What if you could cut your monthly medication bill in half-or even to zero-without switching drugs? It’s not a trick. It’s a tier exception, and millions of people are missing out on it.
If you’ve ever opened your prescription bottle and seen a copay that made you pause-$150 for a drug you’ve been taking for years-you’re not alone. Many Medicare Part D beneficiaries pay far more than they should because their drug is stuck on a higher tier. But there’s a way out. A tier exception lets you move a drug from a costly tier to a cheaper one, if your doctor proves it’s medically necessary. And the savings can be huge.
What Exactly Is a Tier Exception?
Every Medicare Part D plan puts medications into tiers, like levels in a pricing game. Tier 1 is the cheapest-usually generics, often $0 to $10. Tier 2 is preferred brand-name drugs, maybe $10 to $40. Tier 3 is non-preferred brands, $50 to $100. Tier 4 and 5? Those are specialty drugs-biologics, cancer meds, rare disease treatments-and they can cost hundreds or even over $1,000 a month.
A tier exception isn’t about getting a drug that’s not on your plan’s list. That’s a formulary exception. A tier exception is for drugs that are already covered, but stuck on a high-cost tier. You’re asking the plan: “This drug is the right one for me. Can I pay the lower price that goes with a lower tier?”
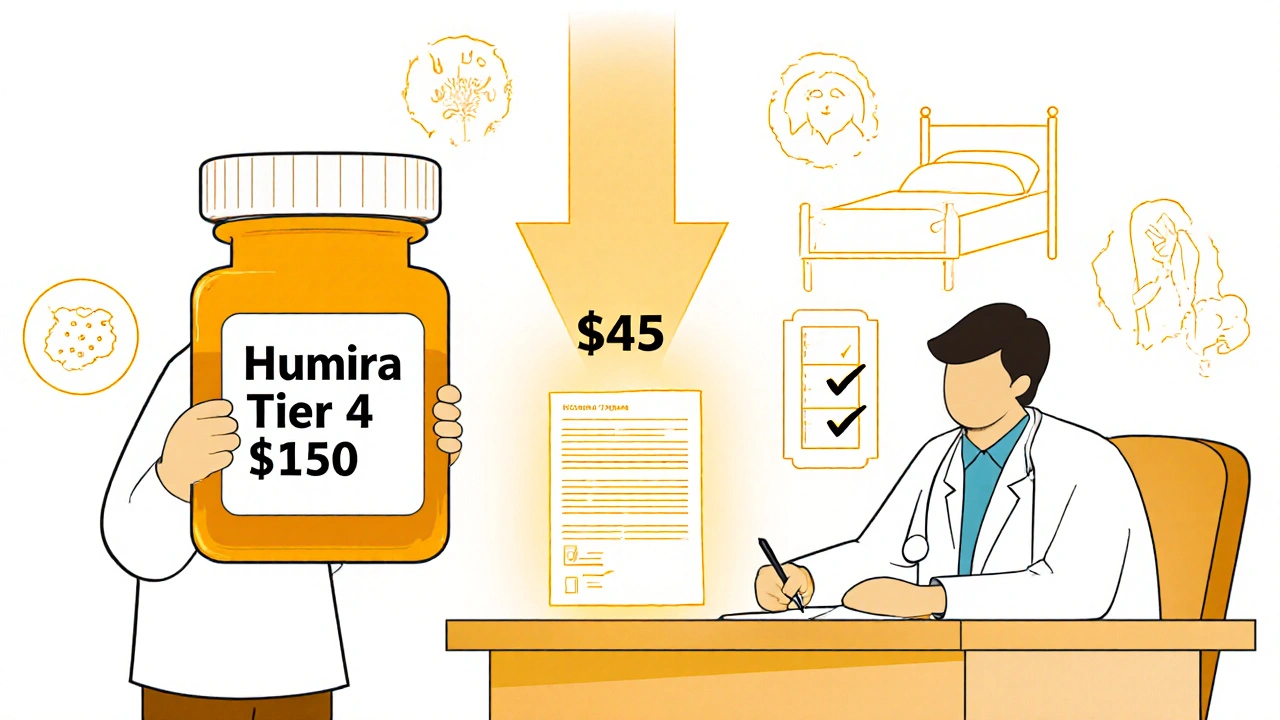
For example, if your Humira is on Tier 4 and costs $150 a month, a successful tier exception could drop it to Tier 3-$45 a month. That’s $1,260 saved a year. Some people even get their drug moved to Tier 1 and pay nothing. According to Sustainmeds.com, that’s not rare. One patient went from $47 to $0 per month just by filing the right paperwork.
Why Do Insurance Plans Use Tiers?
It’s not about punishing patients. It’s about money. Insurance companies negotiate discounts with drug makers. If a drug has a better deal, it gets placed on a lower tier. That’s why a drug like lisinopril (a common blood pressure med) might be on Tier 1-it’s cheap and widely used. But if your drug is newer, more complex, or has less competition, it lands on Tier 3 or higher.
But here’s the catch: just because a drug is on a higher tier doesn’t mean it’s worse. It just means the insurer didn’t get as good a deal on it. A Tier 3 drug might be the only one that works for you. That’s where the tier exception comes in.
When Do You Need a Tier Exception?
You don’t need one if you’re fine with the copay. But if you’re paying more than $50 a month for a drug you’ve been on for years, or if you’re hitting the coverage gap (donut hole), you should ask.
Common situations where tier exceptions work:
- You’re on a biologic drug for rheumatoid arthritis, multiple sclerosis, or psoriasis
- You tried the lower-tier drug and had side effects-rash, nausea, dizziness, or worse
- The lower-tier drug didn’t work at all-your symptoms didn’t improve
- You’re on a drug that’s been stable for years, but your plan changed tiers
- You’re in the coverage gap and paying 25% coinsurance-moving to a lower tier could cut your bill in half
According to the Medicare Rights Center, 58% of people who file tier exceptions get them approved. The biggest wins? Patients with chronic autoimmune diseases. One study showed patients on Humira, Enbrel, or Copaxone saved an average of $37.50 per fill after approval.
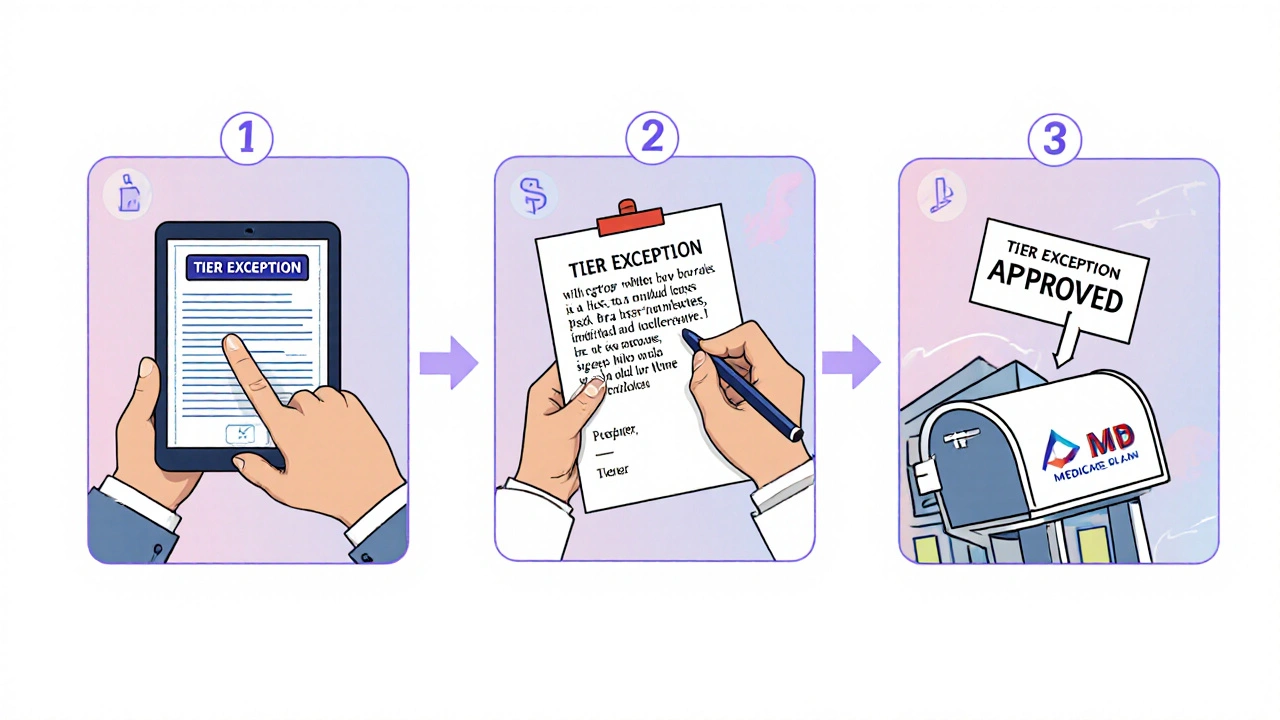
How to File a Tier Exception: The 3-Step Process
Filing a tier exception sounds complicated. It’s not. Here’s how it actually works.
- Get the form - Your doctor’s office should have it. It’s usually called a “Prior Authorization” or “Tier Exception Request” form. If they don’t, call your plan. Most have downloadable forms on their website. Don’t wait-start this before you fill your first prescription.
- Get the letter - This is the most important part. Your doctor must write a note explaining why the lower-tier drugs won’t work for you. Generic statements like “Patient prefers this drug” won’t cut it. They need to say: “Patient developed severe GI bleeding on warfarin. Switching to Xarelto was medically necessary to avoid hospitalization.” Or: “Patient had a rash and swelling on the preferred drug. Only this drug is tolerated.” Specifics matter. Vague = denial.
- Submit it - Your doctor’s office can submit it online, by fax, or by mail. You can also submit it yourself through your plan’s portal. Keep a copy of everything. The plan has 72 hours to respond if your doctor says your health is at risk, or 14 days for a standard request.
Pro tip: Ask your doctor to submit the request the same day they write the prescription. The Medicare Rights Center found that proactive requests (submitted at the same time as the script) have an 89% approval rate. Reactive requests (after you’ve been denied) drop to 67%.

Why Most Requests Get Denied (And How to Fix It)
Dr. Robert Johnson of UnitedHealthcare says 37% of initial tier exception requests are denied-not because they’re wrong, but because the paperwork is incomplete. The most common mistakes:
- Doctor writes: “Patient needs this drug.” Too vague.
- Doctor forgets to sign or date the form.
- Patient submits the form but not the clinical letter.
- Request is sent after the prescription is filled.
If you’re denied, don’t give up. About 78% of denials are overturned on appeal-with better documentation. You can file an appeal in writing. Include:
- Any lab results showing the lower-tier drug didn’t work
- Records of side effects or hospital visits
- Letters from specialists
- Proof you tried other drugs first
One Reddit user tried twice for Xarelto. First time: denied because the doctor didn’t explain why Eliquis (the preferred drug) was unsafe. Second time: added a note about a prior stroke and clotting risk. Approved-but only to Tier 2, not Tier 1. Still saved $30 a month.
What If Your Doctor Won’t Help?
If your doctor says no, ask why. Maybe they don’t know how. Or they think it’s too much work. Tell them: “I need this to afford my medication.” Most doctors will do it if you ask clearly.
If they still refuse, contact your plan’s patient advocate. Medicare plans are required to help you. Call the number on your card and say: “I need help filing a tier exception. My doctor needs support.” Many plans have nurses or pharmacists who can guide your doctor through the process.
You can also call the Medicare Rights Center at 1-800-333-4114. They’ll walk you through the form and even draft a letter template for your doctor.
Real Savings, Real Stories
People aren’t just saving a few bucks. They’re saving hundreds.
- A 72-year-old in Ohio got her Orencia moved from Tier 4 ($180) to Tier 2 ($25). Saved $1,860 a year.
- A 58-year-old with Crohn’s disease got his Stelara approved to Tier 1. Paid $0 instead of $120.
- A veteran in Florida had his Copaxone denied twice. On the third try, his neurologist added a note about muscle spasms from the generic. Approved to Tier 2. Saved $90/month.
These aren’t outliers. They’re standard outcomes. According to CMS, 62% of tier exceptions with full documentation get approved. That’s better than a coin flip.
What’s Changing in 2025?
The Inflation Reduction Act caps out-of-pocket drug costs at $2,000 a year for Medicare beneficiaries starting in 2025. That’s huge. But it doesn’t mean tier exceptions are obsolete.
Here’s why they still matter:
- The $2,000 cap only kicks in after you’ve spent that much. Until then, you’re still paying full tier prices.
- If your drug is on a lower tier, you’ll reach the cap faster-and save more over time.
- Many people don’t hit the cap. Lowering your copay now means less stress, fewer missed doses, and better health.
Plus, with the new CMS rules, plans must now offer electronic forms and faster processing. UnitedHealthcare’s automated pre-check tool cuts approval time from 9 days to under 4. More people will use this tool-and more will save money.
Final Checklist: Are You Ready to File?
Before you call your doctor, ask yourself:
- Is my drug on Tier 3, 4, or 5? (Check your plan’s formulary online)
- Have I tried lower-tier alternatives? (Even if they didn’t work)
- Do I have a medical reason why this drug is necessary? (Side effects? No response? History of complications?)
- Can my doctor write a clear, specific letter? (Not “I like this drug.” “This drug works. Others failed.”)
- Am I filing before I fill the prescription? (Timing matters)
If you answered yes to all five, you’re ready. File it. The worst that happens? You get denied. But if you don’t try, you’ll never know how much you could save.
Can I file a tier exception for any medication?
No. You can only file for drugs that are already on your plan’s formulary but listed on a higher cost tier. If your drug isn’t covered at all, you need a formulary exception, not a tier exception. Tier exceptions are for drugs you can get-but at a price you can’t afford.
How long does a tier exception take to approve?
Standard requests take up to 14 days. If your doctor says your health is at risk-like you’re having worsening symptoms or could be hospitalized-you can request an expedited review. That cuts the wait to 72 hours. Most approvals come within a week if the paperwork is complete.
What if my tier exception is denied?
You can appeal. About 78% of denials are overturned on appeal with better documentation. Get your doctor to add more clinical details-lab results, past treatment failures, side effect records. Submit the appeal in writing and keep copies. You have 60 days to appeal after the denial.
Do I need to be on Medicare Part D to use tier exceptions?
Tier exceptions are most common in Medicare Part D, but many private insurance plans (including employer plans and Medicaid managed care) use tiered formularies too. Check your plan’s website or call customer service. If they use tiers, they likely allow exceptions.
Can my doctor charge me for filling out the form?
No. Doctors cannot charge you for completing a tier exception form. It’s part of your care. If your doctor’s office tries to charge you, call your plan’s patient advocate. They’ll intervene. Many offices do this for free as part of patient support.
Will my copay stay low forever?
Not necessarily. Plans can change their formularies each year. But once approved, your tier exception usually stays in place for the rest of the plan year. Next year, you may need to reapply. But you’ll know the process-and you’ll be ahead of the game.
Next Steps: What to Do Today
Don’t wait until your next refill. Take action now.
- Log into your plan’s website. Look up your medication. Note the tier.
- If it’s Tier 3 or higher, call your doctor’s office. Say: “I need help filing a tier exception for [drug name]. Can you help?”
- Ask if they’ve done this before. If not, tell them to visit Medicare.gov or call the Medicare Rights Center.
- Submit the request before you fill your next prescription.
- Keep a copy of everything. Track the status online.
One form. One letter. One phone call. That’s all it takes to cut your medication costs. You’ve paid for your prescriptions. You deserve to pay the right price-not the highest one.






15 Comments