Antibiotic-Probiotic Timing Calculator
How Timing Matters
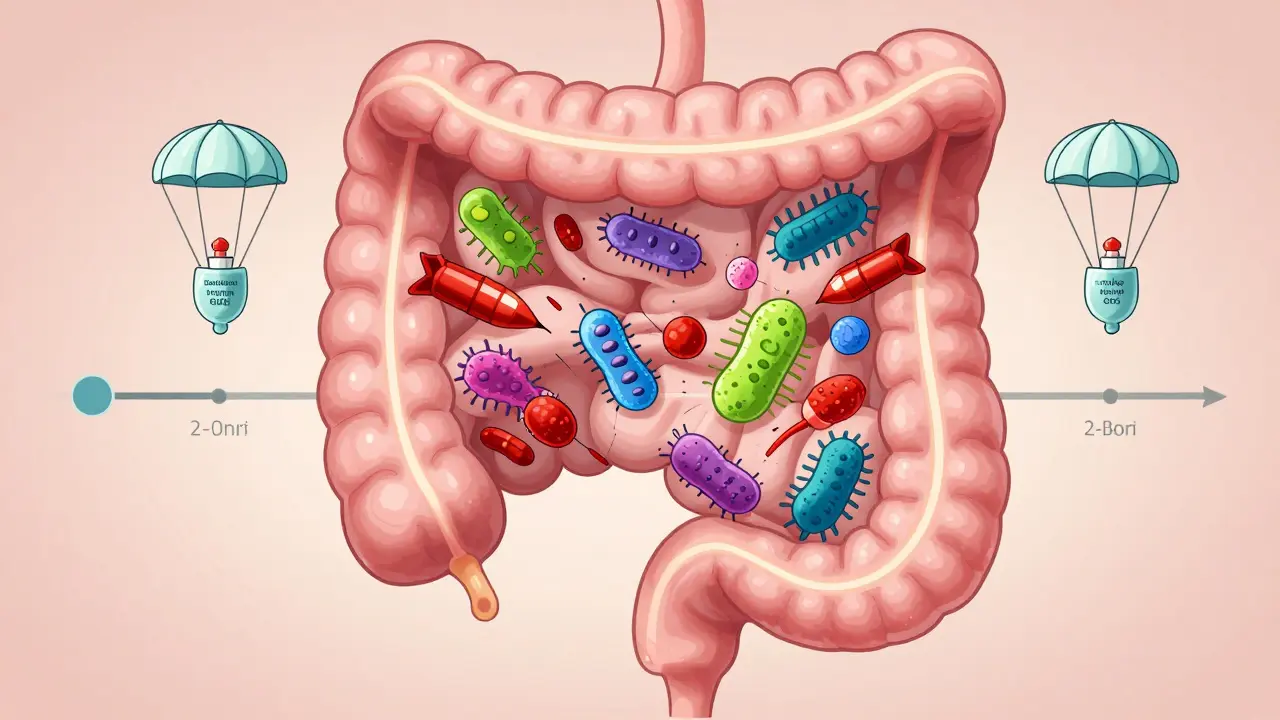
Antibiotics kill harmful bacteria but also wipe out beneficial gut bacteria. To prevent diarrhea and C. diff infection, take probiotics 2-3 hours after your antibiotic dose. This gives the antibiotic time to work while allowing probiotics to establish themselves in your gut.
Calculate Your Optimal Timing
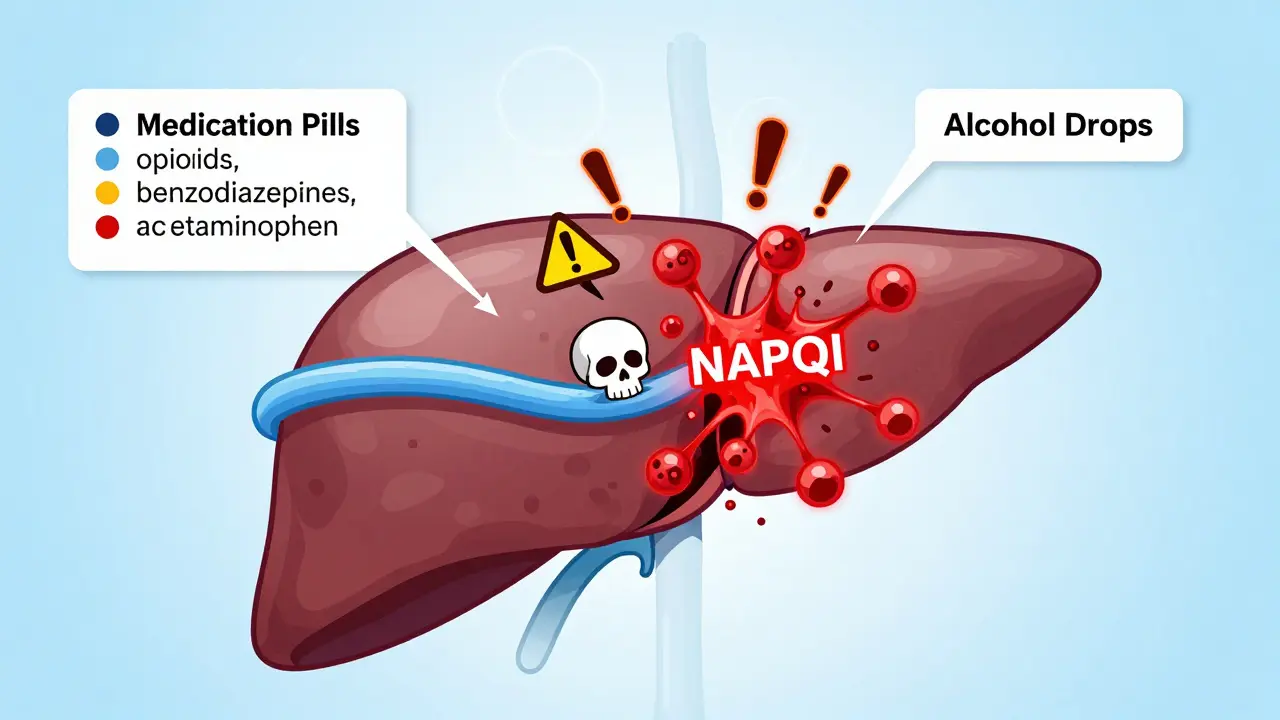
When you're on antibiotics, your gut knows it. You might feel bloated, crampy, or end up with watery stools that last days after you finish your prescription. This isn’t just bad luck-it’s science. Antibiotics don’t just kill the bad bacteria causing your infection. They wipe out the good ones too. And when your gut microbiome gets thrown off balance, digestive trouble follows. About 5-30% of people on antibiotics get antibiotic-associated diarrhea (AAD). For some, it’s mild. For others, it’s Clostridioides difficile (C. diff), a dangerous infection that can land you in the hospital.
Why Probiotics Help When You’re on Antibiotics
Probiotics are live bacteria and yeasts that are meant to restore the good bugs in your gut. They’re not magic pills, but they do have solid evidence backing them up when used correctly. A major 2020 Cochrane review looked at 2454 people taking antibiotics and found that those who took probiotics had just a 3.1% chance of developing C. diff diarrhea. Those who didn’t take probiotics? 11.6%. That’s more than a 70% drop in risk. The most effective strains? Lactobacillus rhamnosus GG and Saccharomyces boulardii. Studies show S. boulardii can cut the risk of antibiotic diarrhea in half. L. rhamnosus GG, found in brands like Culturelle, has been tested in dozens of trials and consistently shows benefit. These strains stick around in your gut longer, fight off harmful bacteria, and help your lining heal faster. They work by crowding out bad bugs, producing natural antimicrobials, and calming gut inflammation. Think of them as reinforcements arriving after a battle-helping your gut recover instead of staying in chaos.Which Probiotic Strains Actually Work?
Not all probiotics are created equal. Just because a product says “probiotic” doesn’t mean it will help with antibiotics. The strain matters more than the brand.- Lactobacillus rhamnosus GG - Best overall for preventing diarrhea. Proven in children and adults. Found in Culturelle and other top brands.
- Saccharomyces boulardii - A yeast, not a bacteria. Works even when taken with antibiotics. Reduces AAD risk by about 50%. Available as Florastor.
- Bifidobacterium lactis - Helps with bloating and gas. Often paired with L. acidophilus in multi-strain formulas.
- Lactobacillus acidophilus - Common in yogurt and supplements, but alone it’s less effective for antibiotic protection.
- Multi-strain blends - Can be helpful, but only if they include proven strains like GG or S. boulardii. Many blends are just marketing.
When and How to Take Them
Timing is everything. If you take your probiotic at the same time as your antibiotic, the antibiotic will kill the probiotic before it can do anything. That’s like sending firefighters into a burning house while the arsonist is still lighting matches. Experts recommend taking your probiotic 2 to 3 hours after your antibiotic dose. This gives the antibiotic time to do its job without wiping out your probiotic. You can take the probiotic with food or on an empty stomach-depends on the product. Acid-resistant strains like S. boulardii can handle stomach acid better, so they’re more forgiving. Take probiotics every day during your antibiotic course and keep going for 1 to 2 weeks after you finish. Your gut doesn’t bounce back overnight. Stopping too soon means you miss the recovery window. Dose-wise, aim for 5 to 10 billion CFUs (colony-forming units) per day. Higher doses aren’t necessarily better. In fact, too much too soon can make bloating worse.What You Might Feel at First
Some people notice more gas, bloating, or even constipation when they start probiotics. This isn’t a sign they’re not working-it’s a sign your gut is adjusting. These symptoms usually fade within a few days. If they don’t, lower your dose or switch strains. A 2023 Cleveland Clinic report says people with sensitive guts or IBS may react more strongly. If you’ve had bad reactions to probiotics before, start with half a dose. Give it 3 days. If things get worse, stop. Don’t assume “natural” means safe. Probiotics are live organisms. In rare cases, they can cause infections-especially in people with weakened immune systems, those who’ve had recent surgery, or those with central lines or catheters. There have been documented cases of Lactobacillus causing bloodstream infections and Saccharomyces boulardii causing fungal infections in vulnerable patients.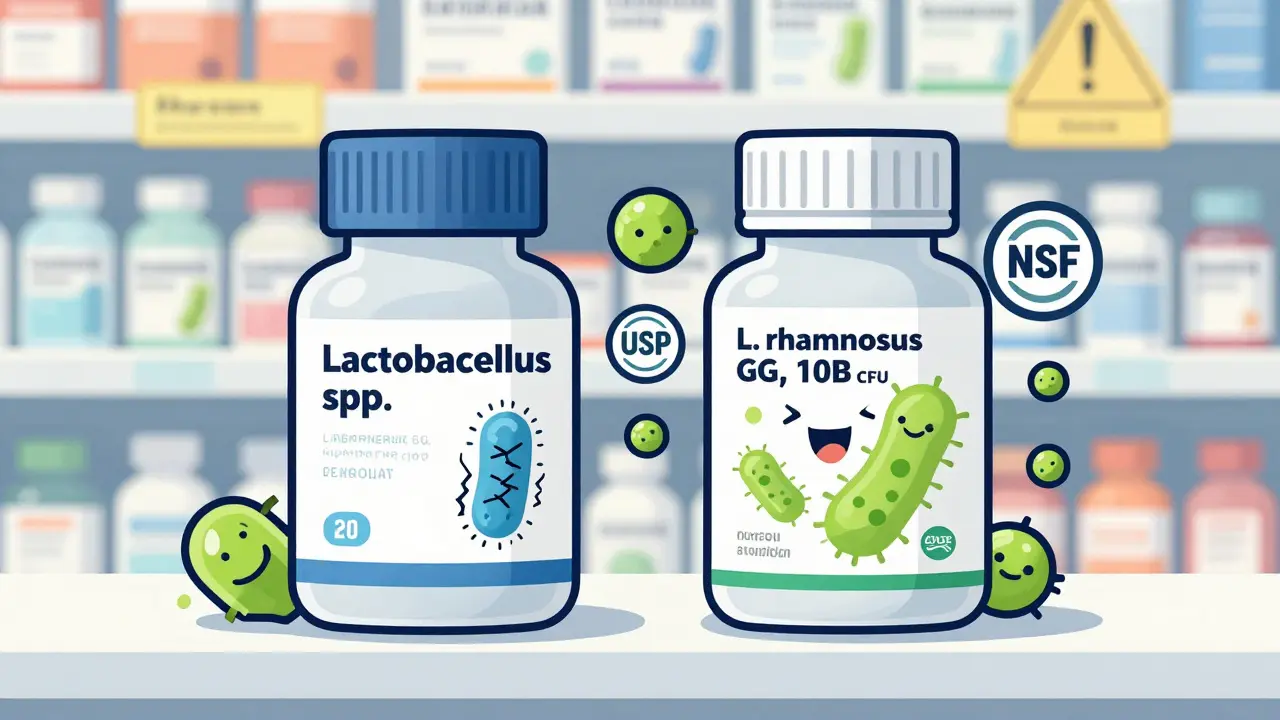
The Big Problem: Unregulated Supplements
Here’s the ugly truth: most probiotics in the U.S. are sold as dietary supplements. That means the FDA doesn’t test them for safety or effectiveness before they hit store shelves. Manufacturers don’t have to prove they work. Independent testing by ConsumerLab in 2022 found:- 30% of probiotics didn’t contain the number of live organisms listed on the label.
- 15% had extra, unlisted bacteria or fungi-some potentially harmful.
- Many products were expired or stored improperly, killing the good bugs before you even opened the bottle.
- List the exact strain (e.g., Lactobacillus rhamnosus GG, not just “Lactobacillus”)
- Provide CFU count at expiration date (not just at time of manufacture)
- Have third-party verification (USP, NSF, or ConsumerLab seal)
- Refrigerate if required (many strains die at room temperature)
Who Should Avoid Probiotics?
Probiotics aren’t for everyone. Avoid them if you:- Have a weakened immune system (HIV, chemotherapy, organ transplant)
- Are critically ill or in the ICU
- Have a central line or catheter
- Have short bowel syndrome
- Are recovering from major surgery
What About Yogurt and Fermented Foods?
Yogurt, kefir, sauerkraut, and kimchi contain live cultures-but they’re not reliable for preventing antibiotic diarrhea. Why? The strains in food aren’t standardized. The number of live bacteria varies wildly by brand, batch, and storage. Plus, most fermented foods don’t contain enough of the specific strains proven to help (like GG or S. boulardii). You can eat them for general gut health, but don’t rely on them during antibiotic therapy. If you want protection, use a targeted supplement with proven strains.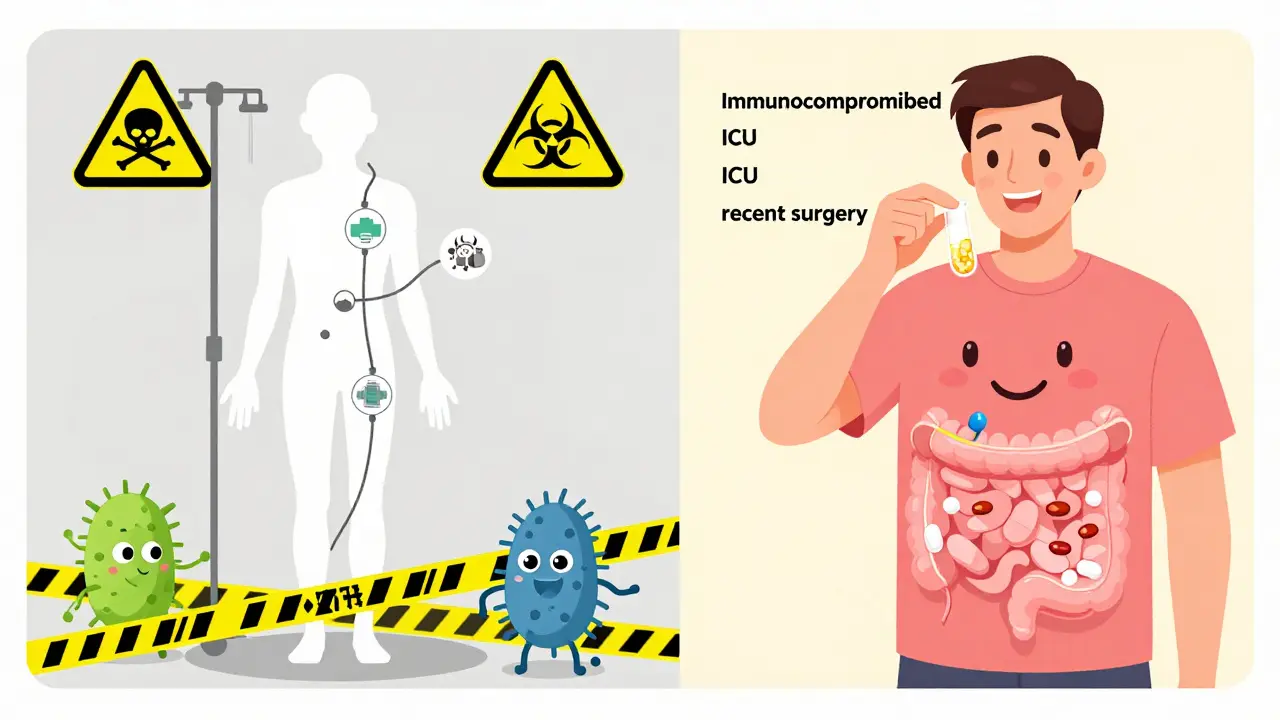
Real People, Real Results
On Amazon, Culturelle (L. rhamnosus GG) has over 12,500 reviews and a 4.2-star rating. Many users say: “Took this with amoxicillin-no diarrhea.” “My son got sick every time he took antibiotics. This time, zero issues.” But not everyone has success. About 15% of negative reviews say “no effect.” Others report worse bloating. This isn’t failure-it’s individuality. Your gut is unique. What works for one person might not work for you. If one strain doesn’t help, try another. Reddit users in r/Probiotics often share timing tips: “I take mine at 8 PM, antibiotic at 8 AM. No issues.” “Started with half a pill. Gave my gut time to adjust.”What’s Next for Probiotics?
Science is moving fast. In 2023, the NIH funded $12.5 million in new research to figure out which probiotic strains work best with which antibiotics. One surprising finding? Some probiotics might actually delay gut recovery after antibiotics. That’s why personalized approaches are the future-not one-size-fits-all. The FDA is working on new rules for live microbial products, but they won’t be finalized until at least 2026. Until then, you’re the gatekeeper of your own health. Choose wisely. Stick to proven strains. Talk to your doctor. And don’t assume more is better.Bottom Line
Taking probiotics with antibiotics can cut your risk of diarrhea by more than half-if you pick the right strain and take it correctly. Lactobacillus rhamnosus GG and Saccharomyces boulardii are your best bets. Take them 2-3 hours after your antibiotic, daily during and after treatment. Skip the unbranded, untested supplements. If you’re immunocompromised, skip probiotics altogether. And if you’re unsure? Ask your doctor. Your gut will thank you.Can probiotics prevent C. diff infection during antibiotics?
Yes, but only with specific strains. Saccharomyces boulardii and Lactobacillus rhamnosus GG have been shown to reduce the risk of C. diff-associated diarrhea by about 70% in high-risk patients. However, they don’t prevent C. diff infection itself-they reduce the chance of it turning into diarrhea. If you’re in the hospital or on strong antibiotics, ask your doctor if probiotics are right for you.
How long should I take probiotics after finishing antibiotics?
Continue for at least 1 to 2 weeks after your last antibiotic dose. Your gut microbiome takes time to rebuild. Stopping too early means you miss the window when probiotics can help restore balance. Some people choose to continue longer for general gut health, but 1-2 weeks is the minimum for preventing antibiotic-related side effects.
Can I take probiotics with food or should I take them on an empty stomach?
It depends on the strain and product. Acid-resistant strains like Saccharomyces boulardii can be taken anytime-even with food. Others, like Lactobacillus rhamnosus GG, are often more effective on an empty stomach, but studies show they still work with meals. Always follow the label instructions. If unsure, take them with a light snack to buffer stomach acid without interfering with absorption.
Do probiotics interfere with antibiotics?
No, they don’t interfere with antibiotics’ ability to kill harmful bacteria. But if you take them at the same time, the antibiotic will kill the probiotic before it can help. That’s why timing matters-take probiotics 2-3 hours after your antibiotic dose. This gives the antibiotic time to work and the probiotic time to survive.
Are there any side effects from taking probiotics with antibiotics?
Mild side effects like bloating, gas, or increased thirst are common in the first few days as your gut adjusts. These usually go away on their own. Rarely, people with weakened immune systems can develop serious infections from probiotics. If you feel worse after starting, stop and talk to your doctor. Don’t ignore new symptoms like fever, chills, or abdominal pain.
Can I get the same benefits from yogurt instead of supplements?
Yogurt and fermented foods contain beneficial bacteria, but they don’t reliably contain the specific strains or high enough doses needed to prevent antibiotic diarrhea. Most yogurts have L. acidophilus or Bifidobacterium, which help with general digestion but aren’t proven for AAD prevention. For targeted protection, use a supplement with L. rhamnosus GG or S. boulardii.
What if I forget to take my probiotic at the right time?
If you accidentally take your probiotic right after your antibiotic, don’t panic. Just wait until your next dose and space them properly then. Taking them too close together reduces their effectiveness, but it won’t harm you. Consistency over time matters more than perfect timing every single day.





12 Comments