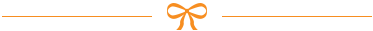
Why Talking About Medications with Your OB/GYN Isn’t Optional
Most women don’t realize that taking a daily vitamin or an over-the-counter painkiller could affect their pregnancy - or even their ability to get pregnant. The truth is, medications with OB/GYN discussions are one of the most important parts of reproductive care. Whether you’re trying to conceive, already pregnant, or breastfeeding, what you’re taking matters more than you think. Your OB/GYN doesn’t just check your blood pressure or listen to your baby’s heartbeat - they’re also your safety net for every pill, patch, and supplement in your medicine cabinet.
The American College of Obstetricians and Gynecologists (ACOG) says every woman should have a full medication review before even trying to get pregnant. And it’s not just about prescriptions. Herbal teas, fish oil capsules, CBD gummies, and even that nightly melatonin tablet can interfere with fertility, fetal development, or breast milk. In fact, 90% of pregnant women take at least one medication during pregnancy, and 68% continue taking drugs they were on before - like thyroid medicine, antidepressants, or blood pressure pills. But here’s the problem: most patients forget to mention the "natural" stuff. And that’s where things go wrong.
What You Need to Bring to Your Appointment
Walking into your OB/GYN appointment with a vague memory of your meds won’t cut it. You need a real list - detailed, accurate, and complete. Start at least 72 hours before your visit. Open your medicine cabinet. Take photos of every bottle. Write down:
- Prescription drugs: Exact name, dosage, how often you take it, and why. Example: "Levothyroxine 75 mcg, one tablet daily, for hypothyroidism."
- Over-the-counter meds: Even if you only take them "once in a while." Example: "Ibuprofen 200 mg, 1-2 tablets every 6 hours for headaches."
- Supplements: Brand name matters. Example: "Nature Made Prenatal, one tablet daily."
- Herbal products: St. John’s Wort, evening primrose oil, black cohosh - yes, even those. They’re not harmless just because they’re "natural."
- Recreational substances: Alcohol, nicotine, cannabis. Your provider needs to know. This isn’t judgment - it’s safety.
One patient on Reddit said she brought a spreadsheet with every supplement, including brand names and doses. Her OB printed it and kept it in her file. That’s the kind of preparation that makes a difference. If you can’t remember exact doses, snap a photo of the bottle. Your phone is your best tool here.
What Your OB/GYN Is Looking For
Your OB/GYN isn’t just checking off a box. They’re scanning for three big risks:
- Teratogens: Drugs that can cause birth defects. Examples: Accutane (isotretinoin), certain seizure meds like valproic acid, and high-dose vitamin A supplements.
- Drug interactions: Things like St. John’s Wort cutting the effectiveness of birth control by 50%. Or NSAIDs like ibuprofen raising the risk of low amniotic fluid after 20 weeks.
- Chronic condition management: If you have high blood pressure, diabetes, asthma, or depression, your meds may need adjustment during pregnancy. For example, Labetalol and Methyldopa are safe for high blood pressure - but ACE inhibitors like Lisinopril are not.
They’re also watching for what you’re not saying. A 2021 study found that 78% of primary care doctors skip screening for teratogenic meds - but OB/GYNs don’t. That’s why this conversation is different than your annual checkup with your family doctor. OB/GYNs are trained to spot reproductive risks others miss. They know that a medication perfectly safe for a 40-year-old with migraines might be dangerous for a 28-year-old trying to conceive.

Top 7 Questions to Ask Your OB/GYN
Don’t wait for them to ask. Come prepared with these questions. They’re not too much - they’re necessary.
- "Is this medication safe during pregnancy?" Don’t accept a vague "probably fine." Ask for the safety category (A, B, C, D, X). Category A is safest (rarely used). Category B is common and generally safe (like insulin or prenatal vitamins). Category D means there’s evidence of risk - but benefits may still outweigh risks. Category X means avoid completely.
- "Is there a safer alternative?" If you’re on a medication in Category C or higher, ask what else works. For example, Tylenol (acetaminophen) is preferred over ibuprofen during pregnancy. For anxiety, SSRIs like sertraline are often safer than benzodiazepines.
- "Should I stop this before I get pregnant?" Some meds need to be weaned off slowly. Others, like certain acne or migraine drugs, need to be stopped months before conception.
- "Will this affect my fertility?" Some antidepressants, antihypertensives, and even high-dose omega-3s can impact ovulation or sperm quality.
- "Is this safe while breastfeeding?" Many drugs pass into breast milk. Some are fine (like levothyroxine), others aren’t (like certain anti-anxiety meds).
- "Do I need more folic acid?" If you’re on seizure meds, metformin, or have a history of neural tube defects, you may need 4-5 mg daily - not the standard 0.4 mg.
- "Can you refer me to a pharmacist who specializes in pregnancy?" For complex cases (four or more meds, chronic illness), a maternal-fetal pharmacy specialist can help untangle interactions.
What Happens If You Don’t Prepare
Skipping prep isn’t just risky - it’s common. One patient forgot to mention evening primrose oil because she thought it was "just a supplement." She found out too late that it can trigger contractions. Another didn’t tell her OB she was taking melatonin nightly - and later learned it might interfere with progesterone levels. These aren’t rare stories.
Patients who prepare their medication lists reduce appointment time by 15-20 minutes and increase discussion quality by 40%. Those who don’t? They get rushed answers, vague reassurances, or worse - prescriptions that shouldn’t have been written. A 2022 survey found 74% of patients felt more confident when they came with questions. But 41% still felt anxious about forgetting something "not real medicine."
And it’s not just about mistakes. It’s about missed opportunities. If you’re on a safe antidepressant, your OB might help you stay on it - avoiding the bigger risk of untreated depression during pregnancy. If you’re on a risky blood pressure med, they can switch you before conception - preventing complications later. Preparation turns fear into control.
What’s Changing in 2026
The rules are evolving. In 2023, ACOG updated its guidelines to include medical marijuana and CBD products. That’s because 18% of reproductive-age women use cannabis - but only 38% of OB/GYNs routinely screen for it. That gap is closing.
Many clinics now use digital tools. The GW Medical Faculty Associates’ Babyscripts app lets hypertensive pregnant patients log their blood pressure and meds in real time. The FDA is working on standardized pregnancy risk scores for medications - expected in 2024. And by Q2 2024, ACOG will release a free patient app to help you build your medication list.
Even more advanced: some academic centers are testing genetic tests (like CYP2D6) to see how your body processes antidepressants. This isn’t sci-fi - it’s the future of personalized prenatal care.
Final Tip: Make This a Habit
You don’t need to be a medical expert. But you do need to be your own advocate. Keep your medication list updated on your phone. Add new pills as soon as you get them. Remove ones you stop. Bring it to every OB/GYN visit - even if you’re not pregnant. Because the next time you walk in, you might be.
Medication safety isn’t about being perfect. It’s about being honest. It’s about asking the hard questions. And it’s about showing up ready - not just hoping your provider will catch something you forgot to mention.
Can I keep taking my antidepressants during pregnancy?
Many antidepressants, especially SSRIs like sertraline and citalopram, are considered low-risk during pregnancy. Untreated depression can be more harmful than the medication. But it’s not one-size-fits-all. Your OB/GYN will weigh your mental health needs against potential risks - like preterm birth or neonatal adaptation syndrome. Never stop cold turkey. Work with your provider to adjust safely.
Is ibuprofen dangerous during pregnancy?
Yes - especially after 20 weeks. Ibuprofen and other NSAIDs can reduce amniotic fluid and affect fetal kidney development. Tylenol (acetaminophen) is the preferred pain reliever during pregnancy. If you need something stronger, talk to your OB/GYN before taking anything.
What if I took a medication before I knew I was pregnant?
Don’t panic. Most medications taken in the first 2-4 weeks after conception either have no effect or cause an all-or-nothing outcome - meaning the pregnancy either continues normally or ends in miscarriage. Tell your OB/GYN what you took, when, and how much. They’ll assess the risk and may recommend extra monitoring. But in most cases, the baby is fine.
Are herbal supplements safe during pregnancy?
No - not automatically. Many herbs can stimulate contractions, affect hormone levels, or interfere with blood clotting. Evening primrose oil, black cohosh, and dong quai are linked to early labor. Ginger is generally safe for nausea, but only in small doses. Always check with your OB/GYN before taking any herb, tea, or tincture.
Can I keep taking my blood pressure meds if I get pregnant?
Some are safe, others are not. ACE inhibitors (like lisinopril) and ARBs (like losartan) are dangerous during pregnancy and must be switched before conception. Safe options include methyldopa, labetalol, and nifedipine. If you’re on blood pressure meds, talk to your OB/GYN before trying to conceive - not after you’re pregnant.
Do I need more folic acid if I’m on birth control?
Birth control doesn’t increase your folic acid needs - but if you’re planning pregnancy, you should start taking 0.4-0.8 mg daily at least one month before trying. If you have a history of neural tube defects, diabetes, or take seizure meds, your OB/GYN may recommend 4-5 mg daily. Folic acid is one of the few supplements proven to prevent serious birth defects.
Can I breastfeed while taking my regular meds?
Many medications are safe during breastfeeding. Levothyroxine, most SSRIs, and insulin pass into breast milk in tiny amounts and are considered low-risk. But some drugs - like certain anti-anxiety meds, chemotherapy, or radioactive treatments - are not. Always ask your OB/GYN or a lactation consultant before taking anything new while nursing.
What to Do Next
Right now, open your medicine cabinet. Take photos of every bottle. Write down what you’re taking - even if you think it’s unimportant. Then, call your OB/GYN’s office and ask: "Can I schedule a medication review appointment?" You don’t need to be pregnant. You don’t need to be trying. You just need to be ready.
If you’re on multiple meds, ask for a referral to a maternal-fetal pharmacy specialist. If you’re not sure what’s safe, don’t guess. Ask. Your future self - and your future baby - will thank you.


15 Comments