Diabetes Medication Comparison Tool
Which Diabetes Medication is Right for You?
Select your key priorities to see which diabetes medications best match your needs.
Recommended Medications
How we selected these medications
Based on your priorities and target HbA1c reduction, we've highlighted medications that match your needs best. Remember to discuss with your doctor before making any treatment changes.
Detailed Comparison
| Medication | HbA1c Reduction | Weight Effect | Cardiovascular Data | Hypoglycemia Risk | Cost (NZD/month) |
|---|---|---|---|---|---|
| Actos (Pioglitazone) | 0.5-1.0% | ~2 kg gain | Neutral; possible heart-failure ↑ risk | Low | ~30 |
| Metformin | 1.0-1.5% | Weight neutral or slight loss | Reduced CV events (UKPDS) | Low | ~15 |
| Empagliflozin (SGLT2) | 0.7-1.0% | ~2 kg loss | Reduced CV mortality, HF hospitalization | Low | ~180 |
| Liraglutide (GLP-1 RA) | 1.0-1.5% | 3-5 kg loss | Reduced MACE, weight-related CV benefit | Low | ~250 |
When your doctor mentions Actos (Pioglitazone) is a thiazolidinedione that improves insulin sensitivity in type 2 diabetes, you probably wonder how it stacks up against the flood of newer pills and injectables. This article breaks down the key differences, so you can decide whether pioglitazone fits your treatment plan or if an alternative makes more sense.
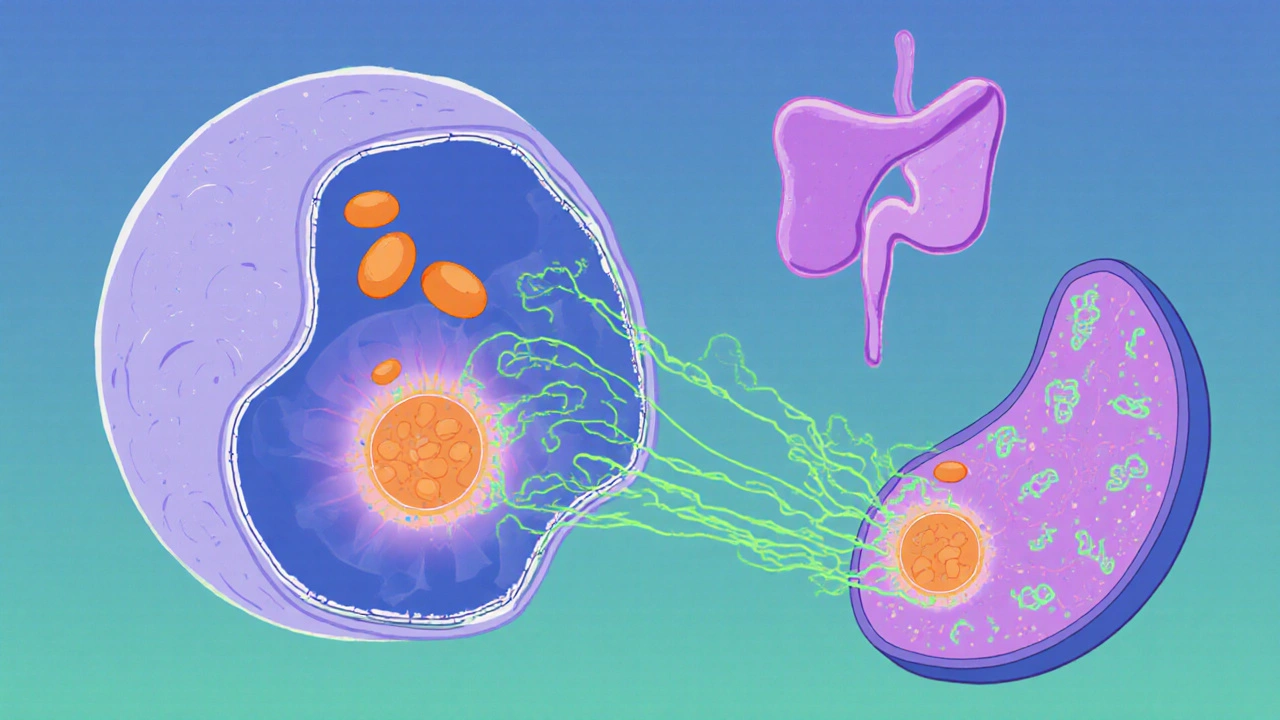
How Actos Works and Who Typically Uses It
Pioglitazone activates the PPAR‑γ receptor in fat and muscle cells, making them respond better to insulin. It doesn’t force your pancreas to produce more insulin, which means a lower risk of hypoglycemia compared with sulfonylureas. In New Zealand, the drug is approved by NZ MedSafe and the U.S. FDA for adults when diet, exercise, and first‑line metformin aren’t enough.
- Typical dose: 15-45 mg once daily with food.
- Onset of effect: 4-12 weeks for HbA1c reduction.
- Common side effects: weight gain, fluid retention, occasional liver enzyme elevation.
Because it works slowly and can cause edema, clinicians often reserve pioglitazone for patients who need better insulin sensitivity but can tolerate modest weight gain.
Why Look at Alternatives?
Since the early 2000s, a slew of new drug classes have entered the market. Some offer stronger glucose‑lowering power, heart‑benefit data, or weight‑loss effects that pioglitazone lacks. Below are the main families you’ll hear about:
- Metformin - biguanide, first‑line, reduces hepatic glucose production.
- Sulfonylureas (e.g., Glipizide) - stimulate insulin release.
- DPP‑4 inhibitors (e.g., Sitagliptin) - enhance incretin effect.
- SGLT2 inhibitors (e.g., Empagliflozin) - block glucose reabsorption in kidneys.
- GLP‑1 receptor agonists (e.g., Liraglutide) - injectable, promote insulin, curb appetite.
Decision Criteria You’ll Need
To compare fairly, line up the attributes that matter most for you or your clinician:
- Glycemic efficacy - average HbA1c drop.
- Weight impact - loss, neutral, or gain.
- Cardiovascular outcomes - heart‑failure risk, MACE benefit.
- Side‑effect profile - hypoglycemia, edema, GI upset.
- Cost & insurance coverage - NZ price points, PBS listings.
- Dosing convenience - oral vs. injection, frequency.
Head‑to‑Head Comparison Table
| Drug / Class | Typical HbA1c reduction | Weight effect | Cardiovascular data | Hypoglycemia risk | Common side effects | Cost (NZD/month) |
|---|---|---|---|---|---|---|
| Actos (Pioglitazone) | 0.5-1.0 % ↓ | ~2 kg gain | Neutral; possible heart‑failure ↑ risk | Low | Edema, bone fractures | ~30 |
| Metformin | 1.0-1.5 % ↓ | Weight neutral or slight loss | Reduced CV events (UKPDS) | Low | GI upset, B12 ↓ | ~15 |
| Glipizide (Sulfonylurea) | 0.8-1.3 % ↓ | Neutral | No CV benefit; possible ↑ risk | Moderate‑high | Hypoglycemia, weight gain | ~10 |
| Sitagliptin (DPP‑4) | 0.5-0.8 % ↓ | Weight neutral | Neutral | Low | URIs, mild nasopharyngitis | ~140 |
| Empagliflozin (SGLT2) | 0.7-1.0 % ↓ | ~2 kg loss | Reduced CV mortality, HF hospitalization | Low | UTI, genital infections, ketoacidosis | ~180 |
| Liraglutide (GLP‑1 RA) | 1.0-1.5 % ↓ | 3-5 kg loss | Reduced MACE, weight‑related CV benefit | Low | Nausea, vomiting, pancreatitis risk | ~250 (injectable) |
When Actos Might Be the Right Choice
Even with newer drugs, pioglitazone still has a niche:
- Low hypoglycemia risk - ideal for elderly or those on multiple agents.
- Cost‑effective - generic price far below most GLP‑1 RAs.
- Insulin‑sparing - can delay the need for injectable therapy.
- Specific hepatic insulin resistance - patients with fatty liver may benefit.
If your primary goal is modest HbA1c reduction without worrying about weight loss, and you can monitor for fluid retention, Actos remains a viable option.
Scenarios Where an Alternative Shines
Consider swapping when any of these apply:
- Weight gain is a concern - SGLT2 inhibitors or GLP‑1 RAs promote loss.
- Heart‑failure risk - Empagliflozin and other SGLT2s have proven benefits.
- Need for stronger HbA1c drop - GLP‑1 RAs or a combo of Metformin + SGLT2.
- Kidney impairment - DPP‑4 inhibitors are generally safer.
- Pregnancy or planning - Pioglitazone is contraindicated; Metformin is preferred.
Practical Decision Flow
- Start with Metformin unless contraindicated. \n
- If Metformin alone isn’t enough, assess patient priorities:
- Prefer oral, low cost, tolerate weight gain → consider pioglitazone.
- Need weight loss or CV benefit → choose SGLT2 or GLP‑1 RA.
- High hypoglycemia risk (elderly) → avoid sulfonylureas.
- Check renal function and heart‑failure status before picking SGLT2.
- Review insurance coverage; NZ Pharma costs vary widely.
- Re‑evaluate HbA1c after 3 months; adjust or add a second agent.
Key Takeaways
- Pioglitazone offers modest glucose control, low hypoglycemia, but adds weight and fluid‑retention risk.
- Metformin remains the cheapest, weight‑neutral first‑line.
- SGLT2 inhibitors and GLP‑1 receptor agonists provide both glucose lowering and weight loss, plus heart‑protective data.
- Cost, dosing convenience, and comorbidities drive the final choice.
Frequently Asked Questions
Can I take Actos with Metformin?
Yes. The combination is common when Metformin alone doesn’t achieve target HbA1c. It adds insulin‑sensitizing power without raising hypoglycemia risk.
Why does pioglitazone cause weight gain?
The drug promotes fat storage in subcutaneous tissue and can cause fluid retention, both of which add to the scale.
Is there a heart‑failure warning for Actos?
Yes. In patients with NYHA class III/IV heart failure, pioglitazone can worsen symptoms. Physicians avoid it in that group.
How does the cost of pioglitazone compare to newer drugs?
In New Zealand, generic pioglitazone is around NZD 30 per month, whereas SGLT2 inhibitors and GLP‑1 agonists often exceed NZD 150-250.
Can I switch from Actos to an SGLT2 inhibitor?
Switching is straightforward. Discontinue pioglitazone, start the SGLT2 inhibitor, and monitor kidney function and electrolytes during the transition.




10 Comments