When your blood sugar climbs too high, your body doesn’t just feel tired-it starts to shut down. Hyperglycemia isn’t just a number on a glucose meter. It’s a warning sign that your body can’t use the sugar in your blood, and if left unchecked, it can lead to a life-threatening emergency. This isn’t rare. In the U.S. alone, over 37 million people with diabetes face high blood sugar episodes regularly. But most don’t recognize the early signs until it’s too late.
What Exactly Is Hyperglycemia?
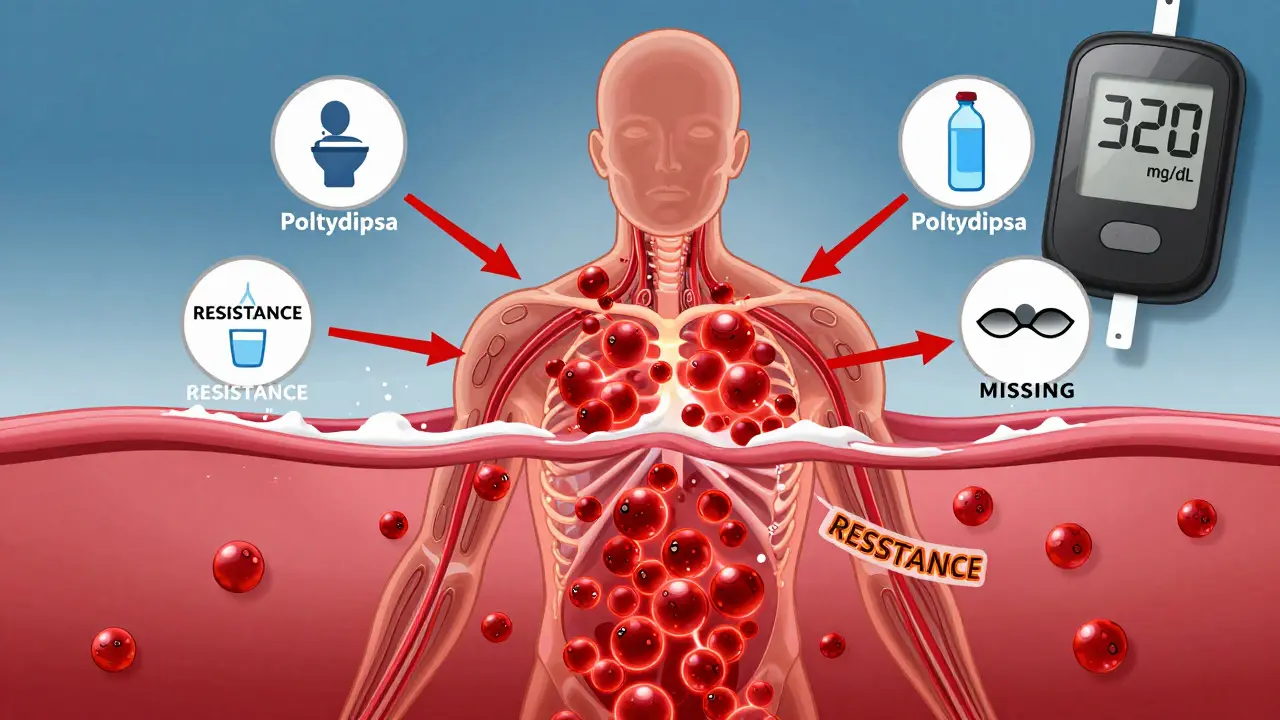
Hyperglycemia means your blood glucose level is above 180 mg/dL. For someone without diabetes, that’s unusually high. For someone with diabetes, it’s a signal that insulin isn’t working right-either because the body doesn’t make enough (type 1) or can’t use it properly (type 2). The result? Sugar piles up in your bloodstream instead of fueling your cells.
It’s not just about diet or forgetting insulin. Stress, illness, infections, even missed sleep can trigger it. Some people get it after eating too many carbs. Others experience it because their insulin pump failed, or they didn’t adjust their dose during sickness. The American Diabetes Association says nearly 45% of all diabetes-related hospital costs come from hyperglycemia complications. That’s not just a medical issue-it’s a daily reality for millions.
Early Warning Signs You Can’t Ignore
At first, hyperglycemia feels like ordinary fatigue. You’re tired. You’re thirsty. You’re peeing more than usual. But these aren’t just inconveniences-they’re your body screaming for help.
- Polyuria: Urinating more than 2.5 liters a day-often every hour or two. You might wake up multiple times at night.
- Polydipsia: Drinking more than 4 liters of fluids daily and still feeling parched. Water alone won’t fix it.
- Blurred vision: Sugar pulls fluid from the lenses of your eyes. Your vision gets foggy, especially when reading or driving.
- Unexplained weight loss: Even if you’re eating normally, your body starts breaking down fat and muscle because it can’t use glucose. Losing more than 5% of your body weight over a few months is a red flag.
According to the ADA, 68% of people with high blood sugar report blurred vision. And 79% say they feel drained-so drained they think it’s just stress or lack of sleep. That’s why so many wait until their blood sugar hits 300 mg/dL before acting.
When It Gets Serious: The Intermediate and Severe Symptoms
Once blood sugar climbs past 250 mg/dL, things shift fast. Headaches, trouble focusing, and nausea start showing up. By 300 mg/dL, your brain is struggling. You feel foggy, confused, or unusually irritable. This isn’t just "being off"-it’s your brain starving for fuel, even though there’s too much sugar in your blood.
At this stage, you might also notice:
- Difficulty concentrating at work or while driving
- Recurring infections-skin boils, yeast infections, slow-healing cuts
- Fruity-smelling breath (like nail polish remover)
These are signs your body is burning fat for energy because it can’t use glucose. That process creates ketones-acidic chemicals that poison your blood. If you’re type 1 diabetic, this could be the start of diabetic ketoacidosis (DKA). If you’re type 2, it could be hyperosmolar hyperglycemic state (HHS). Both are emergencies.
Diabetic Ketoacidosis (DKA) vs. Hyperosmolar Hyperglycemic State (HHS)
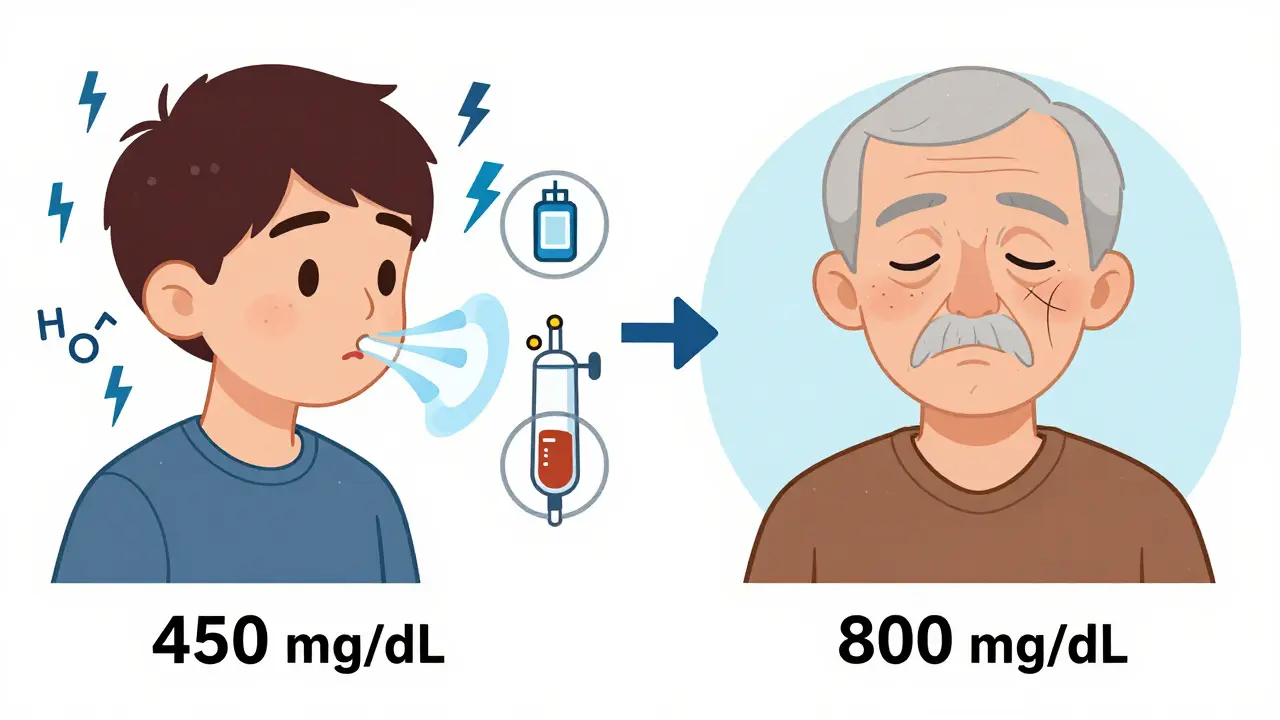
These are two different, equally dangerous outcomes of uncontrolled hyperglycemia. They look similar at first but have key differences.
| Feature | DKA | HHS |
|---|---|---|
| Typical patient | Type 1 diabetes, often under 45 | Type 2 diabetes, usually over 65 |
| Blood glucose level | 250-600 mg/dL | 600+ mg/dL |
| Ketones in blood | High (>3 mmol/L) | Low or absent |
| Dehydration | Moderate | Severe (8-12 liters lost) |
| Neurological symptoms | Mild confusion, drowsiness | Extreme lethargy, coma possible |
| Breathing pattern | Deep, fast (Kussmaul respirations) | Normal or shallow |
| Mortality rate | 1-5% | 15-20% |
HHS is deadlier, especially in older adults. One study found people over 65 with HHS have a 22% chance of dying. DKA hits younger people harder-70% of pediatric diabetes deaths are from DKA. Both need emergency care. Neither can be treated at home.
What to Do When Blood Sugar Is Over 240 mg/dL
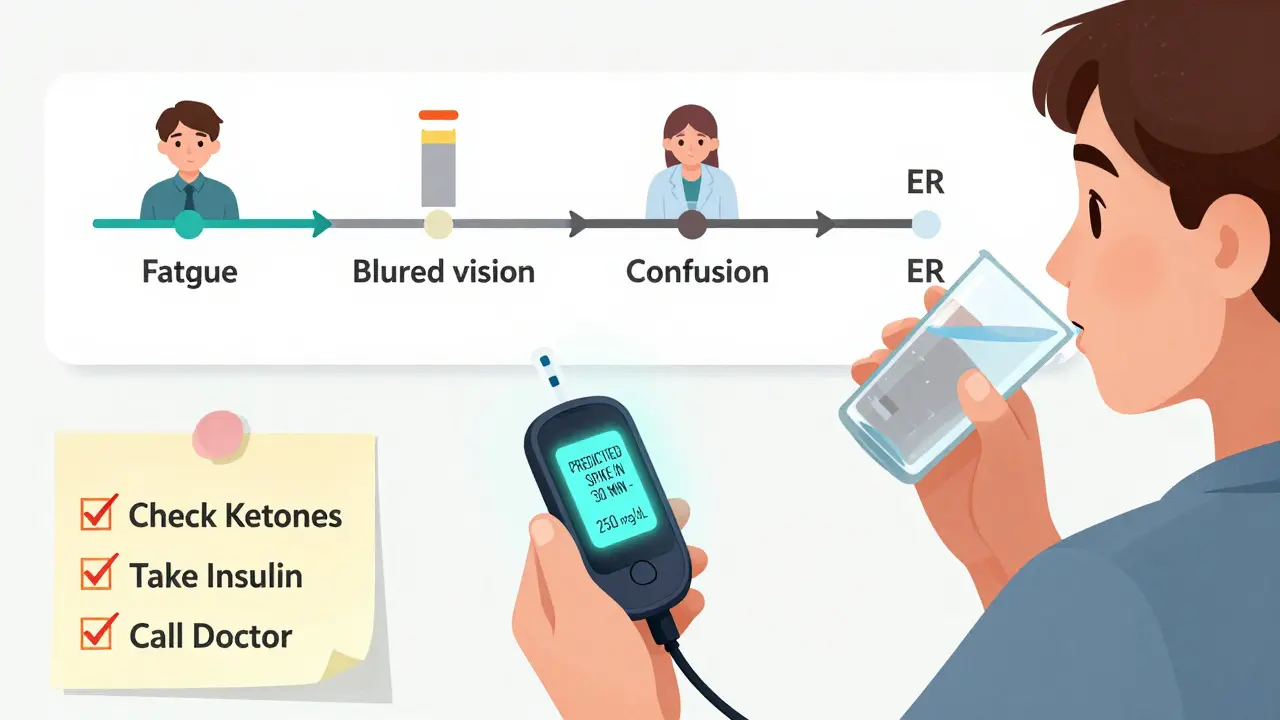
If your glucose hits 240 mg/dL or higher, don’t wait. Act now.
- Check for ketones. Use a urine strip or blood ketone meter. If ketones are moderate or high, don’t exercise-this can make it worse.
- Take your correction insulin. Use your personal insulin-to-carb ratio (usually 1 unit for every 10-15g carbs). If you’re unsure, use 0.1 units per kg of body weight.
- Drink water. Sip 8-16 oz of sugar-free fluid every hour. Avoid caffeine and alcohol-they dehydrate you more.
- Recheck your blood sugar in 2 hours. If it hasn’t dropped by at least 30-50 mg/dL, call your doctor or go to the ER.
- Don’t skip insulin. Even if you’re sick or not eating, you still need basal insulin. Skipping it is one of the top reasons people end up in the hospital.
Many people make the mistake of trying to "wait it out" or thinking they can fix it with just more water. That’s not enough. Insulin is the only thing that moves glucose out of your blood. Without it, your body keeps breaking down fat-producing more ketones, more acid, more damage.
Common Triggers You Might Not Realize
Hyperglycemia doesn’t just happen because you ate too much cake. Real triggers are often hidden:
- Illness or infection: A cold, flu, or UTI can spike blood sugar by 100+ mg/dL. Your body releases stress hormones that block insulin.
- Insulin pump failure: A clogged catheter, disconnected tubing, or expired insulin can cause rapid spikes. Check your pump every time your glucose is high.
- The dawn phenomenon: Between 4-8 a.m., your liver dumps sugar into your blood. Many people wake up with high readings and assume they ate too much the night before.
- Emotional stress: Anxiety, grief, or even arguments can trigger cortisol release, which raises blood sugar.
- Medications: Steroids, some antidepressants, and even decongestants can cause hyperglycemia.
One patient survey found 42% of high blood sugar episodes were linked to illness. Another 29% were from carb-counting errors. Only 18% were from pump failures-but those are the ones that spike fastest.
What Not to Do
There are dangerous myths about managing high blood sugar:
- Don’t exercise to lower it. If ketones are present, exercise makes DKA worse.
- Don’t take extra insulin without checking ketones. Too much insulin too fast can crash your blood sugar and cause seizures.
- Don’t assume it’s "just stress" or "a bad day." Repeated high readings mean your plan needs adjusting.
- Don’t wait for symptoms to get worse. By the time you’re confused or vomiting, it’s already an emergency.
One of the biggest mistakes? "Insulin stacking." That’s when someone takes another dose because their blood sugar didn’t drop fast enough-and then takes another dose 30 minutes later. The result? A dangerous drop later, often while sleeping. It’s responsible for 33% of insulin pump errors.
Technology That’s Changing the Game
Continuous glucose monitors (CGMs) are no longer luxury tools-they’re lifesavers. People using CGMs reduce severe hyperglycemia episodes by 57%, according to the Diabetes Technology Society. Why? Because they catch spikes before you feel them.
The FDA just approved Dexcom G7’s "Glucose Guardian"-a predictive algorithm that warns you 30 minutes before your blood sugar hits 250 mg/dL. That’s game-changing. It gives you time to drink water, take insulin, or call someone before you’re in crisis.
Apps linked to CGMs also track patterns. If you notice your sugar spikes every time you’re stressed or after eating rice, you can adjust. But tech only works if you act on the alerts. One JAMA study found 19% of people with repeated hyperglycemia had undiagnosed gastroparesis-a condition where food sits in the stomach too long, delaying insulin absorption.
When to Go to the ER
Call 911 or go to the emergency room if you have:
- Blood sugar over 300 mg/dL with ketones present
- Confusion, drowsiness, or difficulty staying awake
- Deep, rapid breathing
- Fruity-smelling breath
- Vomiting or abdominal pain
- Loss of consciousness
Don’t wait for all of these. Even one or two-especially if you’re feeling worse-means you need help now. HHS can sneak up on older adults. They might just seem "out of it," but their blood sugar could be over 800 mg/dL. That’s a coma waiting to happen.
Prevention Is Possible
The good news? Most hyperglycemia emergencies are preventable. The CDC’s Diabetes Self-Management Education program reduces hospital visits by 42%. Why? Because people learn what to look for-and what to do.
Here’s what works:
- Test your blood sugar at least twice a day-more if you’re sick or changing your routine.
- Keep fast-acting insulin and ketone strips on hand.
- Have a written plan from your doctor for high blood sugar.
- Use a CGM if you can afford it-or ask about Medicare coverage (expanded in 2023).
- Call the ADA’s 24/7 hotline if you’re unsure. They handle 12,000 calls a month and have an 89% satisfaction rate.
It’s not about perfection. It’s about awareness. One small change-like checking ketones before exercising when your sugar is high-can keep you out of the ER.
Can you have high blood sugar without having diabetes?
Yes. While most cases are tied to diabetes, other conditions can cause hyperglycemia. Severe stress from trauma, infection, or surgery can trigger temporary spikes. Certain medications like steroids or antipsychotics raise blood sugar in up to 70% of users. Cushing’s syndrome, pancreatic diseases, and even rare tumors can also cause high glucose. If you’ve never been diagnosed with diabetes but keep having high readings, see an endocrinologist.
How long does it take for high blood sugar to cause damage?
Damage starts within hours. High glucose coats blood vessels and nerves, causing inflammation. Over time, this leads to kidney disease, vision loss, and nerve damage. But the real danger is acute: blood sugar over 300 mg/dL for more than 24 hours can trigger DKA or HHS. These can develop in as little as 12-24 hours if insulin is missing. That’s why acting fast matters more than long-term control.
Why does my blood sugar spike in the morning?
This is called the dawn phenomenon. Between 4 and 8 a.m., your body naturally releases cortisol and growth hormone to prepare you for the day. These hormones make your liver release glucose and block insulin. If your nighttime insulin dose is too low or your basal rate is off, this causes a spike. Adjusting your insulin timing or basal rate (under your doctor’s guidance) can fix this.
Can stress really cause high blood sugar?
Absolutely. Stress triggers your fight-or-flight response. Your liver dumps glucose into your blood to give you energy. At the same time, stress hormones make your body less sensitive to insulin. Even emotional stress-like an argument or grief-can raise blood sugar by 50-100 mg/dL. Managing stress isn’t optional-it’s part of diabetes care.
Is it safe to exercise when my blood sugar is high?
Only if your ketones are negative. If your blood sugar is over 250 mg/dL and you have moderate or high ketones, don’t exercise. Physical activity can make DKA worse by pushing more ketones into your blood. If ketones are low or absent and you feel okay, light activity like walking may help lower your sugar. Always test ketones first.
What should I do if I’m sick and my blood sugar is high?
Stay on your insulin-even if you can’t eat. Illness raises blood sugar, so you may need more insulin than usual. Drink sugar-free fluids every hour. Test your blood sugar every 2-4 hours. Check ketones if your sugar is over 240 mg/dL. Call your doctor if your sugar stays above 300 mg/dL for more than 6 hours, or if you’re vomiting, dizzy, or confused.
Can I treat hyperglycemia with just diet and water?
No. Water helps with dehydration, and avoiding carbs prevents further spikes, but insulin is the only thing that moves glucose out of your blood. Without insulin, your body keeps breaking down fat and producing ketones. That’s what leads to DKA. Diet and hydration are supportive-but they’re not treatments. Insulin is.
Final Thought: It’s Not About Fear-It’s About Knowing
High blood sugar isn’t a failure. It’s data. Every time your glucose is high, it’s telling you something: your body needs more insulin, you’re stressed, you’re sick, or your plan needs tweaking. The goal isn’t to never have a high reading-it’s to recognize it fast, respond correctly, and avoid the emergency.
People who survive hyperglycemic emergencies don’t have perfect control. They have awareness. They check their numbers. They know their ketone thresholds. They call for help before it’s too late.
You don’t need to be perfect. You just need to be ready.






14 Comments