Why Timing Matters More Than You Think
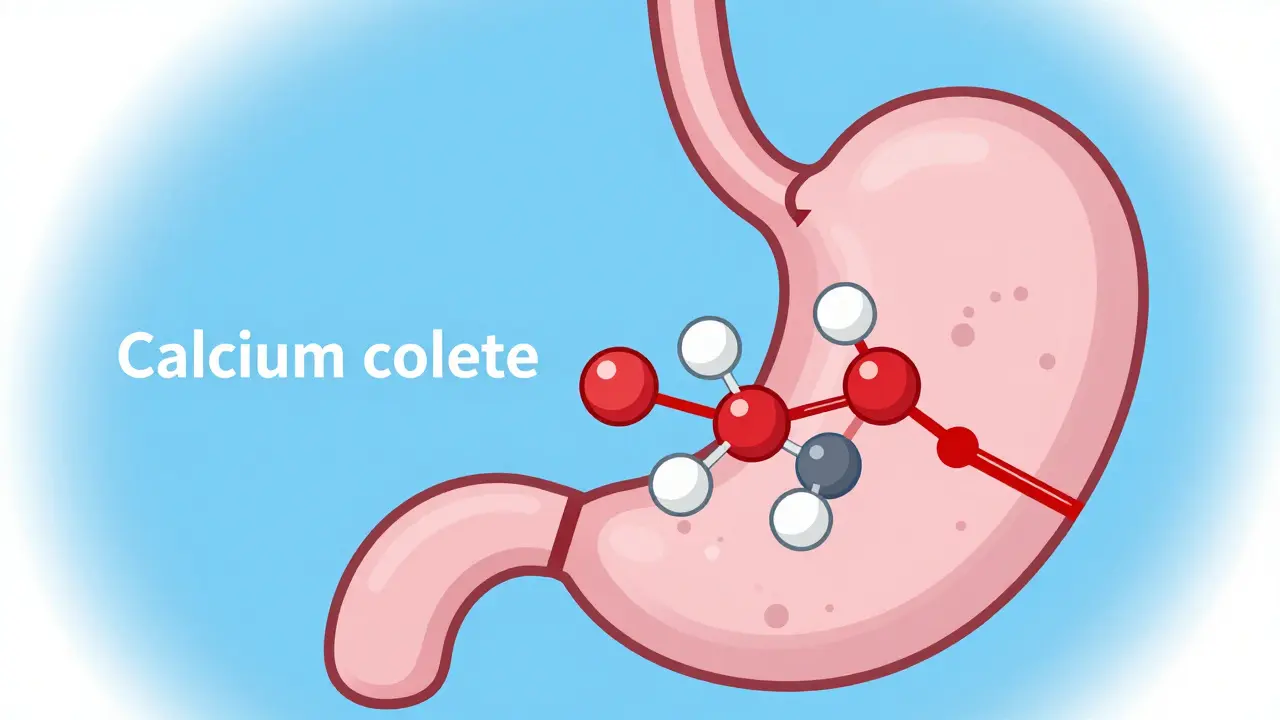
Antacids are common over-the-counter medications that neutralize stomach acid. They typically contain minerals like calcium carbonate, magnesium hydroxide, or aluminum hydroxide. If you take them at the same time as certain antibiotics, they can drastically reduce the antibiotic's effectiveness. For example, fluoroquinolones like ciprofloxacin can lose up to 90% of their absorption when taken with antacids containing magnesium or aluminum. This isn't just a minor issue-it's a major reason why some infections don't clear up as expected.
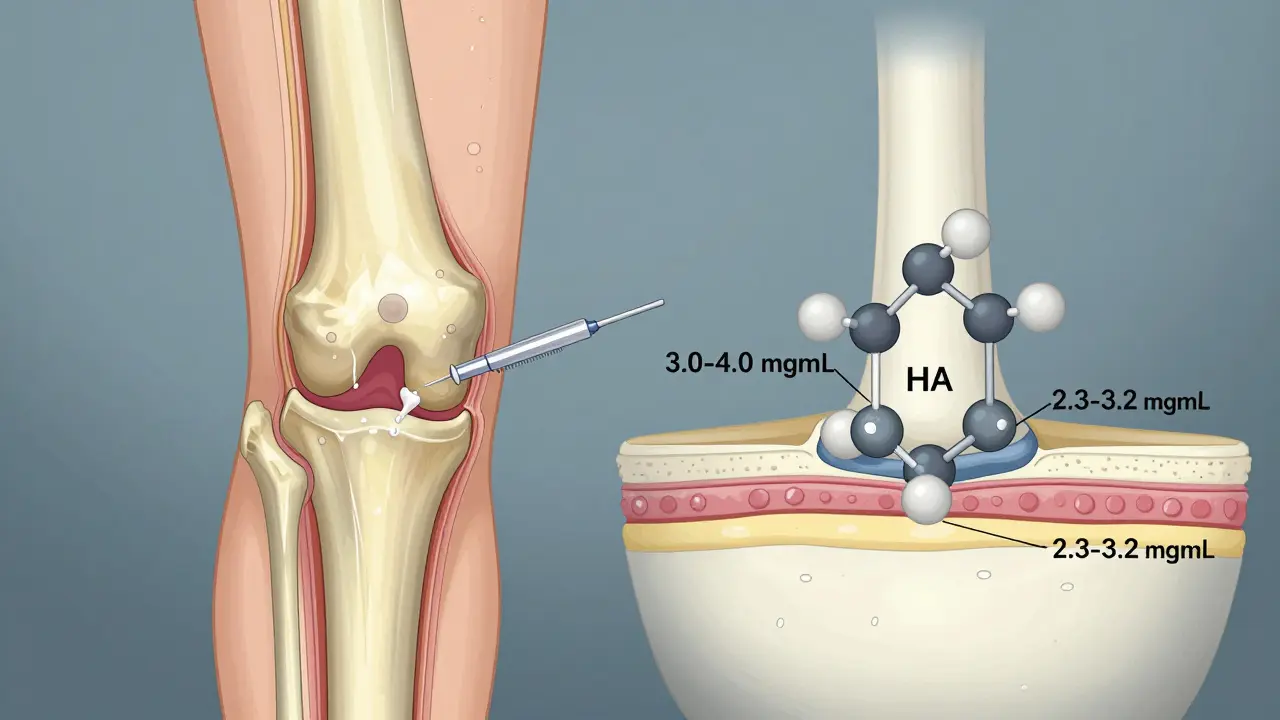
So why does this happen? There are two main mechanisms. First, chelation occurs when minerals in antacids bind directly to antibiotics, forming compounds your body can't absorb. Second, antacids increase stomach pH, which affects how well some antibiotics dissolve and get absorbed. Both processes mean your antibiotic might not reach the levels needed to fight the infection.
Which Antibiotics Are Most Affected?
Not all antibiotics interact with antacids the same way. Some are hit hard, while others are barely affected. Here's the breakdown:
- Fluoroquinolones (e.g., ciprofloxacin, levofloxacin) are the most vulnerable. Studies show up to 90% reduced absorption when taken with antacids. The NHS recommends taking them at least 4 hours before or after antacids.
- Tetracyclines (e.g., doxycycline, tetracycline) also suffer significant reductions. These antibiotics bind tightly to calcium and magnesium, leading to 50-70% lower absorption. Separation of 2-3 hours is key.
- Penicillins like amoxicillin are less affected, but still see 15-20% reduced absorption. A 1-hour separation is usually sufficient.
- Macrolides (e.g., azithromycin, clarithromycin) have minimal interaction, but 2 hours separation is still recommended as a precaution.
- Metronidazole shows no significant interaction with antacids, so timing isn't a concern here.
Quick Reference: Timing Guidelines
| Antibiotic Type | Separation Time | Why It Matters |
|---|---|---|
| Fluoroquinolones (e.g., ciprofloxacin) | 4 hours before or after antacids | Binding to minerals reduces absorption by up to 90% |
| Tetracyclines (e.g., doxycycline) | 2-3 hours before or after antacids | Chelation with calcium or magnesium |
| Penicillins (e.g., amoxicillin) | 1 hour before or after antacids | 15-20% reduced absorption; less severe |
| Macrolides (e.g., azithromycin) | 2 hours separation | Minimal interaction but still recommended |
| Metronidazole | No separation needed | No significant interaction with antacids |
Practical Tips for Getting the Timing Right
Managing multiple medications can be tricky, especially when you need to space doses by hours. Here's how to stay on track:
- Use medication alarms: Set reminders on your phone for when to take each medication. For example, if you take ciprofloxacin twice a day, set alarms for 2 hours before meals and 4 hours after antacids.
- Ask your pharmacist for help: Pharmacists can create a simple schedule tailored to your specific meds. Many pharmacies offer free medication management tools.
- Try a medication app: Apps like MyMedSchedule (used by over 1.2 million people) have built-in alerts for antacid-antibiotic interactions and auto-schedule your doses.
- Keep a written schedule: Write out your dosing times on a calendar and stick it on your fridge. Visual cues work better than memory for many people.
What If You Can't Separate Doses?
Sometimes, life gets in the way. If you're struggling to space out your doses, talk to your doctor about alternatives. For example, switching from antacids to H2 blockers like famotidine or proton pump inhibitors like omeprazole can help. These medications don't contain the minerals that cause chelation, so they're safer to take with antibiotics. A 2023 study found that switching to H2 blockers or PPIs reduced treatment failure rates from 27% to 9% in patients needing both acid-reducing therapy and antibiotics.
But don't switch meds without consulting your doctor. Some antibiotics still interact with H2 blockers or PPIs, though usually less severely. Your doctor can help you find the safest option for your situation.
Frequently Asked Questions
What if I accidentally take my antibiotic and antacid at the same time?
Don't panic. If you realize right away, wait at least 2 hours before taking your next dose of antibiotic. For example, if you took ciprofloxacin with Tums, wait 2 hours before taking the next ciprofloxacin dose. However, if it's close to your next scheduled dose, skip the missed dose. Never double up on antibiotics. Always check with your pharmacist or doctor for specific advice.
Can I take antacids with all antibiotics?
No. While some antibiotics like metronidazole and penicillins have minimal interactions, others like fluoroquinolones and tetracyclines are highly affected. Always check the label or ask your pharmacist about your specific antibiotic. If you're unsure, assume there's an interaction and space the doses apart.
Are over-the-counter antacids safer than prescription ones?
Not necessarily. The active ingredients in OTC antacids (like calcium carbonate in Tums or magnesium hydroxide in Milk of Magnesia) are the same as in some prescription versions. What matters is the type and amount of minerals they contain. All antacids with aluminum, magnesium, or calcium can interact with antibiotics, regardless of whether they're OTC or prescription.
How long do I need to separate doses?
It depends on the antibiotic. Fluoroquinolones require 4 hours before or after antacids. Tetracyclines need 2-3 hours. Penicillins and macrolides need about 1-2 hours. Always check the specific guidelines for your medication. When in doubt, wait 4 hours to be safe.
Why do some sources say different timing recommendations?
Timing guidelines can vary slightly based on the specific drug formulation and individual patient factors. For example, newer antibiotics or extended-release versions might have different interaction profiles. Always follow your doctor's advice or the instructions on your prescription label. Clinical guidelines from the FDA and NHS are the most reliable sources for current recommendations.
Next Steps for Patients
Take action today to protect your treatment:
- Check your medication labels: Look for warnings about antacids or other acid reducers. If it's not clear, ask your pharmacist.
- Set up reminders: Use your phone or a pill organizer to track doses. Apps like MyMedSchedule can automate this for you.
- Talk to your doctor: If you're struggling with timing, ask about alternative medications or dosing schedules. Your doctor can often adjust your treatment plan to fit your lifestyle.
- Keep a medication log: Note when you take each drug and any symptoms. This helps your healthcare team spot issues early.
Remember, proper antacid antibiotic timing is crucial for ensuring your antibiotics work as intended. With a little planning, you can avoid the pitfalls and get the best results from your antibiotics.





10 Comments