Joint Damage & Mental Health Risk Calculator
Assessment Questions
Answer the following questions to estimate your risk of mental health complications due to joint damage.
Your Risk Assessment
Complete the assessment to see your risk level
What This Means
This tool provides an estimate based on common factors associated with joint damage and mental health impacts. It's not a diagnosis, but a guide to understanding potential risks.
Understanding Your Risk
The risk level indicates how likely you are to develop mental health symptoms related to your joint condition:
- High Risk - You may be at increased risk for depression or anxiety. Consider seeking professional help.
- Medium Risk - You may experience some mental health challenges. Lifestyle changes and monitoring are recommended.
- Low Risk - You are less likely to experience severe mental health symptoms. Continue healthy practices.
Remember: Early detection and integrated care can significantly reduce the impact of both joint and mental health issues.
Quick Summary
- Joint damage triggers inflammation and chronic pain, which can change brain chemistry.
- People with osteoarthritis or rheumatoid arthritis are up to three times more likely to develop depression.
- Stress, sleep loss, and limited mobility create a feedback loop that worsens both joint and mental symptoms.
- Integrated treatment-combining physical therapy, medication, and mental‑health support-cuts risk of severe outcomes.
- Early screening for mood changes is as important as X‑rays for joint health.
When you hear the term Joint Damage is the deterioration of cartilage, bone, or surrounding tissues that impairs joint function and causes pain, you might picture a stiff knee or a sore wrist. What most people miss is how that physical breakdown ripples into the brain, influencing emotions, thoughts, and overall mental well‑being. This article unpacks the science, highlights the most common mental‑health conditions tied to damaged joints, and offers practical steps you can take today.
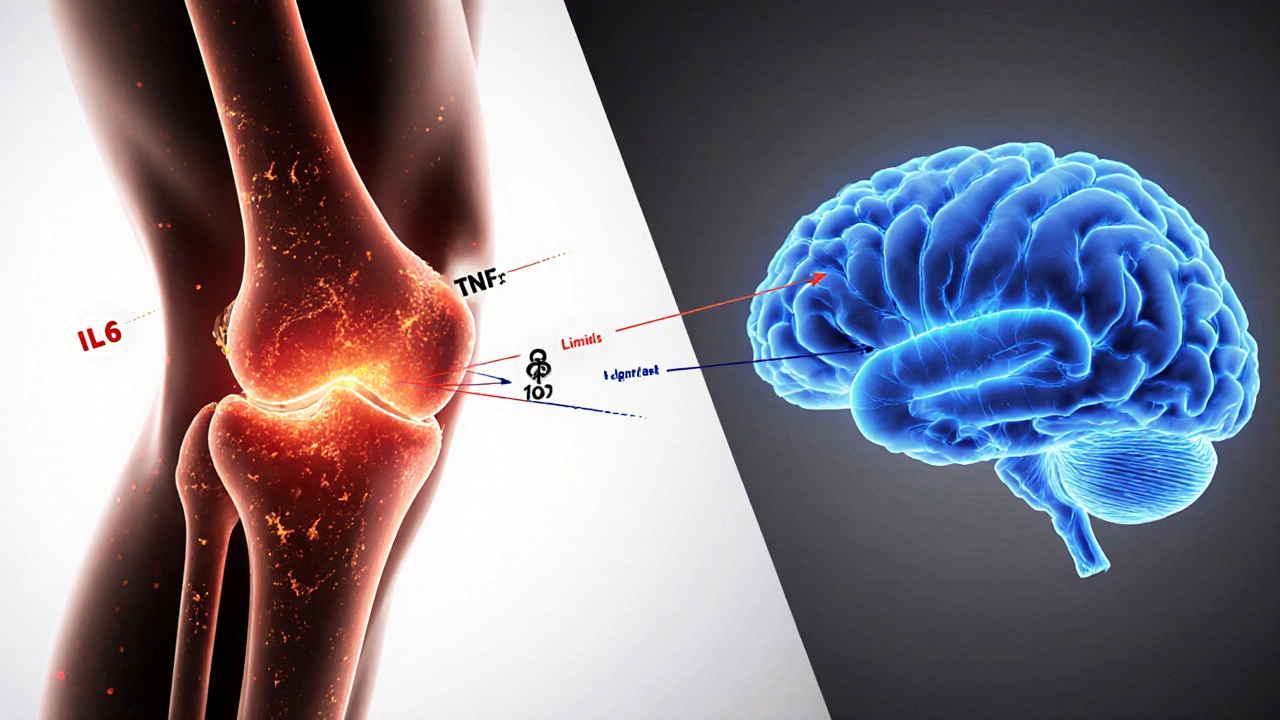
How Joint Damage Talks to the Brain
Three biological pathways carry the pain signal from a hurting joint to the mind:
- Inflammatory messengers-Inflammation releases cytokines such as IL‑6 and TNF‑α. These proteins can cross the blood‑brain barrier, altering neurotransmitter balance and triggering mood swings.
- Chronic pain circuits-Repeated nociceptive input rewires the spinal cord and brain’s pain matrix, making even mild aches feel overwhelming.
- Stress hormones-Persistent discomfort spikes cortisol, a hormone that, when elevated long‑term, disrupts sleep and reduces serotonin production.
Put together, these mechanisms create a perfect storm: the body signals distress, the brain interprets that signal as chronic threat, and emotional regulation falters.
Common Mental‑Health Conditions Linked to Joint Damage
Research from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) shows that adults with Osteoarthritis a degenerative joint disease characterized by cartilage loss have a 30‑45% higher prevalence of Depression a mood disorder marked by persistent sadness, loss of interest, and fatigue. Similar patterns appear for Rheumatoid arthritis an autoimmune condition that inflames joint linings, where anxiety rates can reach 40%.
Typical mental‑health issues include:
- Depression feelings of hopelessness, low energy, and reduced pleasure
- Anxiety excessive worry, restlessness, and muscle tension
- Sleep disturbances-pain interrupts REM cycles, leading to daytime fatigue and mood instability
- Social withdrawal-limited mobility reduces participation in hobbies and community events

Who Is Most at Risk?
Not everyone with joint damage spirals into mental‑health trouble. Several factors raise the odds:
- Severity and duration-People living with pain for more than six months are twice as likely to develop depression.
- Age-Older adults face compounded loss of independence, which magnifies emotional distress.
- Gender-Women report higher anxiety scores in rheumatoid arthritis, possibly due to hormonal influences.
- Social support-Isolation removes a crucial buffer against stress.
- Comorbid conditions-Diabetes, obesity, or cardiovascular disease increase inflammatory load, further stressing the brain.
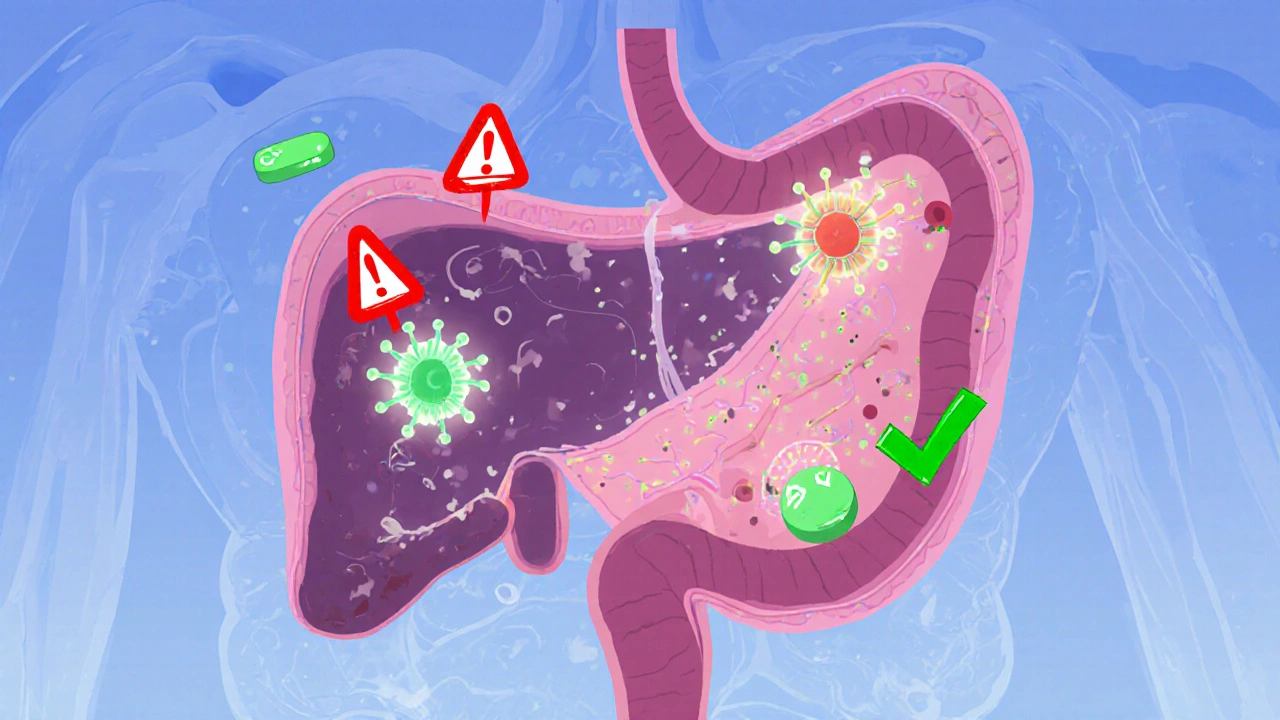
Managing the Dual Challenge: Integrated Care
Addressing joint pain without touching mental health is like fixing a leaky roof while ignoring the mold growing underneath. Effective programs combine:
- Medical treatment-Non‑steroidal anti‑inflammatory drugs (NSAIDs), disease‑modifying agents, or, for severe cases, joint replacement surgery.
- Physical Therapy targeted exercises and manual techniques that restore mobility and strengthen muscles-Regular, low‑impact workouts reduce cytokine levels by up to 20%.
- Psychological support-Cognitive‑behavioral therapy (CBT) teaches coping skills for pain catastrophizing; mindfulness‑based stress reduction lowers cortisol.
- Lifestyle tweaks-Omega‑3‑rich foods, vitamin D, and adequate sleep act as natural anti‑inflammatories.
Studies from the University of Sydney show that patients who receive both physiotherapy and CBT report 35% better pain scores and 28% fewer depressive symptoms than those who get only medical care.
Lifestyle Tips to Protect Joints and Mood
Small daily habits can break the pain‑anxiety loop:
- Move daily-A 30‑minute walk or swimming session keeps cartilage lubricated and releases endorphins.
- Strengthen core muscles-Exercises like squats and planks support knee and hip joints, reducing strain.
- Eat anti‑inflammatory foods-Berries, leafy greens, fatty fish, and nuts lower IL‑6 levels.
- Prioritize sleep-Aim for 7‑9 hours; a cool, dark room improves deep‑sleep phases that reset stress hormones.
- Practice mindfulness-Five minutes of guided breathing each morning cuts perceived pain intensity.

When to Seek Professional Help
Watch for these red flags:
- Persistent low mood lasting more than two weeks
- Thoughts of self‑harm or hopelessness
- Sudden increase in pain despite medication
- Loss of independence-unable to dress, bathe, or cook
- Severe sleep disruption (waking more than three times per night)
If you notice any of these, book an appointment with a primary‑care doctor, rheumatologist, or mental‑health professional. Early intervention shortens recovery time and prevents chronic disability.
Comparison of Joint Disorders and Their Mental‑Health Impact
| Condition | Typical Joint Damage | Common Mental‑Health Issue | Prevalence of Mood Disorder (% of patients) |
|---|---|---|---|
| Osteoarthritis | Cartilage thinning, bone spurs | Depression | 30-45 |
| Rheumatoid Arthritis | Synovial membrane inflammation, joint erosion | Anxiety & Depression | 35-50 |
| Gout | Uric‑acid crystal deposits | Depression | 20-30 |
| Lupus (musculoskeletal involvement) | Joint swelling, occasional erosions | Depression & PTSD‑like symptoms | 40-60 |
| Osteoporosis (fracture‑related) | Vertebral compression, hip fractures | Depression | 25-35 |
Next Steps and Troubleshooting
If you’ve tried exercise, diet, and medication but still feel stuck, consider these options:
- Referral to a pain specialist-They can assess for central sensitization and suggest neuromodulators.
- Group therapy-Sharing experiences with others facing similar joint issues reduces isolation.
- Tele‑health mental‑health coaching-Regular video check‑ins keep you accountable and allow rapid medication adjustments.
- Joint‑preserving surgeries-Arthroscopy or osteotomy may relieve mechanical pressure, indirectly improving mood.
Remember, healing is a two‑way street. As your joints get stronger, your mind often follows suit.
Frequently Asked Questions
Can joint pain really cause depression?
Yes. Chronic pain from damaged joints triggers inflammatory cytokines and stress hormones that lower serotonin and dopamine, key chemicals for mood regulation. Studies show a clear dose‑response: the longer the pain persists, the higher the risk of clinical depression.
Is anxiety more common than depression in arthritis?
Both are frequent, but anxiety often appears first because worrying about future disability can heighten pain perception. In rheumatoid arthritis, up to 40% experience significant anxiety, while depression rates hover around 30%.
Do anti‑inflammatory drugs improve mood?
Some NSAIDs reduce cytokine levels enough to modestly improve mood, but they don’t replace targeted mental‑health treatment. In many trials, adding CBT to medication yields the biggest gains.
How often should I be screened for depression if I have osteoarthritis?
A brief screening (like the PHQ‑2) every six months is recommended, or sooner if pain spikes or you notice changes in sleep or appetite.
Can exercise really help my mood when my joints hurt?
Low‑impact activities such as swimming, cycling, or tai chi boost endorphin release, improve circulation, and lower inflammatory markers-all of which translate into better mood within weeks.
Is there a link between joint damage and sleep disorders?
Pain often wakes you during the night, reducing deep‑sleep phases. In turn, sleep deprivation raises cortisol, making pain feel worse-a vicious cycle that can lead to chronic insomnia.




10 Comments