below 60 mL/min/1.73 m²-the official cutoff for chronic kidney disease (CKD) stage 3. But here’s the problem: doctors often don’t test for it. Or worse, they assume a normal creatinine level means normal kidney function. That’s a mistake. Serum creatinine, the standard blood test used to estimate kidney function, can be misleading in older adults. Muscle mass decreases with age, so even if creatinine looks fine, kidney function may be significantly reduced. That’s why relying only on creatinine leads to underestimating kidney problems in nearly 20% of elderly patients.How to Measure Kidney Function Accurately
There are two main equations doctors use to estimate kidney function: Cockcroft-Gault and MDRD. The Cockcroft-Gault equation, created in 1976, uses age, weight, sex, and serum creatinine to calculate creatinine clearance (CrCl). It’s the go-to for dosing adjustments because it estimates actual drug clearance, not just filtration. For men: [(140 - age) × weight in kg] ÷ (72 × serum creatinine). For women, multiply that result by 0.85. The MDRD equation estimates GFR and is better for population studies, but it’s less reliable for dosing decisions in older adults. Why? It doesn’t account for muscle mass changes. A 2013 study in BMC Nephrology showed Cockcroft-Gault often underestimates kidney function by 15-20% in the elderly-but that’s actually safer when dosing medications. Underestimating kidney function means you’re more likely to reduce the dose, which reduces risk. For patients with borderline kidney function (GFR between 25-59 mL/min/1.73 m²), guidelines from KDIGO recommend using Cockcroft-Gault as the primary tool. If the result is close to a dosing threshold-say, 29 vs. 30 mL/min-use MDRD to confirm. And for those with normal or near-normal creatinine but suspected kidney issues, cystatin C-based equations are more accurate. Cystatin C isn’t affected by muscle mass, making it ideal for older adults.Medications That Require Dose Changes
Not all drugs are created equal. Some are safe at any kidney function. Others? They’re time bombs if not adjusted. Metformin is a classic example. In the U.S., it’s banned if serum creatinine exceeds 1.5 mg/dL in men or 1.4 mg/dL in women. But European guidelines are more flexible. The key is knowing your CrCl. If it’s below 30 mL/min, metformin should be stopped. If it’s between 30-45 mL/min, use the lowest effective dose and check kidney function every 3 months. Digoxin is another high-risk drug. Its therapeutic range is narrow: 0.8-2.0 ng/mL. Too little, and it doesn’t help your heart. Too much, and you get nausea, confusion, or dangerous heart rhythms. In elderly patients with renal impairment, levels should be checked 15-20 days after starting or changing the dose-not 5-7 days like in younger people. Why? It takes longer for digoxin to reach steady state when kidneys are slow. Lithium, used for bipolar disorder, is even trickier. The safe range is 0.6-0.8 mmol/L for long-term use. But if kidney function drops below 30 mL/min, lithium can accumulate fast. Many patients on lithium need monthly blood tests if they’re over 70 and have reduced kidney function. Antibiotics like cefepime and ciprofloxacin also need attention. For cefepime, the standard dose is 1g every 6 hours. But if CrCl is 30-50 mL/min, drop to every 8 hours. If CrCl is below 10 mL/min, give it only once a day. Miss this, and you risk seizures or brain toxicity. Allopurinol, used for gout, can cause life-threatening skin reactions if not dosed properly. In patients with GFR under 10 mL/min, start with 100 mg every other day. Never start at full dose.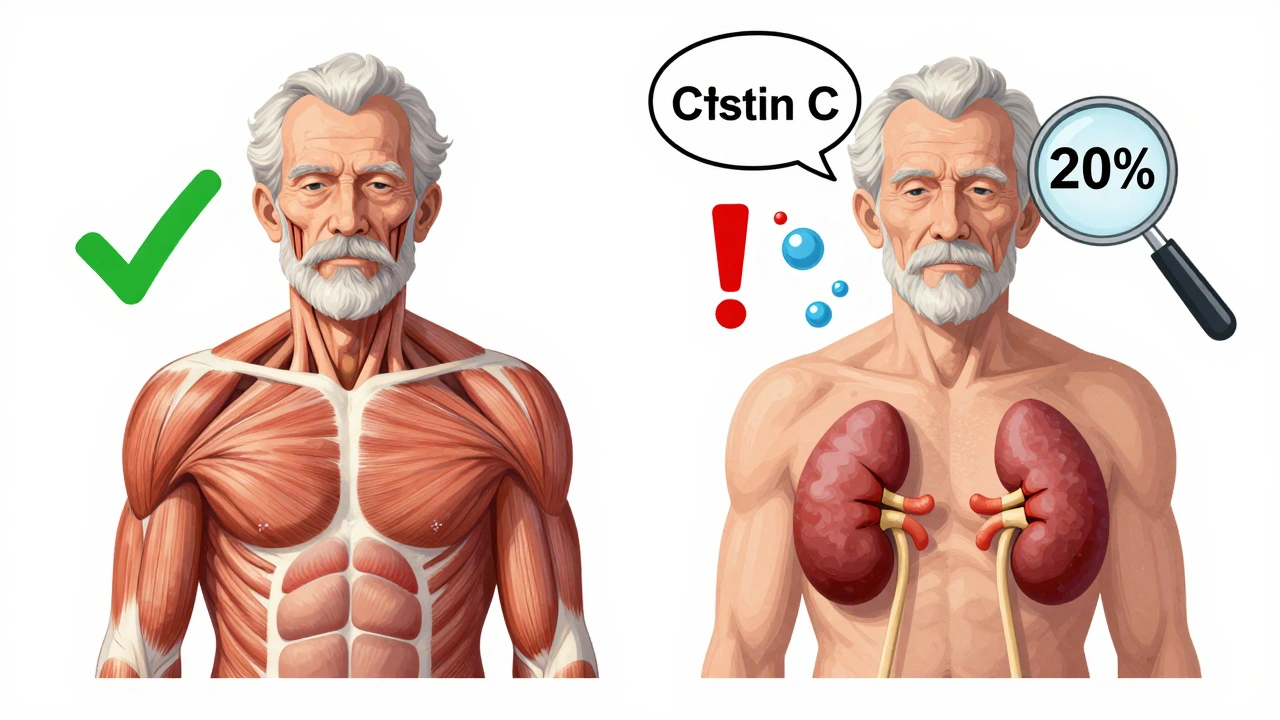
The 50% Rule-And Why It Fails
Many clinicians use a simple trick: if a drug is more than 50% cleared by the kidneys, cut the dose in half when CrCl drops below 50 mL/min. It’s easy. It’s quick. And it’s wrong for many drugs. Gabapentin is a prime example. The 50% rule would suggest halving the dose when CrCl is below 50 mL/min. But gabapentin is almost entirely cleared by the kidneys, and its clearance drops nonlinearly. The correct approach? Reduce the dose by 75% when CrCl is below 30 mL/min. A 2015 study found that 68% of prescribers got gabapentin dosing wrong in elderly patients. Vancomycin is another trap. It’s dosed by interval extension, not dose reduction. If CrCl is low, you give the same dose but less often-every 48 hours instead of every 12. If you just reduce the dose, you risk underdosing and treatment failure. The bottom line: don’t guess. Check the drug’s specific guidelines. Use resources like the University of Nebraska Medical Center’s antimicrobial dosing tables or the KDIGO Drug Dosing Report.What Works in Real Clinics
Knowing what to do is one thing. Doing it consistently is another. A 2015 study found that only 43.7% of doctors routinely adjusted doses for elderly patients with kidney impairment. The biggest mistakes? Gabapentin, rivaroxaban, and allopurinol. The fix? Systems, not just knowledge. At the University of Nebraska Medical Center, they added automated alerts to their electronic health record. When a doctor ordered cefepime for a patient with CrCl under 30 mL/min, the system popped up: “Dose adjustment recommended: 1g every 12 hours.” Within a year, inappropriate dosing dropped by 37.2%. The Mayo Clinic took it further. They assigned clinical pharmacists to review all medication regimens for patients over 65 with kidney disease. Result? A 58% drop in adverse drug events. Mobile apps like Epocrates Renal Dosing (used over 1.2 million times) and integrated EHR calculators have cut dosing errors by 41%, according to a 2022 study in the American Journal of Health-System Pharmacy.New Tools and Future Directions
In 2023, the FDA approved the first AI-powered dosing tool called DoseOptima. It pulls real-time lab values, age, weight, and drug lists to recommend precise doses. In a trial of 15,000 patients, it was 92.4% accurate. KDIGO is updating its guidelines to recommend cystatin C as the preferred test for elderly patients. That’s a big shift-because creatinine alone just doesn’t cut it anymore. The American Society of Health-System Pharmacists is working on a national standard for renal dosing across 150 high-risk drugs. Expected by the end of 2023, this will help unify confusing guidelines. And research is moving into genetics. The NIH is studying how gene variants affect how elderly patients clear drugs. In the future, your DNA might tell your doctor exactly how much of a drug you need.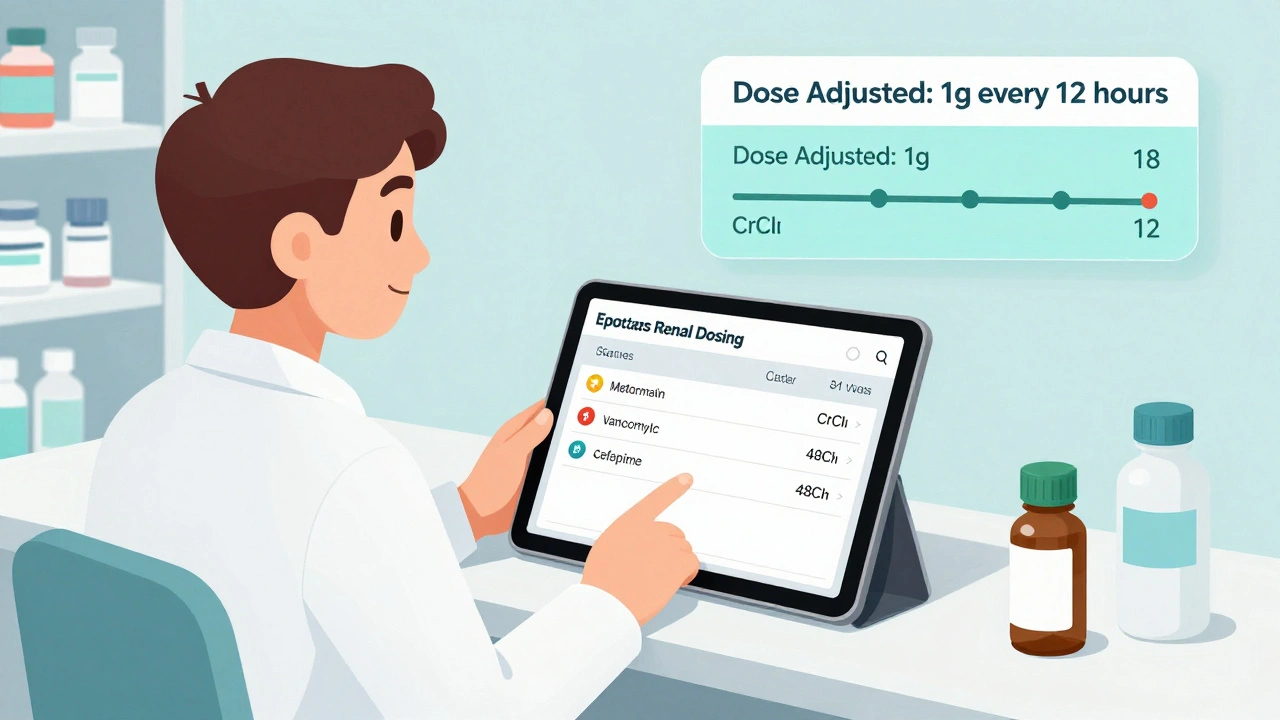
What You Can Do Right Now
If you or a loved one is over 65 and on any medication:- Ask for a CrCl calculation-not just a creatinine level.
- Make a list of all medications, including over-the-counter and supplements.
- Ask the pharmacist: “Which of these need dose changes because of kidney function?”
- Request a medication review every 6 months if you have kidney disease.
- Watch for signs of toxicity: confusion, dizziness, nausea, muscle weakness, or unusual fatigue.
Why This Isn’t Just a Doctor’s Problem
Hospitals are penalized financially if patients have drug-related adverse events. Medicare can take away up to 1% of payments-about $17,000 per bed per year. That’s why big hospitals are investing in systems. But nursing homes? Only 28% have formal renal dosing protocols. This isn’t just about saving money. It’s about saving lives. The Institute for Safe Medication Practices estimates that proper renal dosing could prevent 115,000 adverse drug events each year in the U.S.-and save $1.27 billion. The tools exist. The guidelines are clear. The data is there. What’s missing is consistent action. Every time a dose isn’t adjusted, someone is at risk. And in the elderly, that risk is never small.How do I know if my elderly parent needs a medication dose adjustment?
Start by asking for a creatinine clearance (CrCl) calculation using the Cockcroft-Gault formula. If their CrCl is below 60 mL/min, any medication cleared by the kidneys should be reviewed. High-risk drugs include gabapentin, metformin, digoxin, lithium, and certain antibiotics. If they’ve had recent falls, confusion, or nausea, it could be a sign of drug buildup. Always ask the pharmacist or doctor to review all medications for kidney-related dosing.
Is it safe to keep taking metformin if I have kidney problems?
It depends on your kidney function. In the U.S., metformin is not recommended if serum creatinine is above 1.5 mg/dL in men or 1.4 mg/dL in women. But the better measure is CrCl. If your CrCl is below 30 mL/min, stop metformin. Between 30-45 mL/min, you can use it at the lowest dose with monthly kidney checks. Never assume a normal creatinine means normal kidney function-especially in older adults.
Why do some drugs need interval changes instead of dose reductions?
Some drugs, like vancomycin and certain antibiotics, need to stay at a certain concentration in the blood to work. Reducing the dose too much can make them ineffective. Instead, you keep the same dose but give it less often-like every 48 hours instead of every 12. This lets the drug build up slowly and stay in the therapeutic range without causing toxicity.
Can over-the-counter painkillers harm elderly kidneys?
Yes. NSAIDs like ibuprofen and naproxen reduce blood flow to the kidneys and can cause sudden kidney injury, especially in older adults with existing kidney problems. Acetaminophen is generally safer, but even that can be risky if taken in high doses over time. Always check with a pharmacist before using OTC pain relievers if you’re over 65 or have kidney disease.
Are there apps or tools that help with kidney dosing?
Yes. Epocrates Renal Dosing is used by over a million clinicians and gives quick, evidence-based dosing for hundreds of drugs. Many electronic health records now include built-in calculators that auto-adjust doses based on lab values. These tools reduce errors by up to 41%. If you’re a caregiver, ask the pharmacist to show you how to use one.







15 Comments