It’s 2 a.m. again. You’ve tried counting sheep, scrolling through calming videos, even sipping chamomile tea-but your mind won’t shut off. So you reach for that bottle of OTC sleep aid you’ve had in the cabinet since last year. It’s easy. It’s available without a prescription. And it worked… once. But what happens when you start relying on it? And is it really helping, or just masking a bigger problem?
Over-the-counter sleep aids are everywhere. From pharmacy shelves to Amazon bestsellers, products like Benadryl, Unisom, and melatonin gummies promise quick relief for sleepless nights. In 2023, Americans spent over $600 million on these products. But here’s the truth most labels won’t tell you: these aren’t cures. They’re temporary fixes with hidden risks-and for many people, they make sleep worse in the long run.
What’s Actually in OTC Sleep Aids?
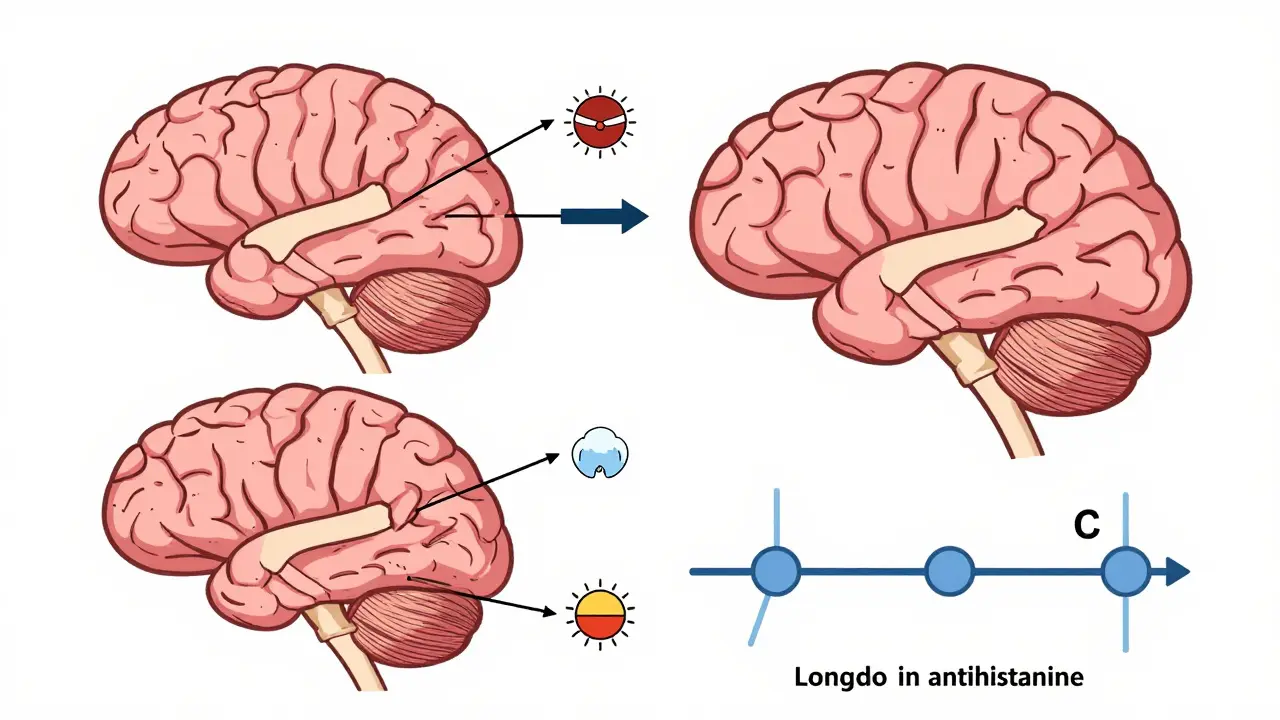
Not all sleep aids are the same. There are two main types: antihistamines and supplements. The most common antihistamines are diphenhydramine and a first-generation antihistamine used in products like Benadryl, Sominex, and Nytol, typically dosed at 25-50 mg per tablet, and doxylaminea stronger antihistamine found in Unisom SleepTabs, usually at 25 mg per dose. These drugs were originally designed for allergies. Their sleepiness effect is a side effect-not their main purpose.
The other group is supplements. melatonina hormone naturally produced by the body to regulate sleep-wake cycles, available as a supplement in doses ranging from 0.5 mg to 10 mg is the most popular. Then there are herbal options like valerian rootan herbal supplement often marketed for sleep, with inconsistent evidence of effectiveness and chamomilea mild herbal tea or capsule often used for relaxation, with minimal clinical support for treating insomnia.
Here’s the catch: melatonin supplements aren’t regulated like drugs. A 2017 study in the Journal of Clinical Sleep Medicine tested 31 products and found that the actual melatonin content ranged from 83% less to 478% more than what was on the label. That means you could be taking almost nothing-or way too much-without knowing it.
How Effective Are They Really?
Let’s get real: OTC sleep aids don’t work like magic. The American Academy of Sleep Medicine reviewed decades of research and concluded in 2017 that there’s insufficient evidence to support using antihistamines or herbal supplements for chronic insomnia. That’s not a minor opinion-it’s a formal guideline.
Studies show that diphenhydramine and doxylamine might help you fall asleep 3 to 13 minutes faster than a placebo. They might add 20 to 60 minutes of sleep total. That’s not a full night’s rest. That’s barely enough to feel slightly less tired the next day.
Melatonin works best for specific cases: jet lag, shift work, or delayed sleep phase. For most people with general insomnia, it barely moves the needle. A 2022 systematic review found that melatonin reduced time to fall asleep by only 7 minutes on average.
And here’s something most users don’t realize: if you use these every night, your body may start to rely on them. About 25% of people who take OTC sleep aids daily for more than 10 days develop tolerance. That means you need more to get the same effect. And when you stop? Around 30% experience rebound insomnia-sleep that’s worse than before you started.
The Hidden Side Effects You’re Not Being Told About
Antihistamine-based sleep aids don’t just make you sleepy. They shut down other systems in your body too. These drugs belong to a class called anticholinergics, which block acetylcholine-a brain chemical critical for memory, focus, and muscle control.
Common side effects include:
- Dry mouth (32% of users)
- Blurred vision (18%)
- Constipation (24%)
- Urinary retention (especially risky for men with enlarged prostates)
- Confusion and dizziness (much more common in people over 65)
And the long-term risks? Scary. A 2015 study in JAMA Internal Medicine followed over 3,400 people for more than 7 years. Those who took anticholinergic drugs regularly had a 54% higher risk of developing dementia. That’s not a small increase. That’s a red flag.
Melatonin seems safer-but it’s not harmless. Common complaints include:
- Daytime drowsiness (45% of users)
- Vivid dreams or nightmares (68%)
- Headaches (31%)
- Nausea and vomiting (up to 19%)
- Dizziness (28%)
- Bedwetting in children (8%)
The NHS warns that melatonin can cause unexplained pain in arms or legs. If that happens, stop taking it. Don’t wait.
And if you have sleep apnea? Don’t use OTC sleep aids at all. They relax throat muscles, which can make breathing interruptions worse. That’s not just disruptive-it’s dangerous.
Who Should Avoid These Products Completely?
Some people shouldn’t touch OTC sleep aids. Period.
Adults over 65: The Beers Criteria (updated in 2023) lists diphenhydramine and doxylamine as potentially inappropriate medications for older adults. Why? They increase the risk of falls by 50% and raise the chance of confusion or memory problems by 60%. One fall can change your life.
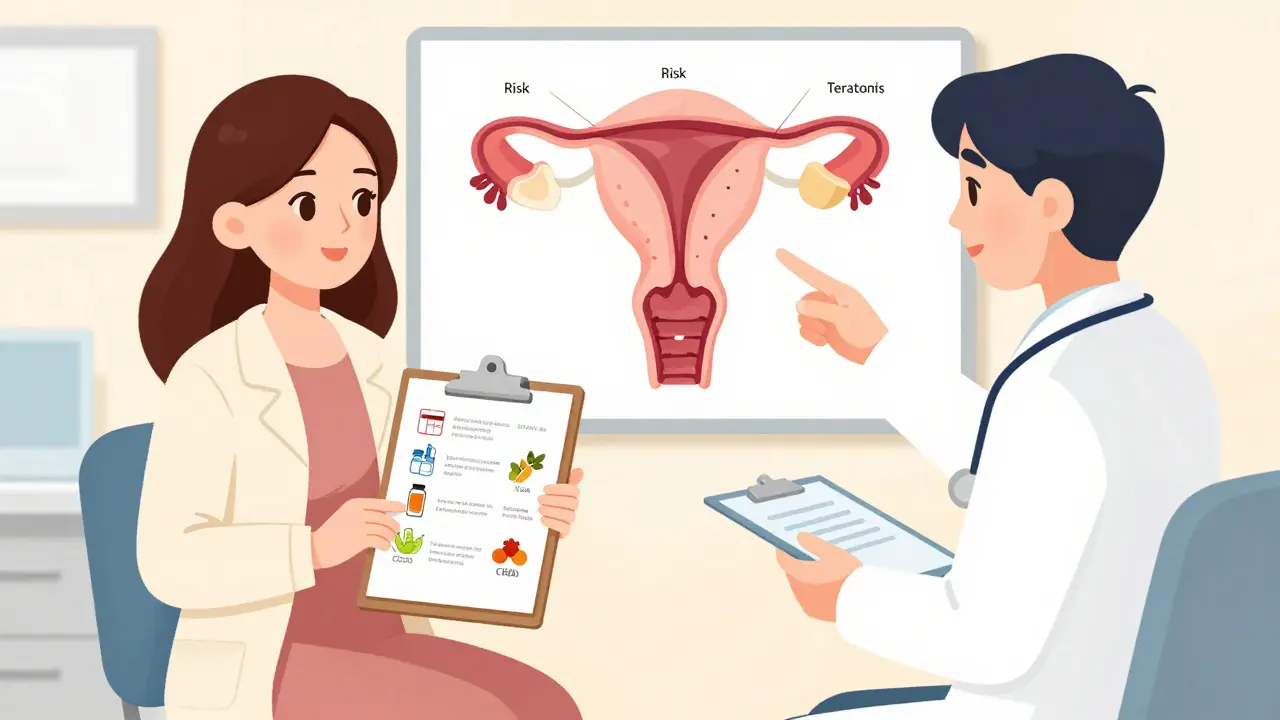
Pregnant or breastfeeding women: The FDA says diphenhydramine is Category B-no proven harm, but not enough data to say it’s safe. Melatonin? Almost no safety data in pregnancy. The NIH’s LactMed database advises caution. If you’re expecting, talk to your doctor before taking anything.
People with chronic health conditions: If you have glaucoma, prostate issues, liver disease, or epilepsy, antihistamines can make things worse. Even if you’ve taken them before, your body changes as you age or as your health shifts.
How Long Is Too Long?
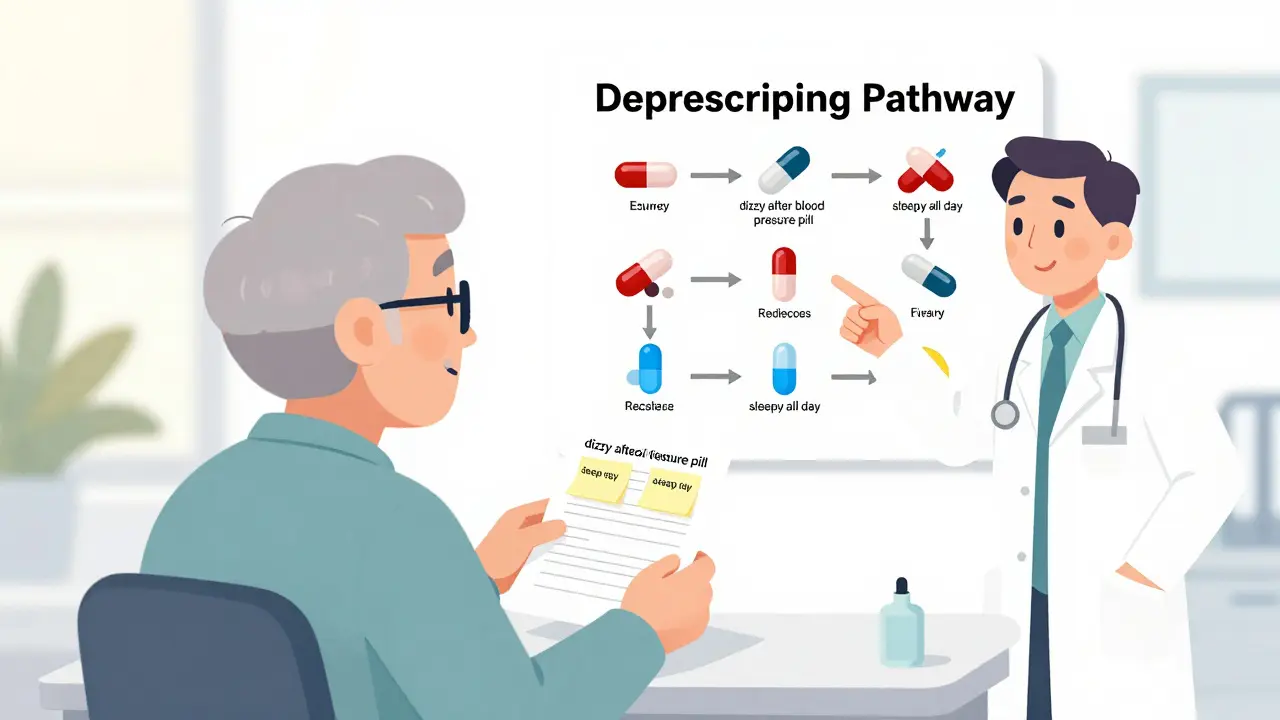
The FDA says: don’t use antihistamine sleep aids for more than two weeks. The Cleveland Clinic says the same. The Sleep Foundation says: if you’ve been using them for more than 10 days straight, you might be building tolerance.
But here’s the problem: a 2022 survey found that 38% of users go beyond two weeks. Nearly 1 in 5 use them for over a month. That’s not occasional use. That’s dependency.
And melatonin? The European Food Safety Authority says 1 mg is enough for most adults. Yet most bottles sell 3 mg, 5 mg, or even 10 mg. You don’t need more to sleep better-you just need to avoid the side effects.
Start low. Use it only when you need it. Not every night. Not for weeks on end.

What Should You Do Instead?
The best treatment for chronic insomnia isn’t a pill. It’s Cognitive Behavioral Therapy for Insomnia (CBT-I)a structured, non-drug therapy that changes thought patterns and behaviors around sleep, with success rates of 70-80%. It’s recommended as the first-line treatment by the American Academy of Sleep Medicine. And it works better than any OTC sleep aid.
CBT-I teaches you how to:
- Stop racing thoughts before bed
- Use your bed only for sleep and sex
- Reset your internal clock with consistent wake-up times
- Reduce anxiety around not sleeping
Studies show 70-80% of people who complete CBT-I see lasting improvements. No side effects. No dependency. Just better sleep.
Even simple changes help: no screens an hour before bed. Keeping your bedroom cool and dark. Avoiding caffeine after 2 p.m. Getting sunlight in the morning. These aren’t trendy tips-they’re science-backed.
Final Advice: Use Wisely, or Don’t Use at All
OTC sleep aids aren’t evil. Sometimes, they help. If you’re flying across time zones, a low dose of melatonin might reset your rhythm. If you’re going through a stressful week and can’t sleep, a single night of diphenhydramine might get you through.
But if you’re using them because you’ve been lying awake for months? That’s not a sleep problem. That’s a signal.
Your body isn’t broken. It’s trying to tell you something. Stress. Anxiety. Poor sleep habits. An undiagnosed condition. OTC sleep aids don’t fix those. They just mute the message.
If you’ve been using OTC sleep aids for more than two weeks, it’s time to talk to someone. A doctor. A sleep specialist. Even a therapist trained in CBT-I. You don’t need to suffer through another sleepless night. There are better ways. And they don’t come in a bottle.
Are OTC sleep aids safe for long-term use?
No. OTC sleep aids like diphenhydramine and doxylamine are not meant for long-term use. Using them for more than two weeks increases the risk of side effects like confusion, dizziness, urinary retention, and constipation. Long-term use of antihistamines has been linked to a 54% higher risk of dementia. Melatonin may seem safer, but daily use for months can lead to tolerance, rebound insomnia, and disrupted natural hormone cycles. Medical guidelines recommend using these products only occasionally and for no longer than 7-10 days.
Which is safer: diphenhydramine or melatonin?
For short-term, occasional use, melatonin is generally safer than diphenhydramine. Melatonin doesn’t cause anticholinergic side effects like dry mouth, blurred vision, or cognitive decline. However, melatonin supplements vary widely in dosage and purity, and high doses (above 5 mg) can cause vivid dreams, dizziness, nausea, and next-day grogginess. Diphenhydramine carries more serious risks, especially for older adults, including increased fall risk and dementia. Neither is ideal for regular use, but melatonin has fewer long-term dangers.
Can OTC sleep aids cause dependence?
Yes. While OTC sleep aids aren’t addictive like prescription sleeping pills, they can create psychological dependence. People start believing they can’t sleep without them. About 25% of users who take these aids daily for more than 10 days develop tolerance, needing higher doses for the same effect. Around 30% experience rebound insomnia-worse sleep than before-when they stop. This isn’t physical addiction, but it’s real enough to trap people in a cycle of reliance.
Why do doctors say melatonin isn’t effective for most insomnia?
Melatonin helps regulate the sleep-wake cycle, not induce sleep. It’s most useful for jet lag, shift work, or delayed sleep phase disorder-conditions where your internal clock is out of sync. For general insomnia, which is often caused by stress, anxiety, or poor sleep habits, melatonin has little impact. A 2022 review found it only reduced time to fall asleep by an average of 7 minutes. Most people with chronic insomnia need behavioral changes, not a hormone supplement.
What should I do if I’ve been using OTC sleep aids for months?
Stop using them gradually. Don’t quit cold turkey if you’ve been using them daily. Talk to a healthcare provider about switching to non-drug strategies like Cognitive Behavioral Therapy for Insomnia (CBT-I), which has a 70-80% success rate. Improve your sleep hygiene: go to bed and wake up at the same time every day, avoid screens before bed, keep your room cool and dark, and get morning sunlight. Most people who make these changes see better sleep within a few weeks-without any pills.





14 Comments