It’s 3:15 p.m. You’re making tea when your neighbor suddenly slurs her words and drops her cup. She laughs it off: "Oh, I’m fine, it passed."" But what if it didn’t just pass? What if that moment was a silent alarm screaming that a stroke is coming - and you just missed the chance to stop it?
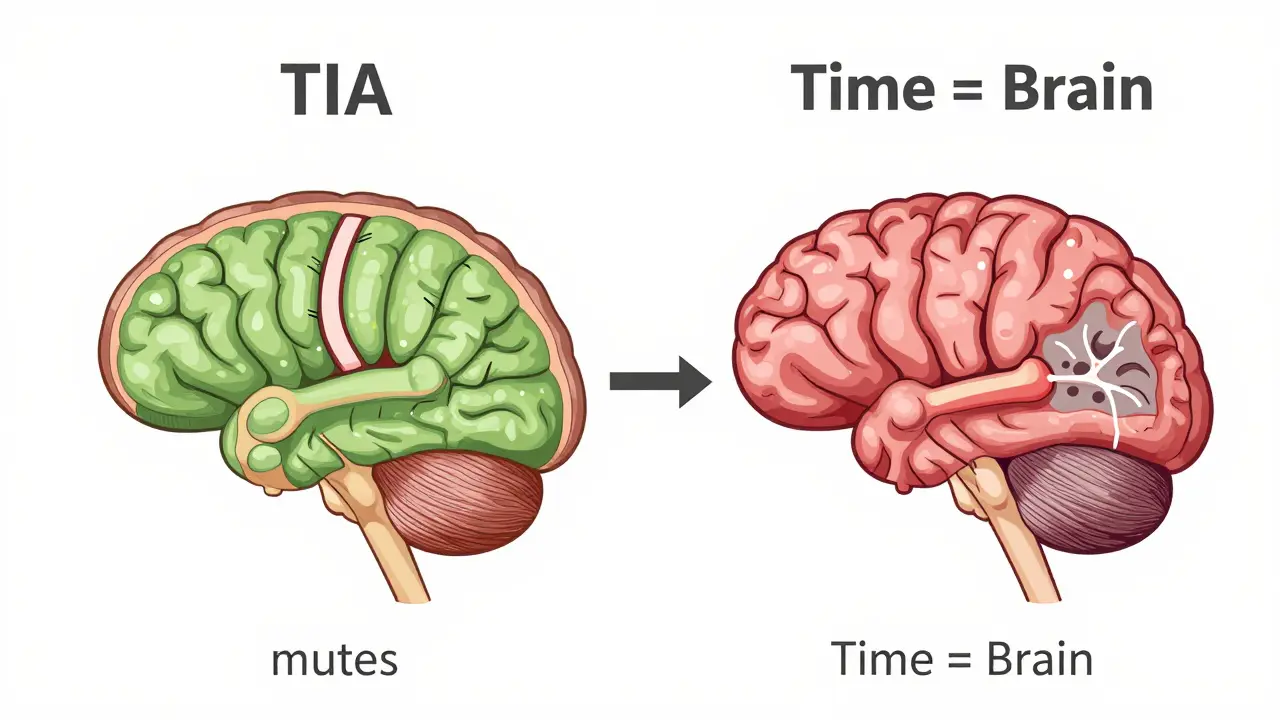
Most people think if symptoms disappear, the danger is gone. That’s the biggest mistake people make with TIA. A Transient Ischemic Attack isn’t a "mini-stroke." It’s a full-blown neurological emergency that hides in plain sight. And every minute you wait after symptoms fade is a minute closer to a disabling or deadly stroke.
What Exactly Is a TIA?
A TIA - or transient ischemic attack - happens when blood flow to part of the brain is blocked, even briefly. The symptoms? Exactly like a stroke: sudden face drooping, one arm going numb, slurred speech, vision loss, dizziness, or a severe headache with no known cause. But here’s the twist: within minutes, often less than an hour, those symptoms vanish. No weakness left. No speech trouble. No vision blur. You feel normal again.
That’s why so many people don’t call 911. They think, "It’s over. No big deal." But that’s dangerous thinking. Modern neurology no longer defines TIA by how long symptoms last. The old rule - "under 24 hours" - is outdated. Now, doctors look at the brain tissue. If there’s no permanent damage on an MRI, it’s a TIA. If there is? That’s a minor stroke. And here’s the shocking part: about 35% of people who think they had a TIA actually had a small stroke all along. Their brain was injured. They just didn’t know it.
TIA vs. Stroke: The Real Difference
At first glance, TIA and stroke look identical. Both can cause:
- One side of the face drooping when smiling
- Inability to raise both arms - one drifts downward
- Slurred, strange, or hard-to-understand speech
- Sudden vision loss in one or both eyes
- Sudden severe dizziness, loss of balance, or coordination
- A headache that feels like the worst of your life
The only difference? Time and tissue.
In a stroke, the blockage lasts long enough to kill brain cells. That damage shows up on MRI as an infarct - a dead patch of tissue. That’s permanent. You might lose movement, speech, or memory. Recovery takes months, if it happens at all.
In a true TIA, the blockage clears before tissue dies. No infarct. No permanent damage. But that doesn’t mean you’re safe. Far from it.
Here’s what the data says: 1 in 5 people who have a TIA will have a full stroke within 90 days. And half of those strokes happen within the first 48 hours. That’s not a warning. That’s a countdown.
Why "Mini-Stroke" Is a Dangerous Lie
Calling a TIA a "mini-stroke" is like calling a fire alarm a "mini-fire." It makes people think it’s harmless. It’s not.
That false label leads to delays. A CDC study found 31% of TIA patients wait more than 24 hours to seek help - because they think the symptoms are gone, so the problem is gone. But the risk doesn’t vanish with the symptoms. The underlying cause - a clot, a narrowed artery, high blood pressure - is still there. Waiting even a day can cost you your brain.
Doctors now say: "TIA is not a warning. It’s a stroke that resolved on its own." That’s not semantics. That’s life-or-death language. If your heart skips a beat and you feel fine, you still go to the ER. Same here. A TIA is your brain’s cry for help. Ignore it, and you’re gambling with your future.
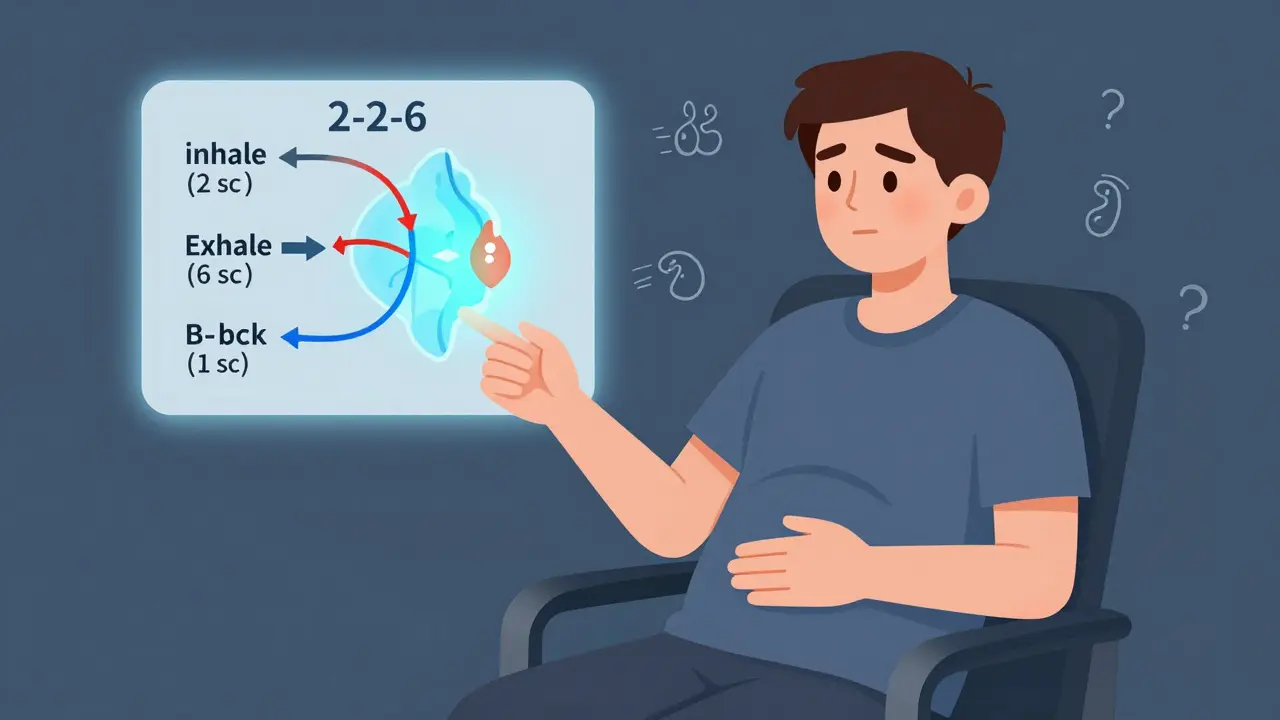
What to Do the Moment Symptoms Appear
Don’t wait. Don’t call your doctor tomorrow. Don’t "see how you feel."
Use BE FAST:
- Balance: Sudden loss of balance or coordination
- Eyes: Sudden vision changes in one or both eyes
- Face: One side drooping
- Arm: One arm weak or numb
- Speech: Slurred or strange speech
- Time: Call 911 immediately - even if symptoms disappear
That’s it. No exceptions. No "I’ll wait and see." If you see any of these, even for 2 minutes, call 911. Paramedics can start treatment in the ambulance. They can alert the hospital. They can get you to the right place - a stroke center - within minutes.
Time is brain. Every minute without blood flow kills 1.9 million neurons. That’s not a metaphor. That’s science.
How Doctors Evaluate You - Fast
When you arrive at the ER, they don’t waste time. First, they do a quick CT scan to rule out bleeding in the brain. Then, they use the ABCD2 score to predict your stroke risk:
- Age: 60 or older? +1 point
- Blood pressure: Over 140/90? +1 point
- Clinical features: Weakness on one side? +2 points. Just speech trouble? +1 point
- Duration: Symptoms lasted 60+ minutes? +2 points. 10-59 minutes? +1 point
- Diabetes: Do you have it? +1 point
Score of 4 or higher? You’re high risk. That means you need to be admitted - today. No waiting. No "follow-up next week." You get an MRI within 24 hours. That’s the gold standard. It finds tiny strokes CT scans miss.
And if you’re high risk? You’ll get aspirin within 24 hours - 325 mg - which cuts your next stroke risk by 60%. You’ll also start a high-dose statin (atorvastatin 80 mg) to stabilize plaque in your arteries. Blood pressure gets controlled fast. And if you’re eligible, you’ll get dual antiplatelet therapy: aspirin plus clopidogrel for 21-30 days. This combo reduces stroke risk by 80% if started within 48 hours.
Why Most People Miss the Warning
There’s a reason TIA gets ignored. It’s invisible. You don’t feel sick. You don’t have chest pain. You don’t break a bone. Your brain just had a hiccup - and it fixed itself. That’s why 70% of people with TIA never get evaluated properly.
But here’s what’s worse: even doctors used to think time mattered. That’s why some patients were sent home with a "wait and see" approach. Not anymore. The American Heart Association now calls TIA a neurological emergency. Every Comprehensive Stroke Center in the U.S. is required to have a TIA pathway. Hospitals that don’t evaluate high-risk TIA patients within 24 hours get fined by Medicare.
Programs like SOS-TIA at Massachusetts General Hospital now get 95% of patients seen the same day. Their 90-day stroke rate? 1.2%. Without fast care? It’s over 10%.

What Happens After the ER
Leaving the hospital after a TIA isn’t the end. It’s the beginning of prevention.
You’ll need:
- A follow-up with a neurologist or stroke specialist within 1 week
- Continuous blood pressure control (target under 140/90)
- Cholesterol management with statins - even if your numbers were "normal" before
- Diabetes control if you have it
- Stopping smoking - if you smoke, your stroke risk doubles
- Regular exercise and a low-sodium, heart-healthy diet
Some people need surgery - carotid endarterectomy or stenting - if a major artery is more than 70% blocked. Others need a heart monitor to check for atrial fibrillation, a silent arrhythmia that causes clots.
And yes - you’ll need to take medicine for the rest of your life. Not because you’re sick. Because you’re high risk. And prevention is cheaper, safer, and more effective than recovery.
The Bigger Picture
TIA isn’t just a brain problem. It’s a heart problem. A blood vessel problem. A lifestyle problem. The same forces that cause a TIA - plaque buildup, high blood pressure, inflammation - also cause heart attacks, kidney failure, and dementia.
One study found 18.9% of TIA patients die within five years - not from the TIA, but from the next heart attack or stroke. That’s why treating a TIA isn’t about fixing a single event. It’s about saving your entire future.
And the cost? A full TIA workup runs about $2,850. A single stroke? Over $21,000. And that’s just the hospital bill. Add rehab, lost wages, caregiving - and the real cost skyrockets.
There’s new tech coming too. Blood tests for GFAP - a protein released when brain cells are injured - can now tell if you’ve had a tiny stroke in under 15 minutes. AI tools are predicting stroke risk with 92% accuracy by analyzing MRI scans. But none of that matters if you don’t act when the symptoms appear.
Final Warning
If you or someone you love has sudden face drooping, arm weakness, or speech trouble - even if it’s gone in 10 minutes - call 911. No exceptions. No "I’ll call my doctor." No "I’ll wait until tomorrow."
That moment you think it’s nothing? That’s the moment your brain is screaming for help. And if you ignore it, you might not get another chance.
Don’t wait for the next stroke. Stop it before it starts.





12 Comments