Every year, more than 36,000 older adults in the U.S. die from falls. That’s more than car accidents. And a big part of the reason? Medications. Not because they’re dangerous by design, but because they’re often kept too long, taken in combination, or prescribed without checking how they affect balance, blood pressure, or thinking. For seniors, even a small change in medication can mean the difference between staying steady on their feet and ending up in the hospital-or worse.
What Makes a Medication Risky for Falls?
It’s not just about being old. It’s about how drugs interact with the aging body. As we get older, our liver and kidneys don’t process medications the same way. Drugs stick around longer. Side effects get stronger. And the brain becomes more sensitive to things that make you drowsy, dizzy, or confused.
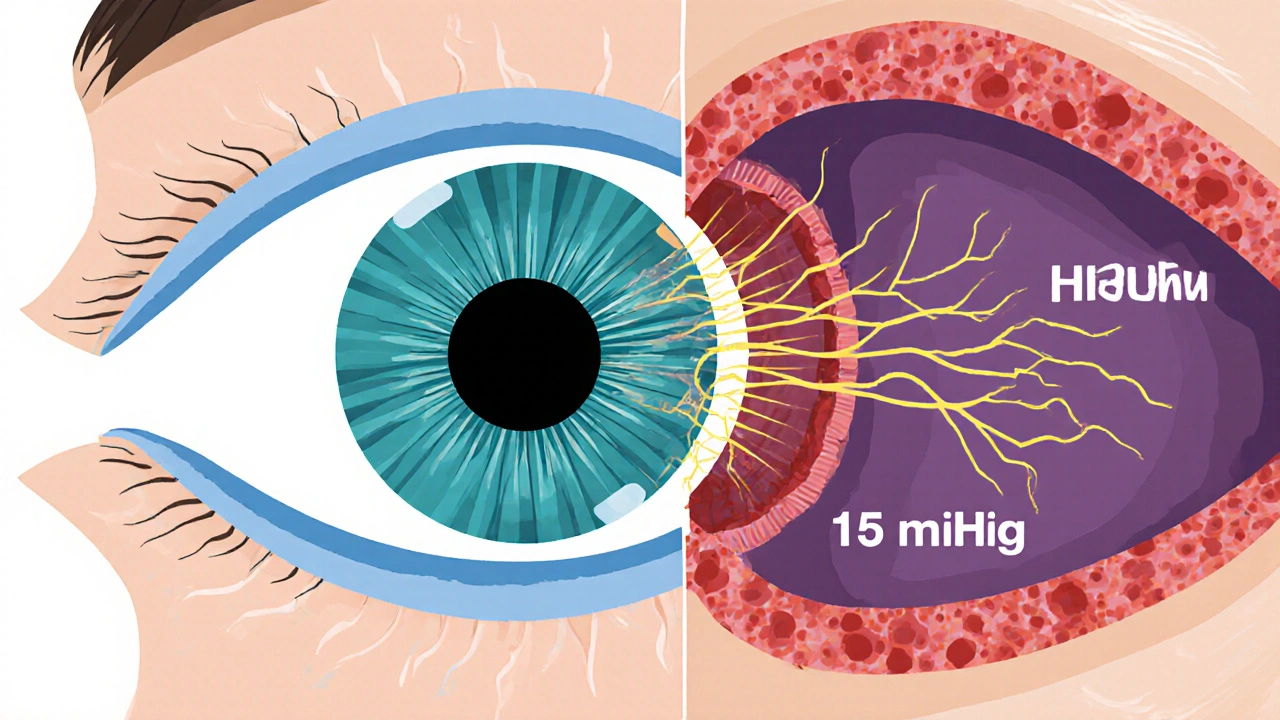
The real danger comes from drugs that affect your central nervous system. These include medications for anxiety, depression, sleep, pain, and even allergies. They slow down your reactions, blur your vision, or drop your blood pressure when you stand up. That’s called orthostatic hypotension-and it’s a silent killer in older adults. One moment you’re walking to the bathroom, the next you’re on the floor.
Top Medications That Increase Fall Risk
According to the American Geriatrics Society’s Beers Criteria (updated in 2023), these are the drug classes most linked to falls in seniors:
- Antidepressants-especially tricyclics like amitriptyline and nortriptyline. These block acetylcholine, which affects balance and causes dry mouth, constipation, and dizziness. Even SSRIs like sertraline or fluoxetine increase fall risk by over 100% in some studies.
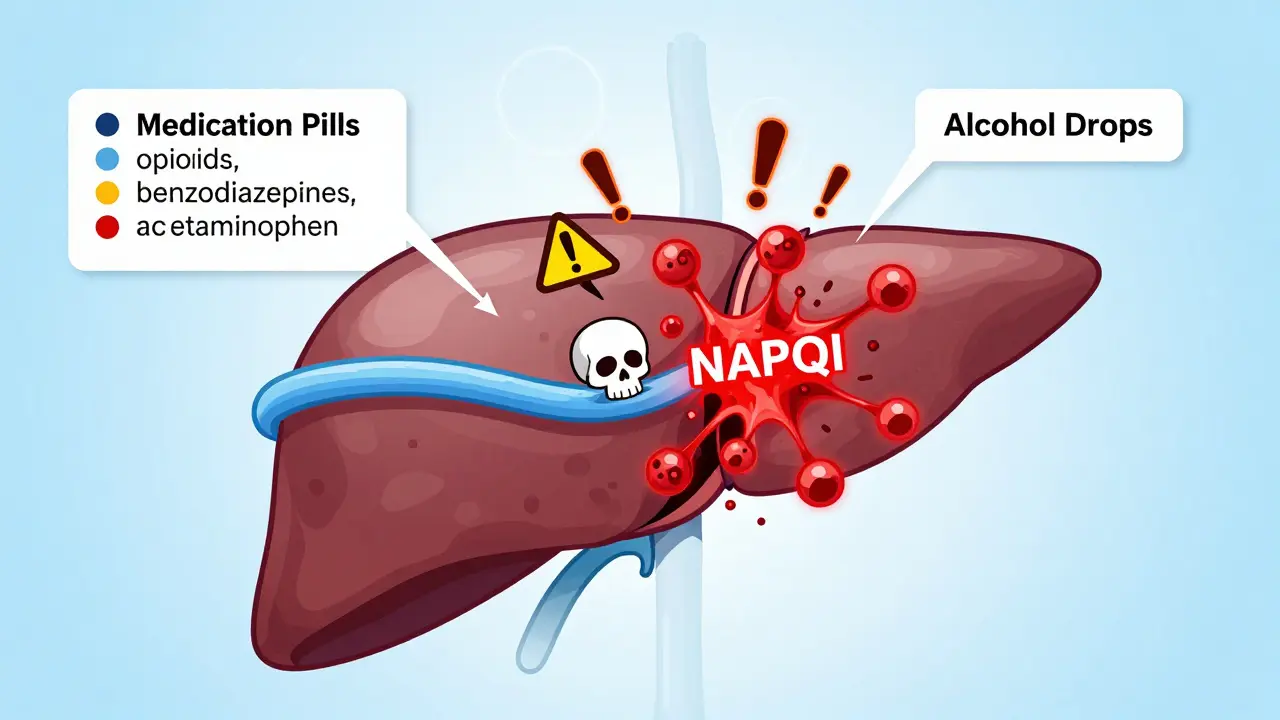
- Benzodiazepines-like diazepam (Valium) or lorazepam (Ativan). These are prescribed for anxiety or insomnia but cause sedation, memory lapses, and delayed reaction times. Long-acting ones are especially dangerous because they build up in the system.
- Antipsychotics-used off-label for agitation in dementia. Drugs like quetiapine or risperidone can cause muscle stiffness, tremors, and sudden drops in blood pressure. They’re often given without proper monitoring.
- Opioids-oxycodone, hydrocodone, tramadol. These slow reflexes and cause dizziness. The risk skyrockets when combined with benzodiazepines-studies show a 150% higher chance of falling.
- Blood pressure meds-especially when doses are changed. Beta blockers like carvedilol, ACE inhibitors like lisinopril, and diuretics like hydrochlorothiazide can cause sudden drops in blood pressure. Many seniors don’t realize their fall was tied to a recent dose increase.
- Antihistamines-over-the-counter sleep aids like diphenhydramine (Benadryl) or doxylamine (Unisom). These are strong anticholinergics. They fog your brain and dry out your mouth and eyes. Yet they’re still sold as “safe” for seniors.
- Muscle relaxants-like cyclobenzaprine or methocarbamol. They’re meant for short-term use, but often get prescribed for chronic back pain. They cause drowsiness and loss of coordination.
- Anticholinergics for bladder control-such as oxybutynin or tolterodine. These reduce urgency but also impair memory and increase confusion. Many seniors don’t connect their falls to their “bladder pill.”
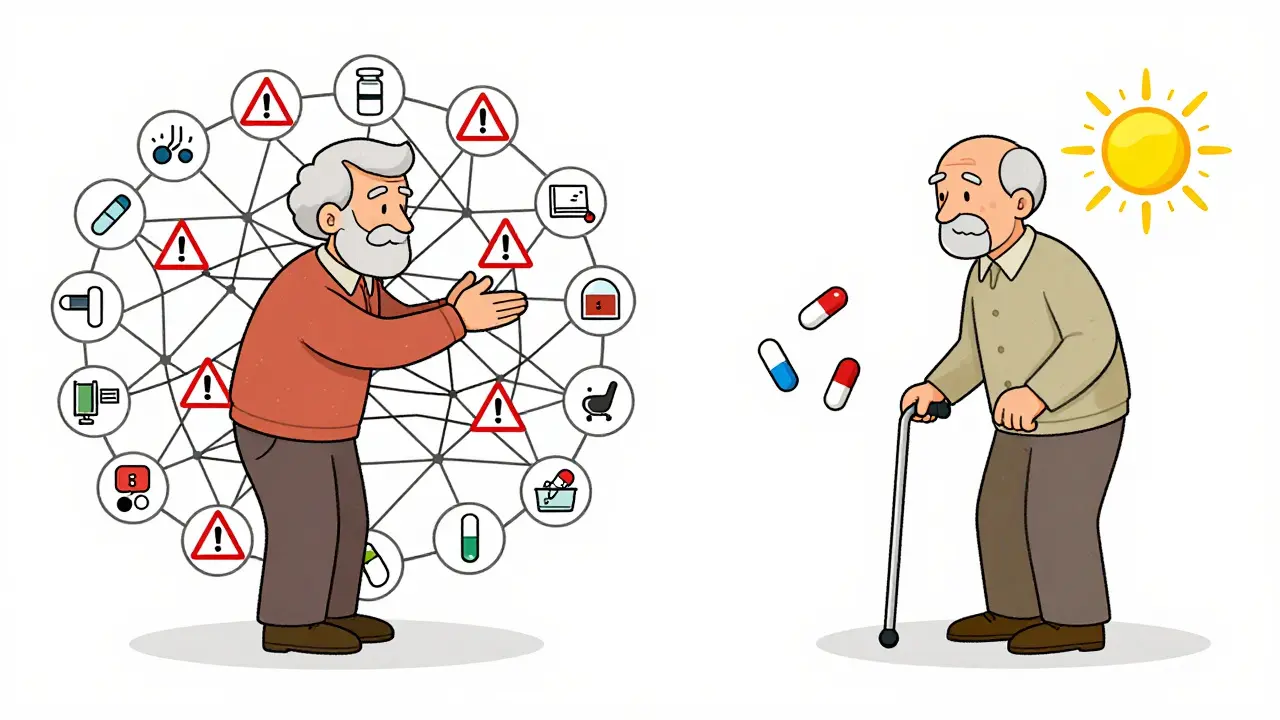
Here’s the kicker: it’s not just one drug. It’s the mix. A 2023 study in JAMA Health Forum found that 65% to 93% of seniors hospitalized after a fall were taking at least one of these drugs-and nearly half were taking three or more. That’s called polypharmacy. And it’s the hidden epidemic.
Why Do Doctors Keep Prescribing These?
It’s not because they don’t know better. It’s because it’s hard to stop.
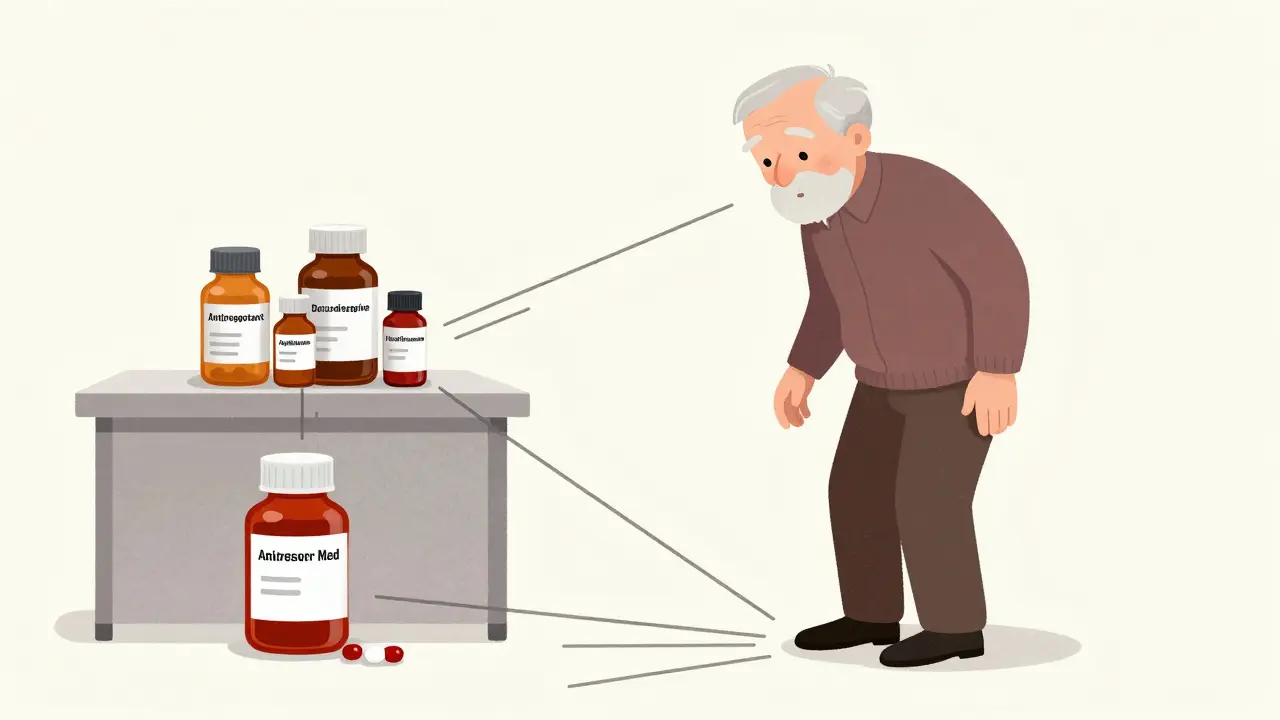
Many seniors see multiple doctors. One prescribes a sleep aid. Another adds an antidepressant. A third gives a painkiller. No one talks to the others. The primary care doctor might not even know about the over-the-counter Benadryl the patient takes every night. And once a drug is started, it’s easier to keep giving it than to take it away.
Doctors also worry about upsetting patients. If someone says, “I can’t sleep,” giving a pill feels like a quick fix. But the long-term cost? Falls, fractures, hospital stays, loss of independence. The real cost isn’t just medical-it’s emotional. Many seniors never fully recover their confidence after a fall.
What Can Be Done?
The good news? You can fix this.
Dr. Cara Cassino, a geriatrician with the CDC’s STEADI program, says: “Reviewing medications with all patients 65 and older is the single most effective clinical intervention for reducing fall risk.”
Here’s what works:
- Ask for a full med review-every year. Bring every pill bottle, supplement, and OTC product to your doctor. Include what you take for sleep, pain, or allergies.
- Ask: “Is this still necessary?”-Especially for drugs taken for more than a few months. Many were started for a short-term issue and never stopped.
- Check for interactions-Opioids + benzodiazepines? That’s a red flag. Antidepressants + anticholinergics? That’s a double hit.
- Test for orthostatic hypotension-Ask your doctor to check your blood pressure while sitting and then standing. A drop of 20 mm Hg systolic or 10 mm Hg diastolic is a sign your meds might be too strong.
- Consider a pharmacist-led review-Programs like HomeMeds have shown that trained pharmacists can cut fall rates by 22% just by identifying and adjusting risky meds.
- Deprescribe, don’t just stop-Don’t quit cold turkey. Work with your doctor to taper off slowly. Some meds, like benzodiazepines, need weeks or months to come off safely.
One woman in her 70s from Auckland came in after three falls in six months. She was on a sleep aid, an antidepressant, a blood pressure pill, and a bladder medication. Her doctor didn’t know about the sleep aid. After removing the diphenhydramine and lowering the antidepressant dose, her balance improved in two weeks. No more falls. No new prescriptions. Just a cleaner list.
What About “Safer” Alternatives?
Some people think switching to “safer” versions helps. Like using a short-acting benzodiazepine instead of a long-acting one. Or choosing an SSRI over a tricyclic. But the data doesn’t back that up.
A 2018 meta-analysis found that even “safer” antidepressants still doubled fall risk. Short-acting benzodiazepines still cause dizziness and memory issues. There’s no magic bullet. The safest option isn’t a different drug-it’s fewer drugs.
Non-drug solutions work better. For sleep: better light exposure, regular bedtime, cutting caffeine after noon. For anxiety: therapy, mindfulness, movement. For bladder issues: pelvic floor exercises, timed voiding. For pain: physical therapy, heat, acupuncture. These don’t come with a warning label about falling.

What Should You Do Right Now?
If you or someone you care about is over 65 and has fallen-even once-take action.
- Make a list of every medication, supplement, and OTC product taken daily.
- Bring it to your doctor or pharmacist. Ask: “Which of these could be making me unsteady?”
- Don’t be afraid to say: “I’d like to see if I can stop or lower this.”
- If your doctor says no, ask for a referral to a geriatrician or clinical pharmacist.
- Track your balance. Can you stand on one foot for 10 seconds? Can you walk heel-to-toe in a straight line? If not, your risk is higher.
Falls aren’t accidents. They’re signals. And medications are often the loudest one.
When to Seek Help
Call your doctor immediately if:
- You’ve fallen more than once in the last year.
- You feel dizzy when standing up.
- You’ve started a new medication and noticed balance problems.
- You’re taking four or more prescription drugs.
- You’re taking an opioid and a sleep aid or anxiety medication together.
These aren’t minor concerns. They’re warning signs that your body is under too much chemical stress.
Can over-the-counter medicines cause falls in seniors?
Yes. Many OTC drugs, especially first-generation antihistamines like diphenhydramine (Benadryl) and doxylamine (Unisom), are strong anticholinergics. They cause drowsiness, dry mouth, blurred vision, and confusion-all of which increase fall risk. Sleep aids, allergy pills, and stomach remedies often contain these ingredients. Just because they’re sold without a prescription doesn’t mean they’re safe for older adults.
Are there any medications that are safe for seniors to take without increasing fall risk?
Some medications are low-risk when used correctly, like certain blood pressure drugs if doses are stable, or thyroid meds like levothyroxine. But the real answer is: it’s not about the drug-it’s about the number and combination. Even “safe” meds become risky when taken with others. The safest approach is to use the fewest number of drugs possible and review them regularly.
How often should seniors have their medications reviewed?
At least once a year, and every time a new medication is added or changed. The CDC and American Geriatrics Society recommend a full medication review during annual wellness visits. If a senior has fallen, had a hospital stay, or started seeing a new specialist, a review should happen immediately-not months later.
Can stopping a medication actually improve balance?
Absolutely. Studies show that carefully reducing or stopping fall-risk-increasing medications can lower fall rates by 20-30%. One 2021 study found that seniors who had their benzodiazepines or antidepressants tapered off under medical supervision saw noticeable improvements in walking speed and balance within 4-8 weeks. The body often regains its natural stability once the chemical fog lifts.
What’s the difference between the Beers Criteria and STOPP/START?
The Beers Criteria is a list of medications that should be avoided in older adults because of high fall risk or other side effects. STOPP (Screening Tool of Older Persons’ Prescriptions) helps identify inappropriate prescriptions-like giving a muscle relaxant to someone with dementia. START (Screening Tool to Alert to Right Treatment) finds missing but needed meds, like a bone-strengthening drug for someone with osteoporosis. Together, they help doctors both stop bad drugs and start good ones.
Is polypharmacy always dangerous for seniors?
Not always-but it’s risky. Taking four or more medications increases fall risk significantly, especially if any are central nervous system-active. The problem isn’t the number alone-it’s whether each drug is still needed, whether they interact, and whether the person can manage them. A senior on three essential meds for heart disease, diabetes, and high blood pressure-with no sedatives or sleep aids-has much lower risk than someone on two blood pressure pills, an antidepressant, a benzodiazepine, and an OTC sleep aid.
Every medication has a purpose. But when that purpose fades, the risk remains. For seniors, the goal isn’t to avoid all drugs-it’s to take only what’s truly necessary. A simpler medicine list isn’t just safer. It’s more freedom. More confidence. More years on your own two feet.




14 Comments