Opioid Itch Treatment Calculator
Determine Best Treatment for Opioid-Induced Itching
Select patient factors to receive evidence-based treatment recommendations. Based on the article's clinical algorithm and efficacy data.
Recommended Treatment
Select options to see recommendations.
When patients get a dose of morphine, fentanyl or another strong painkiller, they sometimes end up with an unbearable urge to scratch. That sensation-known as opioid induced itching-can turn a routine postoperative recovery into a night of sleepless discomfort.
What Is Opioid‑Induced Itching?
Opioid‑Induced Itching is an unpleasant skin sensation that provokes an urge to scratch and occurs as a direct side effect of opioid administration. It is also called opioid‑induced pruritus. Reports show that anywhere from 30% to nearly every patient receiving spinal or epidural opioids experience it, with intrathecal morphine at the top of the list.
Why Do Opioids Trigger Itch?
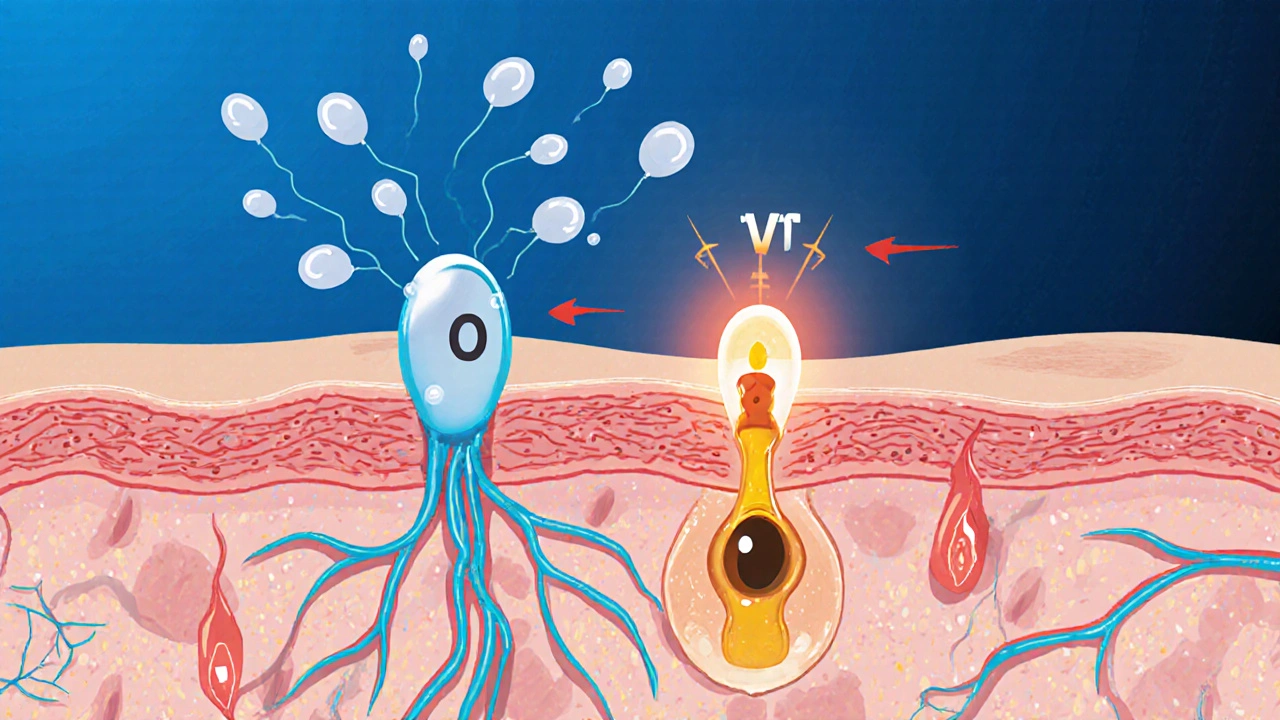
The old textbook answer blamed histamine released from Mast Cells immune cells in the skin that store and release histamine upon activation. Early studies demonstrated that morphine, codeine and meperidine can cause non‑immunologic histamine discharge at concentrations as low as 10⁻⁹ M.
Modern research, however, paints a more nuanced picture. A 2018 Nature Scientific Reports study showed that activation of the Mu Opioid Receptor a receptor that mediates analgesia and, paradoxically, itch when stimulated on peripheral nerve endings drives itch through TRPV1 a heat‑sensing ion channel expressed on dorsal root ganglion neurons fibers. When a selective MOR agonist like DAMGO was injected into the skin, patients felt intense itch that was blocked by a peripherally restricted antagonist (naloxone‑methiodide) and disappeared when TRPV1 was co‑stimulated with capsaicin.
In practice, both pathways can co‑exist. Histamine contributes more to urticarial reactions (hives), while the neural route dominates the classic “pins‑and‑needles” itch seen after a single bolus of intrathecal morphine.
Incidence by Administration Route
- Intrathecal morphine: 70‑100% experience pruritus.
- Intravenous opioids: 30‑50%.
- Oral opioids: 10‑30%.
The higher incidence with neuraxial delivery reflects direct exposure of spinal MORs where itching pathways are densely packed.
Management Options: From Antihistamines to Receptor‑Targeted Drugs
Because a single approach rarely solves every case, clinicians usually adopt a stepwise or multimodal strategy.
| Intervention | Mechanism | Typical Dose | Pruritus Reduction | Impact on Analgesia |
|---|---|---|---|---|
| First‑generation antihistamine (e.g., diphenhydramine) | Histamine H1 blockade | 25‑50 mg IV | 20‑30% | None, but causes sedation |
| Second‑generation antihistamine (e.g., cetirizine) | Selective H1 blockade | 10 mg PO | 30‑40% (still under study) | Minimal sedation |
| Naloxone a mu opioid receptor antagonist infusion | MOR antagonism (peripheral) | 0.25 µg/kg/min | 60‑80% | Analgesia preserved if titrated |
| Nalbuphine mixed mu antagonist / kappa agonist | Mu block + kappa activation | 5‑10 mg IV | ≈85% | Analgesia maintained or slightly enhanced |
| Butorphanol kappa agonist with partial mu antagonism | Kappa activation, mu blockade | 0.01‑0.02 mg/kg IV | 70‑80% (score drop 8.2→2.1) | Analgesia retained |
| IV Lignocaine | Na⁺ channel blockade (non‑opioid) | 1.5 mg/kg | ≈70% | No effect on opioid analgesia, requires cardiac monitoring |
Notice how agents that directly target the MOR or add kappa stimulation achieve the biggest itch drop while sparing pain relief. That’s why many modern protocols favor nalbuphine or a low‑dose naloxone drip over old‑school diphenhydramine.
Putting It All Together: A Practical Algorithm
- Assess onset (usually 5‑30 min after opioid dose) and distribution (face, upper torso, neck).
- Rule out true allergic reaction (look for wheal, hypotension, bronchospasm). If anaphylaxis is suspected, treat per ACLS guidelines-not with antihistamines alone.
- If itching is mild and patient is stable, try a second‑generation antihistamine (cetirizine 10 mg PO).
- For moderate‑to‑severe itch, start a low‑dose naloxone infusion (0.1‑0.25 µg/kg/min) while monitoring pain scores.
- If naloxone blunts analgesia, switch to a mixed mu antagonist/kappa agonist such as nalbuphine 5 mg IV; titrate every 5 min until itch subsides.
- Consider non‑opioid adjuncts (IV lignocaine) if receptor drugs are contraindicated.
- Document timing, dose, and response; use the hospital’s “Pruritus First‑Response” checklist to ensure consistency.
When applied correctly, most patients experience relief within 5‑10 minutes and can continue their pain regimen uninterrupted.
Special Populations: Obstetrics & Chronic Pain
Cesarean‑section patients receiving intrathecal morphine often rank itch as the most disruptive postoperative symptom. Studies show 78% describe it as “severely disruptive” to mother‑infant bonding. In this group, a 2 mg IV bolus of nalbuphine works in under 5 minutes without the drowsiness that diphenhydramine brings.
For chronic pain sufferers on long‑term oral opioids, the itch can become a reason to taper or stop therapy altogether (≈22% discontinue because of pruritus). Here, rotating to a kappa‑biased agonist like difelikefalin (CR845) in a clinical trial reduced itch by 65% while preserving analgesia.

Future Directions
By 2028, experts predict that mu‑antagonist/kappa‑agonist combos will be standard in 75% of major centers. Ongoing Phase II trials of peripherally restricted kappa agents (difelikefalin) aim to eliminate central side‑effects entirely. At the same time, new data from a 2023 Journal of Investigative Dermatology paper revive the histamine angle, showing serum tryptase correlates with itch severity in 68% of morphine patients. This suggests a future where an initial tryptase screen could help decide whether an antihistamine‑first approach is warranted.
Key Take‑aways for Clinicians
- Recognize that opioid‑induced itching is mainly a MOR‑driven neural event, not just histamine release.
- Prioritize receptor‑targeted drugs (naloxone, nalbuphine, butorphanol) for moderate‑to‑severe cases.
- Reserve antihistamines for mild itch or patients with known allergy‑related histamine surges.
- Administer antipruritic agents within 5‑10 minutes of symptom onset for maximum effect.
- Document and follow a standardized algorithm to avoid misdiagnosing itch as anaphylaxis.
Frequently Asked Questions
Why does morphine cause itching but not other analgesics?
Morphine is a potent Mu Opioid Receptor agonist that, aside from blocking pain signals, also activates itch‑specific pathways in peripheral neurons. Not all opioids have the same MOR bias; some, like buprenorphine, produce far less pruritus.
Can antihistamines ever fully stop opioid‑induced itching?
Only in a minority of cases. First‑generation antihistamines work for about 20‑30% of patients, mainly when histamine release contributes to a urticarial rash. For the classic neural itch, receptor antagonists are far more reliable.
Is giving naloxone risky for pain control?
If dosed low (0.1‑0.25 µg/kg/min) and titrated, naloxone can suppress itch while preserving >90% of analgesia. Overshooting the dose can reverse pain relief, so continuous pain scores are essential.
What’s the role of kappa agonists like nalbuphine?
Kappa activation provides its own analgesic effect while the mu‑blocking component eliminates itch. This dual action leads to the highest reported success rates (≈85%) without sacrificing pain control.
Should I screen for mast cell activation before treating itch?
Routine screening isn’t standard yet. However, if a patient reports hives, flushing, or elevated serum tryptase, an antihistamine‑first approach may be justified.






12 Comments