You’re staring at a prescription or a search bar and wondering if Luvox (fluvoxamine) is the right call-especially for OCD or stubborn anxiety. You want a plain-English, no-drama guide: what it helps with, how to start, how long until you feel something, and what to watch for. That’s exactly what you’ll get here-plus the stuff people usually find out too late (like caffeine issues and drug interactions).
Quick expectations: Luvox sits in the SSRI family. It’s a first-line option for obsessive-compulsive disorder (OCD) and also used for depression and some anxiety disorders. It needs time-think weeks, not days. Side effects are common early but often settle. Interactions can be a big deal with fluvoxamine, so a smart setup avoids trouble. This is general information, not medical advice-work with your GP, psychiatrist, or pharmacist, especially around dosing and switches.
TL;DR: Luvox (Fluvoxamine) in Plain English
- What it’s for: Strong evidence for OCD; also prescribed for depression and some anxiety disorders. Guidelines (NICE 2022; NZF, 2025) place SSRIs as first-line for OCD, with fluvoxamine among the main options.
- How it works: It boosts serotonin signaling. Expect first changes in sleep/anxiety within 1-2 weeks, with bigger gains for OCD after 6-12 weeks.
- Typical dosing (adults): Start 50 mg at night; increase by 50 mg every 4-7 days as tolerated. Usual range: 100-300 mg/day (OCD often needs the higher end). Max varies by country; follow your prescriber.
- Common bumps: Nausea, insomnia or sleepiness, headache, sweating, sexual side effects. Early jitteriness can happen. Many effects ease after 2-4 weeks.
- Serious red flags (get urgent help): Suicidal thoughts (especially under 25s), serotonin syndrome (agitation, sweating, fever, rigid muscles), severe rash, manic switch, low sodium confusion in older adults.
- Interactions matter: Fluvoxamine strongly inhibits CYP1A2 and CYP2C19. It can spike levels of clozapine, theophylline, tizanidine, warfarin, and caffeine. MAOIs/linezolid/methylene blue are no-go.
- NZ notes (2025): Available via prescription in NZ; funding and brand availability can change. Check NZ Formulary and your pharmacist for current supply and subsidy status.
| Quick Facts (2025) | Details |
|---|---|
| Indications | OCD (strong evidence), depression, some anxiety disorders (off-label varies by country) |
| Adult starting dose | 50 mg at night; titrate by 50 mg every 4-7 days as tolerated |
| Typical effective dose | OCD: 150-300 mg/day; Depression/Anxiety: 100-200 mg/day |
| Time to effect | Sleep/anxiety shifts: 1-2 weeks; OCD response: 6-12+ weeks; full trial: 10-12 weeks at a therapeutic dose |
| Half-life | ~15-20 hours (no active metabolite) |
| Key enzyme effects | Potent inhibitor: CYP1A2, CYP2C19; Moderate: CYP2C9, CYP2D6, CYP3A4 |
| Common side effects | Nausea, insomnia/sleepiness, headache, tremor, sweating, GI upset, sexual dysfunction |
| Serious risks | Suicidality (under 25s), serotonin syndrome, bleeding risk, hyponatraemia (older adults), mania in bipolar |
| Pregnancy/breastfeeding | Discuss risks/benefits; SSRIs used in pregnancy when needed; fluvoxamine data moderate; Lactation often compatible (check NZF/LactMed) |
| Alcohol & caffeine | Avoid alcohol (sedation). Reduce caffeine (levels rise with fluvoxamine; can cause jitteriness/insomnia) |
| Do not combine | MAOIs, linezolid, methylene blue; caution with triptans, tramadol, lithium, St John’s wort |
How to Start and Use Luvox Safely (Step-by-Step)
If you’re new to SSRIs, the best results come from a slow, steady setup. Here’s a simple roadmap that lines up with NZ Formulary (NZF) practices and international labels.
Before you start: a quick checklist
- Write down every medicine and supplement you take (including caffeine habits, nicotine, and over-the-counter pain meds). Bring this to your prescriber or pharmacist.
- Flag possible interactions: clozapine, theophylline, tizanidine, warfarin, phenytoin, carbamazepine, methadone, benzodiazepines, triptans, tramadol, linezolid/methylene blue, St John’s wort.
- Screen for bipolar history (mania/hypomania), seizures, bleeding disorders, and low sodium risk (older age, diuretics).
- Pregnant, planning, or breastfeeding? Discuss the plan before starting. Often, staying on a stable effective SSRI is safer than switching mid-pregnancy.
- Set up a follow-up schedule: 2 weeks (tolerability), 6 weeks (dose check), 10-12 weeks (response at target dose).
Week-by-week dosing idea (work with your prescriber)
- Week 1: 50 mg at night with a light snack if nausea is an issue.
- Week 2: 100 mg/day (often split 50 mg morning, 50 mg night if daytime sedation or nausea is a problem; some tolerate it all at night).
- Week 3-4: 150-200 mg/day if OCD symptoms persist and side effects are manageable.
- Weeks 5-8: Push toward 200-300 mg/day for OCD if needed and tolerated. Go slower if you’re sensitive.
Note: Some markets have controlled-release (CR) versions; in NZ, immediate-release tablets are most common. Follow your local label. Maximum doses vary-your prescriber will set the ceiling.
How long to give it?
- OCD: Plan a full 10-12 week trial at a therapeutic dose before judging response. SSRIs often need higher doses for OCD than for depression.
- Depression/anxiety: Expect meaningful change by weeks 4-6. If nothing changes by week 6 at a fair dose, reassess.
If you miss a dose
- Take it when you remember unless it’s close to the next dose. Don’t double up.
- Set a phone reminder. Consistency keeps your brain chemistry steadier-and side effects milder.
Stopping or switching
- Taper over weeks, not days. A common approach: reduce by 50 mg every 1-2 weeks, slower if withdrawal symptoms show up (dizziness, “brain zaps,” irritability).
- Switching from/to MAOIs needs a 14-day washout (longer from fluoxetine to MAOIs). This is safety-critical-get clear instructions in writing.
Real-life examples
- University student with OCD rituals: Started 50 mg nightly, then 100 mg week 2, 150 mg week 3. First real gains at 8 weeks alongside ERP therapy. Settled at 200 mg day with minimal nausea.
- New parent with intrusive thoughts: Felt wired on morning doses. Moving most dose to night cut daytime jitteriness. Sleep improved once caffeine was halved.
- Middle-aged man on theophylline for asthma: Switched to a different SSRI due to interaction risk; pharmacist flagged this before starting.
Side Effects, Red Flags, and What to Do
Most side effects show up early and fade. Your job is to know what’s manageable at home and what needs help.
Common, usually temporary (first 1-3 weeks)
- Nausea or stomach upset: Take with food or at night. Ginger tea can help. If it’s rough, ask about slower titration or using an anti-nausea med briefly.
- Insomnia or sleepiness: Shift dosing time. If wired at night, move part of the dose to morning; if sleepy in the day, move it to bedtime.
- Headache, sweating, mild tremor: Often settle. Hydration and light exercise help. Mention tremor if it persists-it may relate to dose or interactions.
- Sexual side effects (low libido, delayed orgasm): Very common across SSRIs. Options: dose timing, dose adjustment, or targeted add-ons-talk to your prescriber.
Less common but important
- Increased anxiety/jitteriness in week 1-2: This “activation” tends to pass. Slow the titration or add a short-term calming strategy if needed.
- Weight change: Modest shifts can happen over months. Track trends with your GP if concerned.
- Bleeding risk: SSRIs can raise bleeding risk, especially with NSAIDs, aspirin, anticoagulants. Report easy bruising or nosebleeds.
- Low sodium (hyponatraemia): More likely in older adults or if you’re on diuretics. Watch for fatigue, confusion, falls-urgent check if suspected.
Red flags-seek urgent care
- Serotonin syndrome: Agitation, sweating, fever, shivering, diarrhea, rigid muscles, confusion. Higher risk when combined with MAOIs, linezolid, methylene blue, tramadol, or multiple serotonergic meds.
- Suicidal thoughts or behavior changes: SSRIs carry a boxed warning, especially under 25s. Don’t wait-contact your prescriber or emergency services.
- Mania/hypomania: Racing thoughts, less sleep, impulsive behavior-flag for possible bipolar spectrum and adjust treatment.
- Severe allergic reactions: Rash with fever, swelling, or breathing trouble-get help fast.
Withdrawal symptoms (if stopped abruptly)
- Dizziness, electric-shock sensations, nausea, irritability, sleep problems. Prevent with a slow taper. If symptoms appear, pause the taper or step back up and slow it further.
Interactions, Special Situations, and NZ-Specific Notes
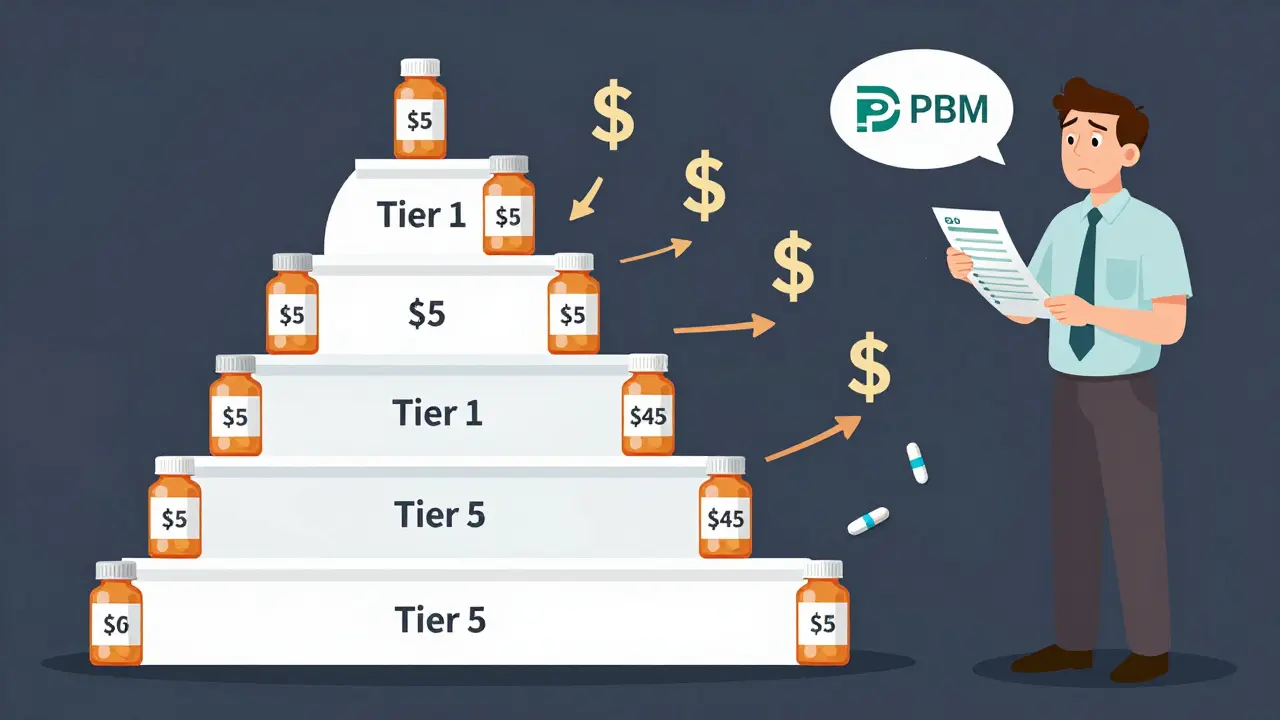
Fluvoxamine’s interaction profile is its biggest gotcha. It strongly inhibits CYP1A2 and CYP2C19, and to a lesser extent CYP2C9, CYP2D6, and CYP3A4. Translation: it can raise levels of other medicines that use those enzymes. A pharmacist review is gold.
High-risk interactions to avoid or adjust
- MAOIs (e.g., phenelzine), linezolid, methylene blue: Contraindicated. Risk of serotonin syndrome. Respect washout periods.
- Clozapine, olanzapine: Levels can rise-risk of sedation, seizures (clozapine). Often choose a different SSRI or monitor closely.
- Tizanidine: Contraindicated in some countries-risk of profound hypotension and sedation.
- Theophylline: Levels can spike-arrhythmia/seizure risk. Usually avoid or reduce and monitor levels.
- Warfarin and other anticoagulants/antiplatelets: Increased bleeding risk. Closer INR and clinical monitoring needed.
- Triptans, tramadol, lithium, St John’s wort: Serotonin syndrome risk-use caution, monitor, or avoid combos.
- Benzodiazepines (e.g., diazepam): Levels may increase-watch sedation; dose adjust.
Caffeine, alcohol, nicotine
- Caffeine: Fluvoxamine can raise caffeine levels. Cut coffee/energy drinks by half to start. If you get jittery or can’t sleep, reduce more.
- Alcohol: Increases drowsiness and accident risk. Best to avoid, especially early on.
- Smoking: Tobacco smoke induces CYP1A2. If you quit smoking while on clozapine or theophylline and take fluvoxamine, levels of those meds can jump. Keep your team in the loop during any quit attempt.
Special populations
- Adolescents/young adults: Higher risk of suicidal thoughts early on; close follow-up is standard. Fluvoxamine is used for pediatric OCD in some countries-check local approvals.
- Older adults: Start low, go slow. Higher risk of low sodium and bleeding. Consider sodium checks after starting or dose changes.
- Liver impairment: Lower starting doses and slower titration; fluvoxamine is hepatically metabolized.
- Pregnancy: SSRIs are widely used when benefits outweigh risks. Third-trimester exposure can cause transient neonatal symptoms (jitteriness, feeding issues). Decisions should be individualized; NZF/Medsafe guidance supports shared decision-making.
- Breastfeeding: Many SSRIs are compatible; fluvoxamine appears in milk at low levels. Monitor baby’s feeding and sleep. Confirm with NZF or LactMed.
NZ-specific notes (2025)
- Availability/funding: Brand and subsidy status can change. Your pharmacist and the NZ Formulary (NZF) have the latest. If not funded, ask about generic pricing or alternatives.
- Therapy access: For OCD, exposure and response prevention (ERP) therapy is as important as medication. Your GP can refer through local services; private options exist across NZ.
- Monitoring: Many practices offer phone or virtual follow-ups after starting an SSRI-ask for this when you pick up the script.

Quick Cheats, Comparisons, and FAQ
Best for / Not for
- Best for: OCD where higher SSRI doses are needed; people who can manage caffeine and medication interactions; those who prefer bedtime dosing due to mild sedation.
- Not for: Complex polypharmacy with high-risk CYP1A2 substrates (clozapine, theophylline, tizanidine); those who can’t reduce caffeine; people with prior severe SSRI reactions where another class might be better.
Luvox vs other SSRIs (rule-of-thumb)
- For OCD: Fluvoxamine, sertraline, and fluoxetine are all solid. If interactions are a headache, sertraline often plays nicer.
- For activation/anxiety early on: Consider slower titration. If you needed very low starting doses in the past, mention it-your prescriber can match that style.
- If sexual side effects are a deal-breaker: This is a class effect. Some people do better with bupropion add-on or a different strategy; raise it early so you have options.
Pro tips
- Use a symptom tracker. For OCD, track time spent on rituals and distress ratings weekly; for mood/anxiety, use the same time of day and same scale each week.
- Change one thing at a time. If you’re starting Luvox, don’t also overhaul caffeine, sleep, and supplements in the same week-you won’t know what helped or hurt.
- ERP + SSRI beats either alone for many people with OCD. If therapy feels overwhelming, ask for a stepped approach.
- Tell your pharmacist you’re on fluvoxamine before buying cold/flu meds. They’ll steer you away from risky combos.
Mini-FAQ
- How long until I know if it’s working? Some easing of anxiety/sleep can show in 1-2 weeks. For OCD, give it 10-12 weeks at a target dose before calling it.
- Can I drink coffee? Yes, but cut back. Fluvoxamine boosts caffeine levels-too much can make you edgy and sleepless.
- Is weight gain guaranteed? No. Some gain a little over months, some don’t. Track and adjust lifestyle early.
- What if I feel worse at first? Early activation happens. Slow the titration and check in. Short-term support (like sleep strategies) can help.
- Is it safe in pregnancy? Many people continue an SSRI in pregnancy when benefits are clear. Discuss timing, dosing, and alternatives with your team.
- Do I need blood tests? Not routinely. Older adults or those at risk may get sodium checks. If on interacting drugs (like warfarin), closer monitoring applies.
Next steps and troubleshooting
- If you’re just starting: Book check-ins at 2, 6, and 12 weeks. Put side effects and wins into a simple note app.
- If mild side effects bug you: Don’t abandon ship in week 1. Ask about splitting dose, moving to night, or slower increases.
- If nothing changes by week 6: Confirm the dose is therapeutic for your condition (OCD often needs 150-300 mg). Consider pushing the dose, therapy integration, or switching.
- If you take multiple medicines: Schedule a meds review with your pharmacist; ask specifically about CYP1A2/CYP2C19 interactions.
- If you’re travelling: Keep meds in original packaging in your carry-on. Time zones? Take your next dose roughly 24 hours after the last, then adjust by 1-2 hours per day.
- If you might stop: Taper slowly. A rough guide is 10-25% dose reduction every 1-2 weeks, slower if you feel discontinuation symptoms.
Why trust this? The details above align with the New Zealand Formulary (NZF, accessed 2025), Medsafe data sheets, the FDA label for fluvoxamine, NICE guidelines for OCD (2022), and Cochrane reviews on SSRIs in OCD and depression. Those sources consistently support SSRIs as first-line for OCD, the need for higher dosing and longer trials for OCD than for depression, and careful interaction management for fluvoxamine.
Final note: If anything here clashes with your prescriber’s plan, follow the plan you agreed on together. They know your full history. Bring your questions-good care is a conversation.




20 Comments