Zoonotic Amoeba Infection Checker
This tool helps identify potential zoonotic amoeba infections in animals based on clinical signs and exposure history. It provides educational insights into the key species involved and their transmission pathways.
Potential Zoonotic Amoeba Infections Identified
Key Amoeba Species Overview
Entamoeba histolytica
Common in cattle and pigs; transmitted via fecal-oral route.
Colitis
Hepatic Abscesses
Naegleria fowleri
Found in warm water bodies; causes primary amoebic meningoencephalitis.
Encephalitis
Nasal Irrigation Exposure
Acanthamoeba spp.
Contact with contaminated soil/water; causes keratitis and encephalitis.
Keratitis
Granulomatous Encephalitis
Balamuthia mandrillaris
Soil-borne; rare but fatal granulomatous amoebic encephalitis.
Encephalitis
Skin Lesions
When wildlife, livestock, or pets become sick with amoeba infections, the ripple effects often reach humans, water supplies, and even local economies. Understanding why these tiny protozoa matter and how a One Health approach links human, animal, and environmental health to tackle shared threats can turn a baffling disease into a manageable challenge.
What are Amoeba single‑celled eukaryotic organisms that thrive in moist environments and can cause disease when they invade tissues?
Amoebae belong to the Phylum Amoebozoa or to diverse free‑living groups such as the family Vahlkampfiidae. Not all are harmful, but a handful can jump from water, soil, or contaminated feed into animal hosts. When an infected animal sheds cysts or trophozoites, those stages can survive in the environment, creating a feedback loop that puts people and other animals at risk - exactly the scenario One Health was built to address.
Key Zoonotic Amoebae Found in Animals
The following species are repeatedly linked to disease in mammals, birds, or reptiles and have documented human cases.
| Species | Typical Animal Hosts | Transmission Route | Animal Disease | Human Risk | Effective Treatment |
|---|---|---|---|---|---|
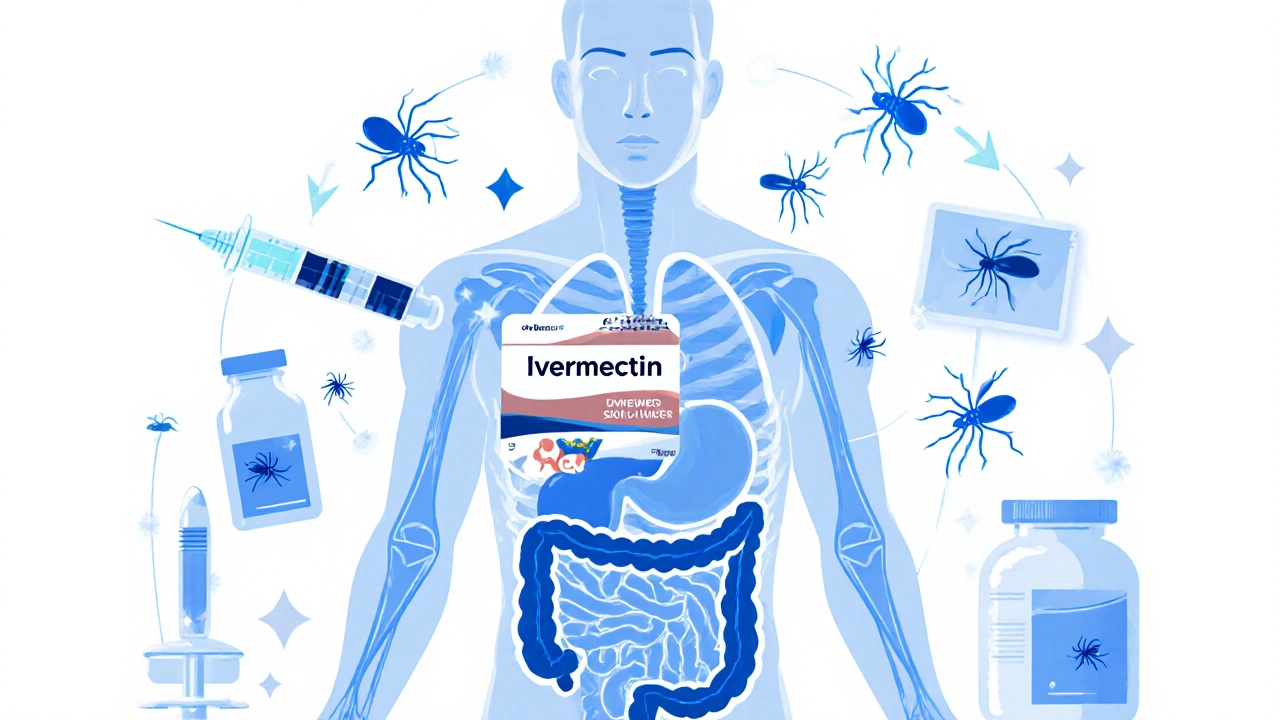
| Entamoeba histolytica | Cattle, pigs, primates | Fecal‑oral via contaminated water or feed | Colitis, hepatic abscesses | Severe dysentery, liver disease | Metronidazole + luminal agents |
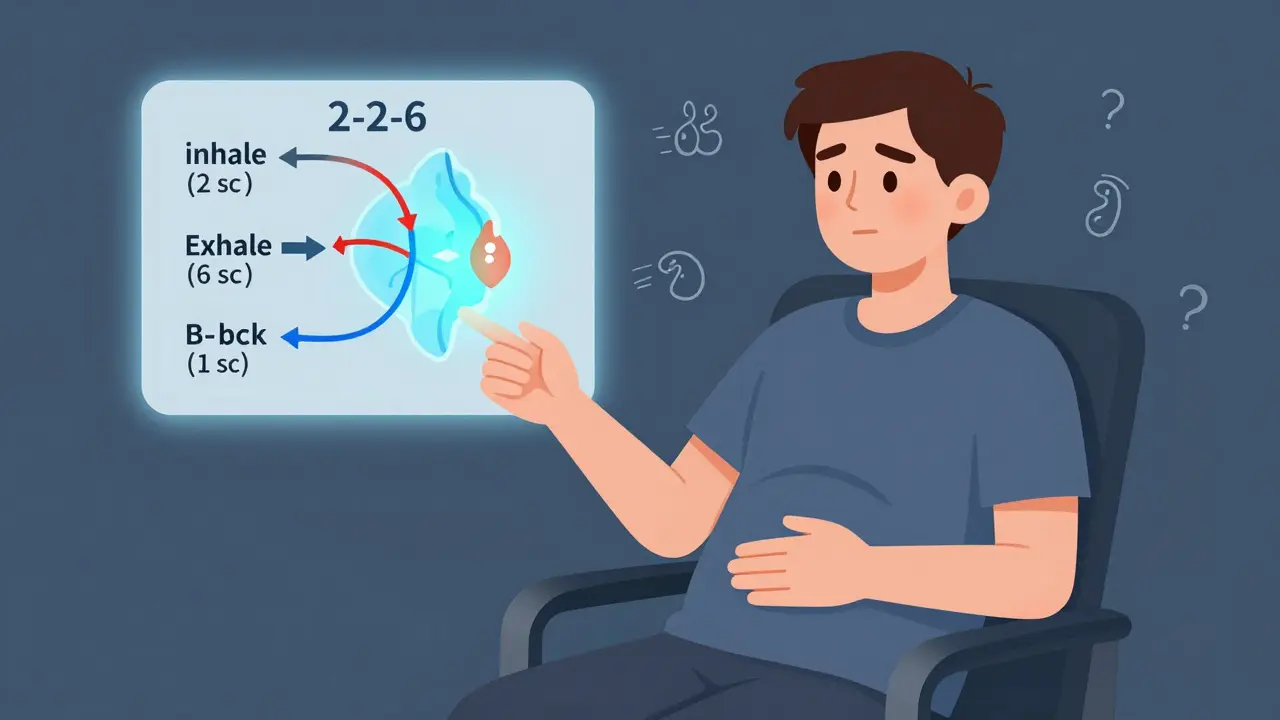
| Naegleria fowleri | Waterfowl, amphibians, laboratory rodents | Inhalation of contaminated warm water (nasal irrigation) | Rare encephalitis in animals, often fatal | Primary amoebic meningoencephalitis (PAM) | Amphotericin B + miltefosine |
| Acanthamoeba spp. | Dogs, cats, horses, exotic pets | Contact with contaminated soil or water; wound exposure | Granulomatous encephalitis, keratitis | Granulomatous amoebic encephalitis (GAE), keratitis | Miltefosine, azoles, pentamidine |
| Balamuthia mandrillaris | Rabbits, primates, wildlife | Soil inhalation or skin breach | Diffuse encephalitis, skin lesions | Rare but fatal GAE | Combination therapy (pentamidine, sulfadiazine, azoles) |
Applying the One Health Lens
Three pillars guide a One Health response to amoebiasis:
- Surveillance Integration: Veterinary labs, wildlife agencies, and public‑health labs share data on cyst detection, outbreak locations, and water‑quality testing.
- Environmental Management: Controlling standing water, improving irrigation drainage, and treating drinking water reduce the environmental load of cysts.
- Cross‑Sector Education: Farmers, pet owners, and clinicians receive coordinated training on recognizing signs, sampling techniques, and safe handling of specimens.
When these pillars click, a single case in a dairy cow can trigger a community‑wide water‑testing campaign before any human case emerges.
Diagnosis and Treatment in Animals
Accurate diagnosis hinges on three steps:
- Sample Collection: Fresh feces for Entamoeba, nasal lavage for Naegleria, corneal scrapings for Acanthamoeba. Use sterile containers and keep samples cool.
- Laboratory Confirmation: Microscopy (trophozoite morphology), antigen‑based ELISA, or PCR panels that target 18S rRNA genes. PCR offers the highest specificity, especially for mixed infections.
- Therapeutic Choice: Match the agent to the species. Metronidazole works for Entamoeba, while Naegleria and Acanthamoeba demand amphotericin‑based regimens plus newer agents like miltefosine.
Veterinarians should also consider supportive care-fluid therapy for diarrheal cases, anti‑inflammatory drugs for encephalitis, and wound debridement for skin lesions.

Prevention & Control Across Species
Practical steps that work for farms, zoos, and households:
- Provide filtered or UV‑treated water for livestock and pets.
- Implement regular cleaning of animal housing to eliminate standing moisture.
- Use protective equipment when handling soil or decaying vegetation.
- Educate staff on proper hand‑washing after animal contact.
- Monitor wildlife reservoirs (e.g., waterfowl) and limit their access to feed stores.
- In regions with warm climates, schedule seasonal water‑temperature checks to prevent Naegleria growth.
These measures not only curb animal disease but also protect the community’s water supply-a core One Health win.
Quick Checklist for Practitioners
- Identify high‑risk species on your premises (cattle, dogs, waterfowl).
- Collect appropriate specimens within 24hours of symptom onset.
- Run PCR or ELISA when microscopy is inconclusive.
- Start empiric therapy based on most likely amoeba while awaiting results.
- Report positive findings to local public‑health authorities.
- Review water and soil management practices monthly.
- Provide education sessions for staff and animal owners at least twice a year.
Frequently Asked Questions
Can my pet get a serious amoeba infection?
Yes. Dogs and cats can develop keratitis or encephalitis from Acanthamoeba, especially after exposure to contaminated tap water or soil.
What is the most reliable test for amoebic infections in livestock?
PCR targeting the 18S ribosomal RNA gene is the gold standard because it distinguishes pathogenic Entamoeba from harmless commensals.
How does a One Health approach change day‑to‑day farm management?
It adds routine environmental monitoring, encourages data sharing with health agencies, and prompts training on zoonotic risks-all without major extra costs.
Are there vaccines available for animal amoebiasis?
No licensed vaccines exist yet. Prevention focuses on hygiene, water treatment, and early detection.
What should I do if I suspect a water source is contaminated?
Stop using the water for animals and humans, conduct a cyst survey, and treat the source with chlorine or UV disinfection before reuse.






19 Comments