Alcohol & Medication Interaction Checker
Check if your medications interact with alcohol and get specific safety information.
Every year, thousands of people end up in emergency rooms because they didn’t realize that a drink with their medication could be deadly. It’s not just about getting drunk. It’s about what happens when alcohol meets your pills - whether they’re prescription, over-the-counter, or even herbal. The risk isn’t theoretical. It’s happening right now, to people who think they’re being careful.
Why Alcohol and Medications Don’t Mix
Alcohol doesn’t just sit in your body quietly. It gets processed by your liver - the same place where most medications are broken down. When you drink while taking meds, your liver gets overwhelmed. It can’t handle both at once. That means your medication might stay in your system too long, or break down too fast. Either way, things go wrong.Some drugs get stronger when mixed with alcohol. Others stop working. And some turn toxic. This isn’t guesswork. It’s science. The National Institute on Alcohol Abuse and Alcoholism says nearly 40% of adults took a medication last year that could react badly with alcohol. That’s almost half of us.
The Deadliest Combinations
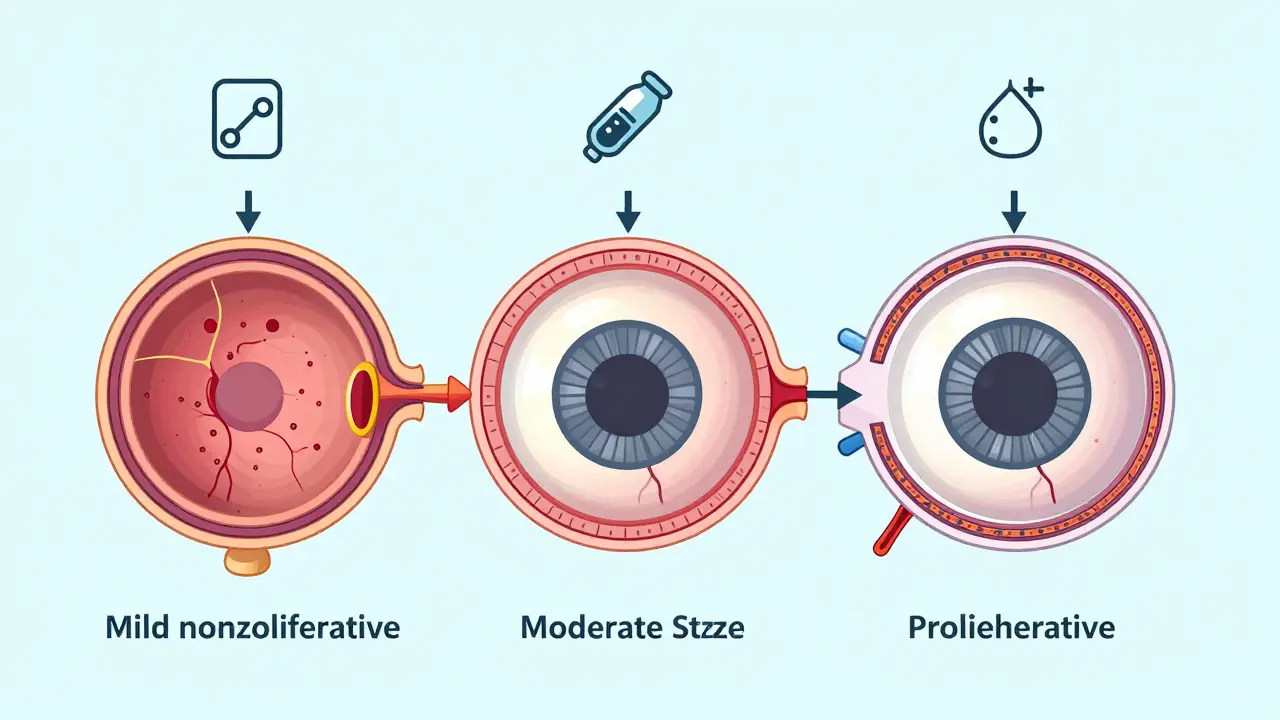
Not all meds are equal when it comes to alcohol. Some combinations are far more dangerous than others.Opioids - like oxycodone, hydrocodone, or methadone - are among the most lethal. When alcohol joins them, your breathing slows down. A lot. The FDA has documented cases where people died because alcohol caused a sudden, massive release of the opioid into their bloodstream. In 2020, 20% of opioid overdose deaths involved alcohol. That’s not a coincidence. It’s a pattern.
Benzodiazepines - such as Xanax, Valium, or Klonopin - are meant to calm you down. Alcohol does the same thing. Together, they’re like pressing the brake and the gas at the same time. Your central nervous system shuts down. A 2019 study found that mixing these drugs with alcohol increases overdose risk by 24 times. That’s not a typo.
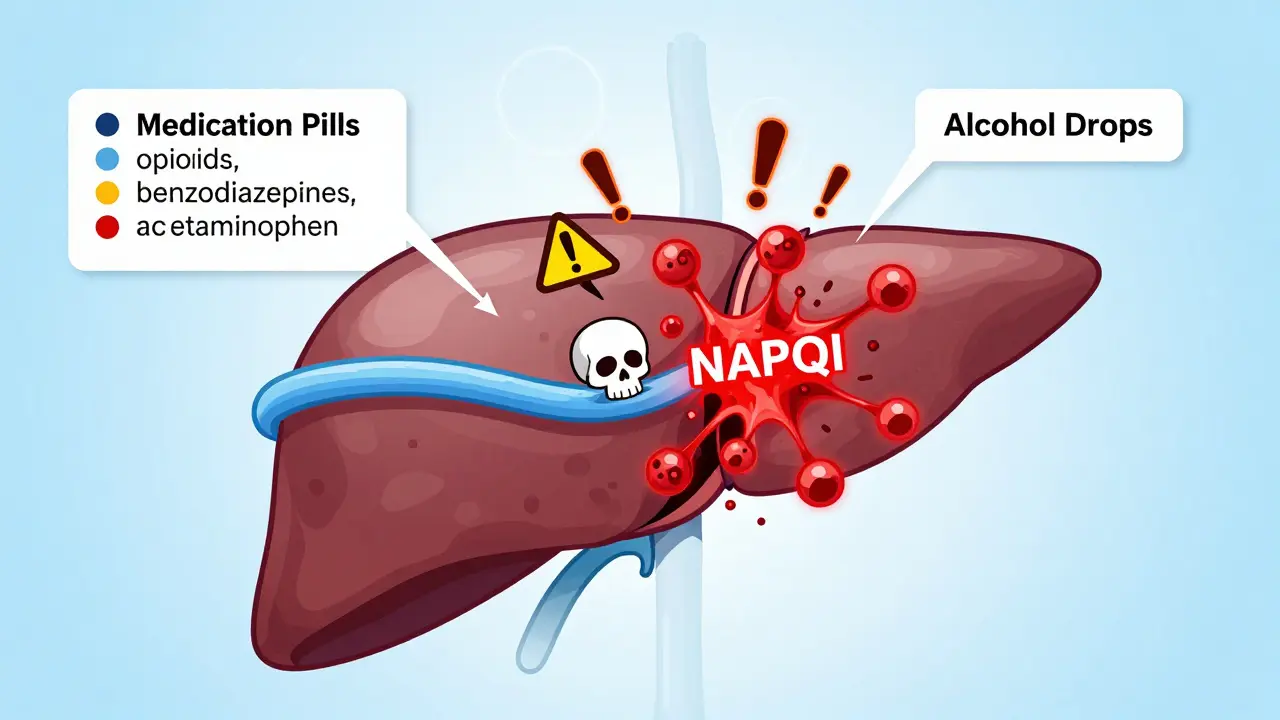
Acetaminophen (Tylenol) is another silent killer. People take it for headaches or fever, not thinking twice. But when you drink while taking it, your liver starts producing a poison called NAPQI. Your body usually neutralizes it with glutathione. But alcohol depletes that defense. The result? Acute liver failure. The FDA says acetaminophen overdoses - often tied to alcohol - cause over 56,000 ER visits and nearly 500 deaths every year in the U.S. alone.
Metronidazole (Flagyl) is an antibiotic used for infections. If you drink while taking it, you’ll get a reaction called disulfiram-like response: nausea, vomiting, flushing, rapid heartbeat, and severe dizziness. It’s not just uncomfortable. It can send you to the hospital. The Illinois Poison Center says you need to wait at least 72 hours after your last dose before even a sip of alcohol.
Other High-Risk Meds You Might Not Realize
You might think, “I only take one or two pills. It’s not a big deal.” But here’s what else you should avoid mixing with alcohol:- NSAIDs - like ibuprofen or naproxen. These already irritate your stomach lining. Add alcohol, and your risk of internal bleeding goes up 3 to 5 times.
- Antihistamines - such as Benadryl. They make you sleepy. Alcohol makes you sleepier. Together, you could pass out, fall, hit your head, or stop breathing.
- ADHD meds - like Adderall or Ritalin. They speed you up. Alcohol slows you down. This clash stresses your heart. It can cause irregular heartbeat, high blood pressure, and even heart attack.
- SSRIs - antidepressants like Prozac or Zoloft. Alcohol can make depression worse, reduce the drug’s effect, and increase dizziness or drowsiness.
- Blood pressure meds - alcohol can drop your blood pressure too far, especially when standing up. That’s why older adults are at risk for falls.
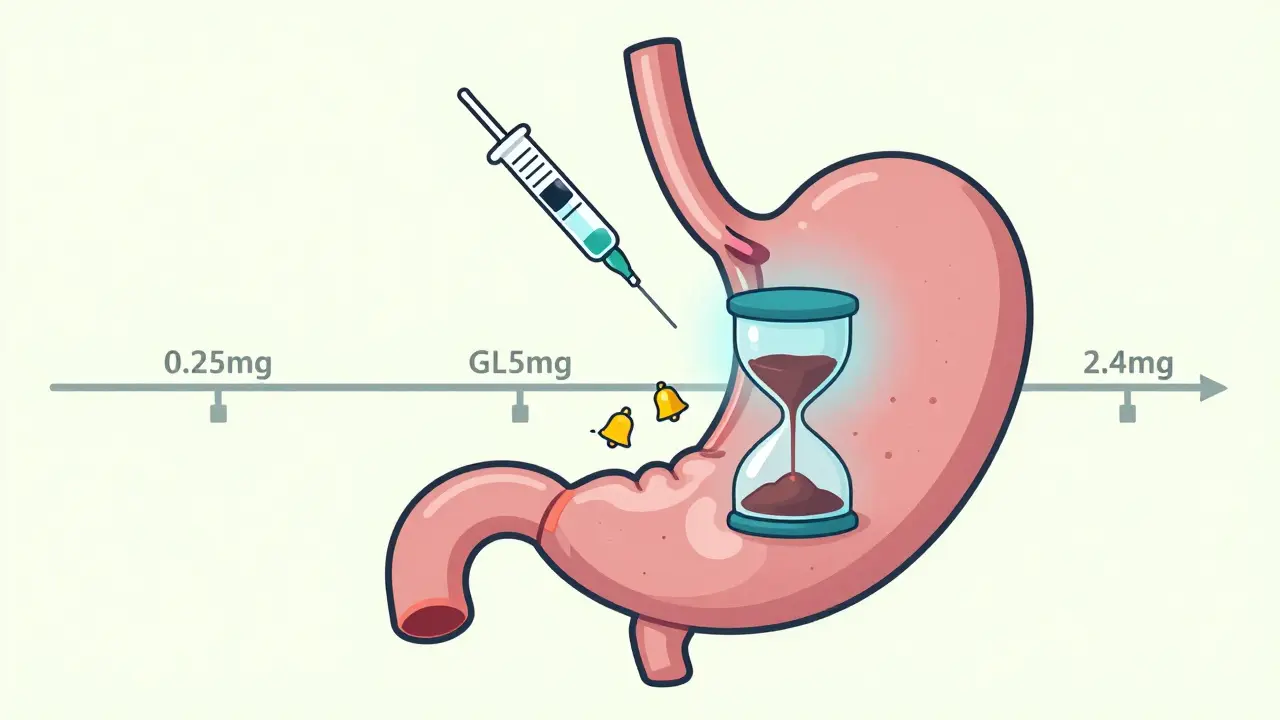
- Diabetes meds - sulfonylureas (like glipizide) can cause dangerous drops in blood sugar. Alcohol blocks your liver from releasing glucose. That combo can lead to unconsciousness or seizures. Even metformin carries a risk of lactic acidosis if you drink too much.
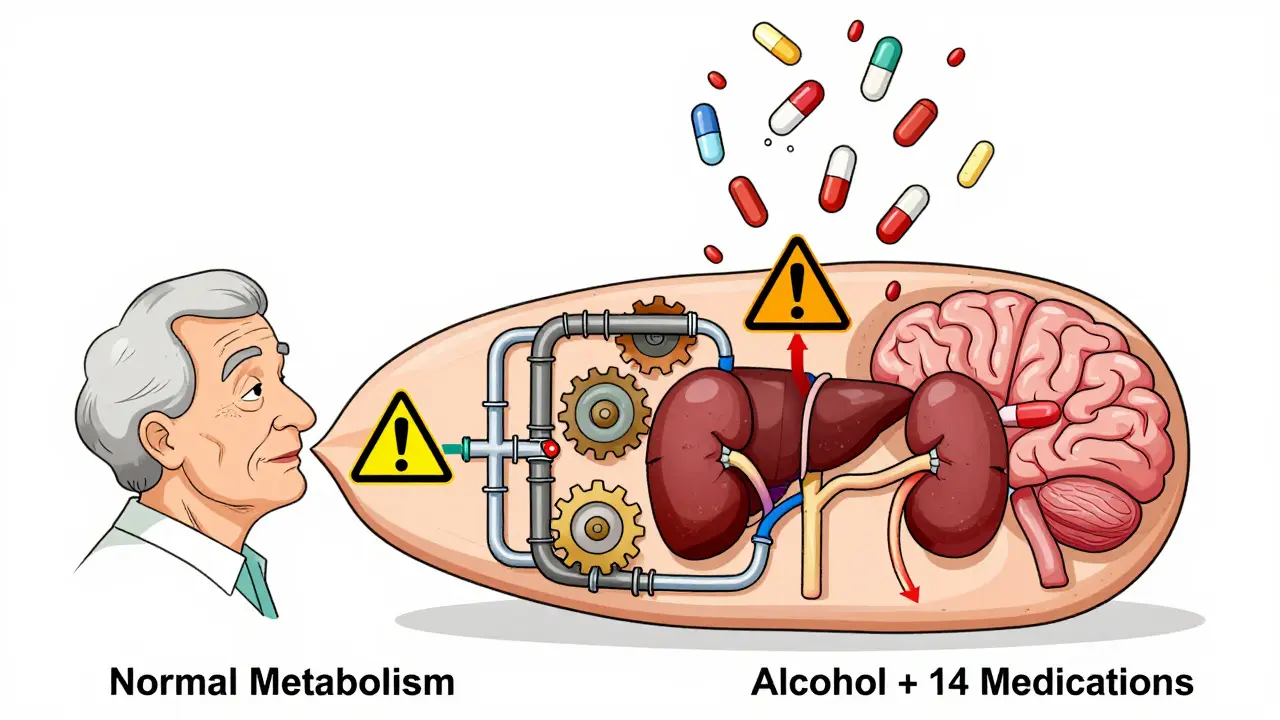
Why Older Adults Are at Higher Risk
If you’re 65 or older, your body doesn’t handle alcohol the way it used to. You have less water in your body, so alcohol stays concentrated. Your liver slows down. Your kidneys don’t clear drugs as fast. And you’re likely taking more meds - an average of 14 prescriptions per year, according to CDC data.The Beers Criteria, updated in 2019, lists 30 medications that are risky for older adults when combined with alcohol. That includes benzodiazepines, muscle relaxants, and first-gen antihistamines. These aren’t just side notes. They’re red flags.
And here’s the kicker: most older adults don’t even know they’re at risk. A 2022 study in JAMA Internal Medicine found that only 35% of primary care doctors routinely ask patients about alcohol use during medication visits. That means you’re probably not being warned - even if you should be.
Women and Alcohol: A Different Risk
Women process alcohol differently than men. They have less body water and lower levels of the enzyme that breaks down alcohol in the stomach. That means if a man and a woman drink the same amount, the woman ends up with a higher blood alcohol level. That makes every interaction worse.That’s why women are more likely to suffer liver damage from alcohol and acetaminophen. It’s also why they’re more vulnerable to falls, accidents, and overdose when mixing meds and drinks.
What About “Just One Drink”?
People often say, “I only have one glass of wine with dinner.” But “one drink” doesn’t mean safe. One standard drink is:- 12 oz of beer
- 5 oz of wine
- 1.5 oz of spirits
That’s it. But even that tiny amount can be dangerous if you’re on certain meds. For example, with metronidazole, even a sip can trigger a reaction. With opioids or benzodiazepines, one drink can be enough to stop your breathing.
There’s no “safe” amount for high-risk combinations. The only safe choice is none.

What Should You Do?
You don’t need to guess. Here’s what actually works:- Read the label. The FDA requires warning labels on about 100 prescription and 700 over-the-counter drugs. If it says “avoid alcohol,” don’t.
- Ask your pharmacist. They’re trained to catch these interactions. When you pick up a new script, ask: “Can I drink alcohol with this?” Don’t assume they’ll tell you - ask.
- Check your meds regularly. Your list changes. A new antibiotic, a new painkiller, a new sleep aid - each one could change the risk.
- Use the AUDIT-C screen. It’s a simple 3-question tool doctors use to spot risky drinking. If you’re on high-risk meds, ask your doctor to use it.
- Wait it out. After finishing metronidazole, wait 72 hours. After stopping a benzodiazepine, wait at least 24-48 hours. For opioids, wait until the drug is completely out of your system - which can take days.
The Bigger Picture
This isn’t just about individual choices. It’s about systems failing. Pharmacies don’t always flag interactions. Doctors don’t always ask. Patients don’t always know. But change is coming.Electronic health records now have hard-stop alerts. If a doctor tries to prescribe oxycodone to someone with a history of alcohol use, the system blocks it unless they override it. The FDA now requires new extended-release opioids to be tested with alcohol before approval. And in 2023, the CDC launched a $2.5 million public awareness campaign: “Alcohol and Medicine Don’t Mix.”
Still, the biggest barrier is silence. People don’t talk about it. They’re embarrassed. They think it’s their fault. But it’s not. It’s a system problem - and it’s fixable.
Final Thought
You take your meds because you want to feel better. You drink because you want to relax. But when they meet, the result isn’t relaxation. It’s risk. It’s hospital visits. It’s death.You don’t have to give up everything. But if you’re on any of these medications, you need to know: alcohol isn’t just a drink. It’s a drug. And some drugs don’t play nice with others.
Ask. Read. Wait. Protect yourself. It’s not about being perfect. It’s about being informed.
Can I have one drink while taking antibiotics?
It depends on the antibiotic. With metronidazole, tinidazole, or some sulfa drugs, even one drink can cause severe nausea, vomiting, flushing, and a fast heartbeat. With others like amoxicillin or azithromycin, alcohol won’t reduce the drug’s effectiveness, but it can worsen side effects like stomach upset or dizziness. When in doubt, avoid alcohol until you finish the course and check with your pharmacist.
Does alcohol make painkillers less effective?
Not always - but it often makes them more dangerous. Alcohol doesn’t usually reduce the pain-relieving effect of opioids or acetaminophen. Instead, it increases the risk of overdose, liver damage, or stomach bleeding. So while the pain relief might stay the same, your risk goes way up. That’s not worth it.
Is it safe to drink alcohol while on antidepressants?
It’s not recommended. Alcohol can make depression and anxiety worse, reduce the effectiveness of SSRIs, and increase drowsiness or dizziness. Even if you feel fine, alcohol interferes with brain chemistry in ways that can undo progress in therapy. If you’re treating depression, limiting or avoiding alcohol gives you the best shot at recovery.
What should I do if I accidentally mixed alcohol with my medication?
If you feel dizzy, nauseous, have trouble breathing, or feel like you might pass out, call emergency services immediately. For less severe symptoms like mild drowsiness or upset stomach, stop drinking, drink water, and monitor yourself. Contact your pharmacist or doctor to assess risk. Don’t wait - even if you feel okay now, some reactions can be delayed.
Are herbal supplements safe with alcohol?
No - and they’re often overlooked. Supplements like kava, valerian, and St. John’s wort can cause drowsiness or liver damage when mixed with alcohol. Melatonin can increase dizziness. Even common herbs like echinacea or garlic can interact with blood thinners or blood pressure meds. Always treat herbal supplements like real medicine - and ask your pharmacist before combining them with alcohol.
Can I drink the day after taking a strong painkiller?
It depends on the drug. For short-acting painkillers like oxycodone or hydrocodone, the drug may still be in your system 12-24 hours after your last dose. For extended-release versions, it can linger for days. If you’re unsure, wait at least 48 hours. When you’re on opioids, even one drink after a day can still be risky. When in doubt, skip it.
Why don’t doctors always warn me about alcohol interactions?
Many don’t ask. A 2022 study found only 35% of primary care doctors routinely screen patients for alcohol use when prescribing medications. Time constraints, assumptions that patients won’t drink, or lack of training can all play a role. That’s why it’s up to you to ask. Don’t wait for them to bring it up - bring it up yourself.
Knowing the risks isn’t about fear. It’s about control. You’re not powerless. You can protect yourself - one question, one label, one choice at a time.





10 Comments