Many older adults take five or more medications every day. Some of these pills were prescribed years ago for conditions that have changed-or even disappeared. Yet they’re still on the list. This isn’t rare. It’s common. And it’s risky. Taking too many drugs can lead to dizziness, confusion, falls, kidney problems, and even hospital visits. The good news? You don’t have to keep taking them all. Deprescribing-the careful, step-by-step process of stopping or lowering doses of medicines that no longer help-can make your life safer and better. But it doesn’t happen by accident. It starts with a conversation. And you have to start it.
Why This Conversation Matters More Than You Think
Every year, about 15% of seniors on five or more medications experience a harmful side effect from one of them. That’s not a small number. It’s one in six. Many of these reactions come from drugs that were once helpful but now do more harm than good. Maybe your blood pressure is now too low. Maybe your stomach hurts every time you take that painkiller. Maybe you feel foggy after your afternoon pill. These aren’t just annoyances-they’re warning signs.
Doctors don’t always bring this up. They’re busy. They’re focused on what’s new. And they assume you’re fine because you’re not complaining. But here’s the truth: 68% of seniors would like to take fewer medications-if someone would just ask them if they’re ready. You don’t need to wait for your doctor to notice. You can lead the conversation.
What Deprescribing Really Means (And What It Doesn’t)
Deprescribing isn’t about quitting meds cold turkey. It’s not about skipping pills because you’re tired of them. It’s not about saving money-even though that can be a side benefit. Deprescribing is about matching your meds to your life right now.
Think of it like this: When you were younger, you took a statin to lower cholesterol because you had heart disease. Now you’re 80. Your cholesterol is fine. You walk slowly. You’re more worried about staying steady on your feet than about your LDL numbers. That statin? It might be making you dizzy. It might be hurting your muscles. It might not be helping anymore. Stopping it isn’t giving up. It’s choosing to protect what matters most: your balance, your independence, your mornings without falls.
Doctors use tools like the Beers Criteria and STOPP/START guidelines to spot medications that are risky for older adults. But you don’t need to know all the names. You just need to know how you feel.
How to Prepare Before Your Appointment
Walking into a doctor’s visit and saying, “I want to take fewer pills,” rarely works. It sounds vague. It sounds like you’re being difficult. But if you come prepared, you turn a yes-or-no question into a real discussion.
Here’s what to do in the week before your visit:
- Write down every medication you take. Include prescriptions, over-the-counter pills, vitamins, herbal supplements, and even eye drops. Don’t forget the aspirin you take for your heart or the melatonin you use at night. Many people forget these. But they matter.
- Write down how each one affects you. Not just side effects-how they change your daily life. For example: “I feel dizzy 2 hours after taking my blood pressure pill. I almost fell three times last month.” Or: “The sleeping pill makes me groggy all day. I can’t walk the dog like I used to.” Be specific. Time, frequency, and impact matter.
- Choose 1 or 2 meds you’re most concerned about. Don’t try to tackle everything at once. Pick the one causing the biggest problem. Maybe it’s the painkiller that makes you nauseous. Or the anticholinergic that makes your memory worse. Focus on that one.
- Write down one goal you care about. Not “I want fewer pills.” But “I want to be able to walk to the mailbox without holding onto the fence.” Or “I want to play cards with my grandkids without feeling sleepy.” This connects your meds to your life.
- Bring a printed copy of the Canadian Deprescribing Guidelines. You don’t need to read all of it. Just print the section on your medication class-like “benzodiazepines” or “antihypertensives.” It shows you’ve done your homework. Doctors respect that.
Studies show that patients who do this are 37% more likely to have a successful deprescribing plan. That’s not magic. It’s preparation.

How to Start the Conversation
Don’t say: “Can we cut some of these pills?”
Say: “I’ve been thinking about my medications and how they’re affecting my daily life. I’m worried one or two might be doing more harm than good. Can we talk about which ones might be safe to reduce?”
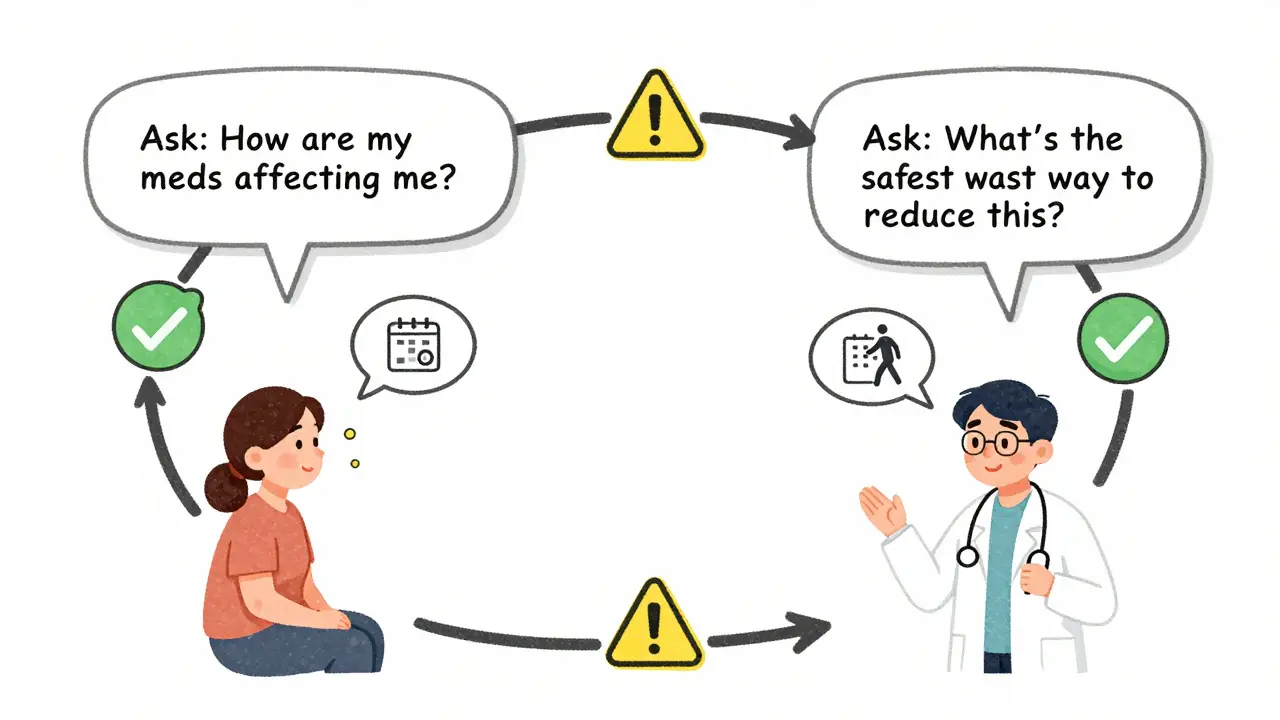
Use the “ask-tell-ask” method:
- Ask: “What’s your view on how my medications are working for me right now?”
- Tell: “I’ve noticed that after I take my sleeping pill, I’m really unsteady in the morning. I’ve almost fallen twice this month. I’d love to be able to walk to the garden without help.”
- Ask: “What would be the safest way to test if reducing this medicine could help?”
This approach works because it’s not demanding. It’s collaborative. It shows you’re not resisting care-you’re trying to get better care.
Doctors respond best when you connect the medication to a personal goal. Saying, “I want to be able to walk my granddaughter to school without feeling dizzy,” gets a much stronger response than “I want to take fewer pills.” Why? Because it’s not about the drugs. It’s about your life.
What to Expect When You Ask
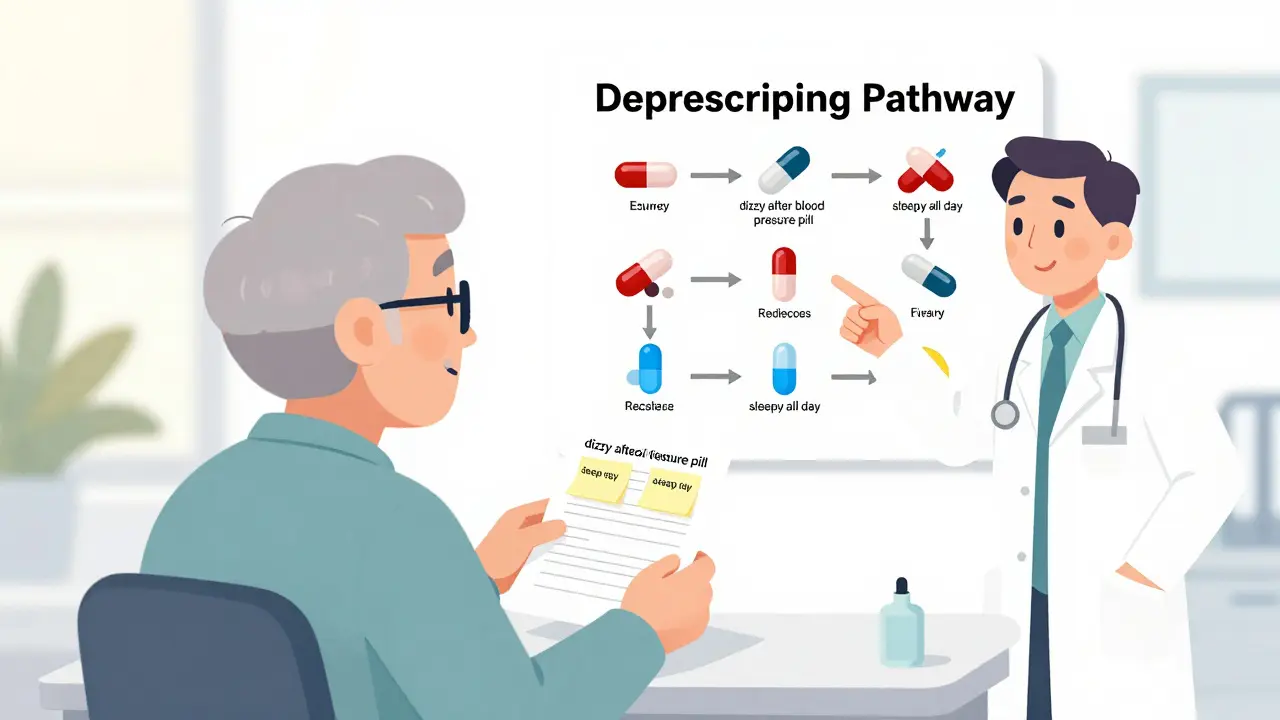
Most doctors will say yes-if you’ve prepared well. But they won’t stop everything at once. That’s dangerous. Deprescribing is slow. It’s usually done over weeks or months.
Here’s what a typical plan looks like:
- One medication is chosen to reduce first.
- The dose is lowered by 25% every 2-4 weeks.
- You keep a simple journal: “Did I feel dizzy? Did I sleep better? Did my pain change?”
- You schedule a follow-up in 4-6 weeks to check how you’re doing.
Some medications need to be tapered slowly. Others can be stopped more quickly. Your doctor will know which. But you need to agree on the plan-and stick to it. Don’t stop on your own. Don’t skip doses. This isn’t a DIY project. It’s a team effort.
And if your doctor says no? Ask why. “What’s the biggest risk if I stop this?” “What would happen if I tried reducing it slowly?” Sometimes, they’ll say, “We can try it.” Other times, they’ll explain why it’s still needed. Either way, you’ve had a real conversation.
What If You’re Afraid?
It’s normal to be scared. What if your blood pressure spikes? What if your pain comes back? What if your doctor thinks you’re being difficult?
Here’s the truth: 89% of doctors say deprescribing goes better when the patient brings it up. They’re not annoyed. They’re relieved. Many of them want to help but don’t know how to start.
And the fear of worsening symptoms? That’s why you do it slowly-with monitoring. You’re not jumping off a cliff. You’re stepping down one rung at a time.
And if you’re worried about being seen as “difficult”? Remember: You’re not asking for a favor. You’re asking for safe, thoughtful care. That’s your right.
What Happens After You Start?
Once you begin reducing a medication, pay attention. Keep your journal. Note changes in energy, sleep, balance, mood, or pain. Bring it to your next visit.
If you feel worse, don’t panic. Call your doctor. It might mean you need to slow down. Or it might mean you need a different approach. Either way, you’re in control.
And if you feel better? That’s the goal. Less clutter. More clarity. More freedom. More time to do the things you love-without the side effects holding you back.
It’s Not Just About Pills. It’s About Living.
Medications are tools. Not life sentences. You didn’t take them to become a list of drugs. You took them to live well. If they’re no longer helping you do that, it’s okay to let them go.
Deprescribing isn’t giving up. It’s choosing. Choosing safety over convenience. Choosing function over fear. Choosing your life over your pill bottle.
You don’t need to wait for your doctor to bring it up. You don’t need to be perfect. You just need to be ready. And you are.
What is deprescribing?
Deprescribing is the process of safely reducing or stopping medications that are no longer beneficial-or that may be causing more harm than good. It’s especially important for older adults taking multiple drugs. The goal isn’t to take fewer pills for the sake of it, but to match your medications to your current health goals and quality of life.
Why don’t doctors usually bring up deprescribing?
Most doctors are focused on treating new or active conditions. They may not realize how many medications you’re on, or they assume you’re fine because you’re not complaining. Also, many doctors feel undertrained in how to have these conversations. That’s why it’s important for you to start the discussion.
Can I just stop a medication on my own?
No. Stopping some medications suddenly can be dangerous. Blood pressure drugs, antidepressants, and anti-seizure meds, for example, can cause serious withdrawal symptoms if stopped abruptly. Always work with your doctor to create a safe, gradual plan.
What if my doctor says no to deprescribing?
Ask why. “What’s the biggest risk if I stop this?” “Is there a way we could try reducing it slowly?” Sometimes, the answer is valid-you still need the medication. But other times, they’ll agree to a trial. If they refuse without explanation, consider asking for a referral to a geriatrician or pharmacist who specializes in medication reviews.
How long does deprescribing take?
It varies. Most successful deprescribing plans take weeks to months. One medication is usually reduced at a time, with doses lowered by 25% every 2-4 weeks. You’ll need follow-up visits to check how you’re feeling. Patience is key-rushing can lead to setbacks.
Are there any tools or resources I can bring to my doctor?
Yes. The Canadian Deprescribing Network has free, evidence-based guidelines for common medications like benzodiazepines, anticholinergics, and proton pump inhibitors. Print the section on your specific drug. Also, bring a complete list of all your medications-including supplements and over-the-counter pills. This helps your doctor see the full picture.
Will reducing medications make me sicker?
It’s possible-but only if done too quickly or without monitoring. That’s why deprescribing is done slowly and with follow-up. Many people feel better after stopping a medication that was causing side effects like dizziness, confusion, or fatigue. The goal is to remove drugs that are no longer helping, not ones that are still protecting you.







10 Comments