When your bones start to weaken without warning, even a simple fall or a sneeze can lead to a fracture. That’s the reality for more than 10 million Americans with osteoporosis, and another 44 million with early bone thinning. It’s not just an older person’s problem - it’s a silent disease that creeps in over years, often unnoticed until something breaks. The good news? We have tools to stop it. One of the most proven, widely used, and cost-effective treatments is bisphosphonate therapy.
What Exactly Is Osteoporosis?
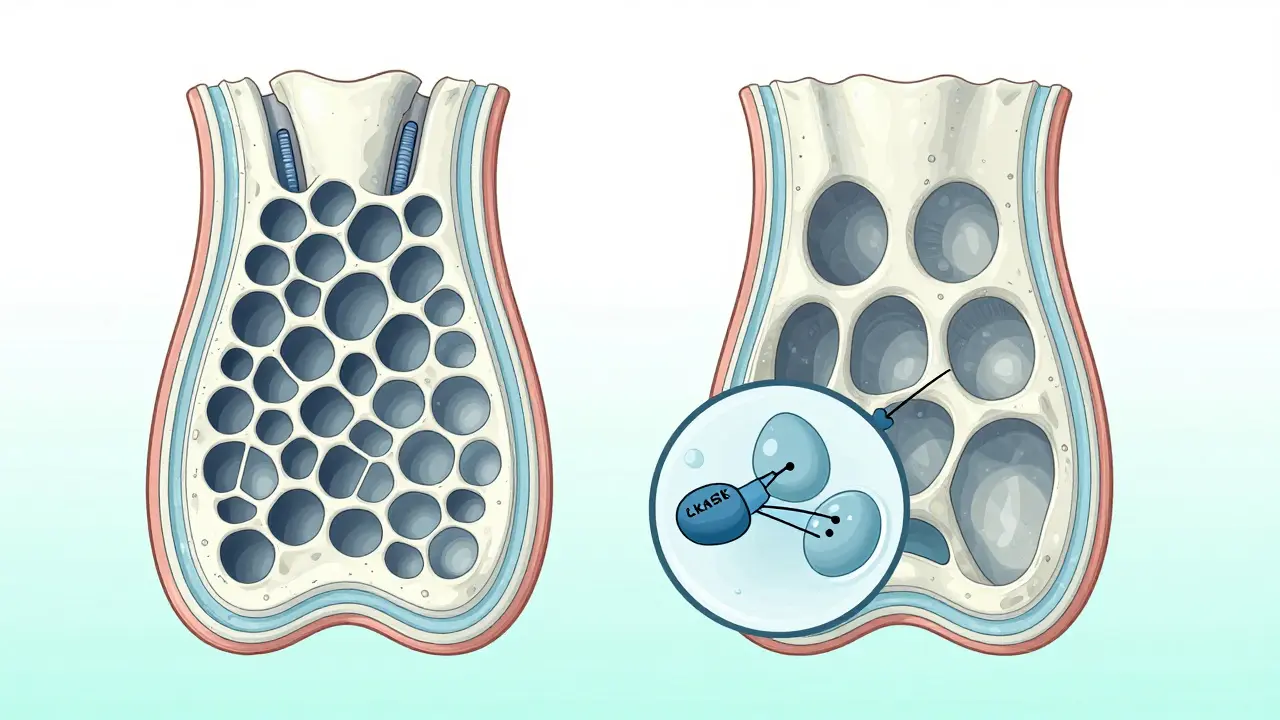
Osteoporosis isn’t just about getting older. It’s when your bones lose density and structure, becoming porous and fragile. Think of it like a sponge that’s lost its firmness - the inside becomes full of holes, and the outer shell gets thin. This happens because your body breaks down old bone faster than it builds new bone. The result? Bones that snap under pressure that shouldn’t harm them - a wrist from a fall, a hip from stepping wrong, or a vertebra from bending over.
The World Health Organization defined osteoporosis in 1994 based on bone mineral density (BMD) measurements. A T-score of -2.5 or lower on a DXA scan means you have osteoporosis. A score between -1 and -2.5 is called osteopenia - a warning sign. Women are at higher risk, especially after menopause, because estrogen helps protect bone. When estrogen drops, bone loss speeds up. Men get it too, but less often and later in life.
Why Bisphosphonates Are the First-Line Treatment
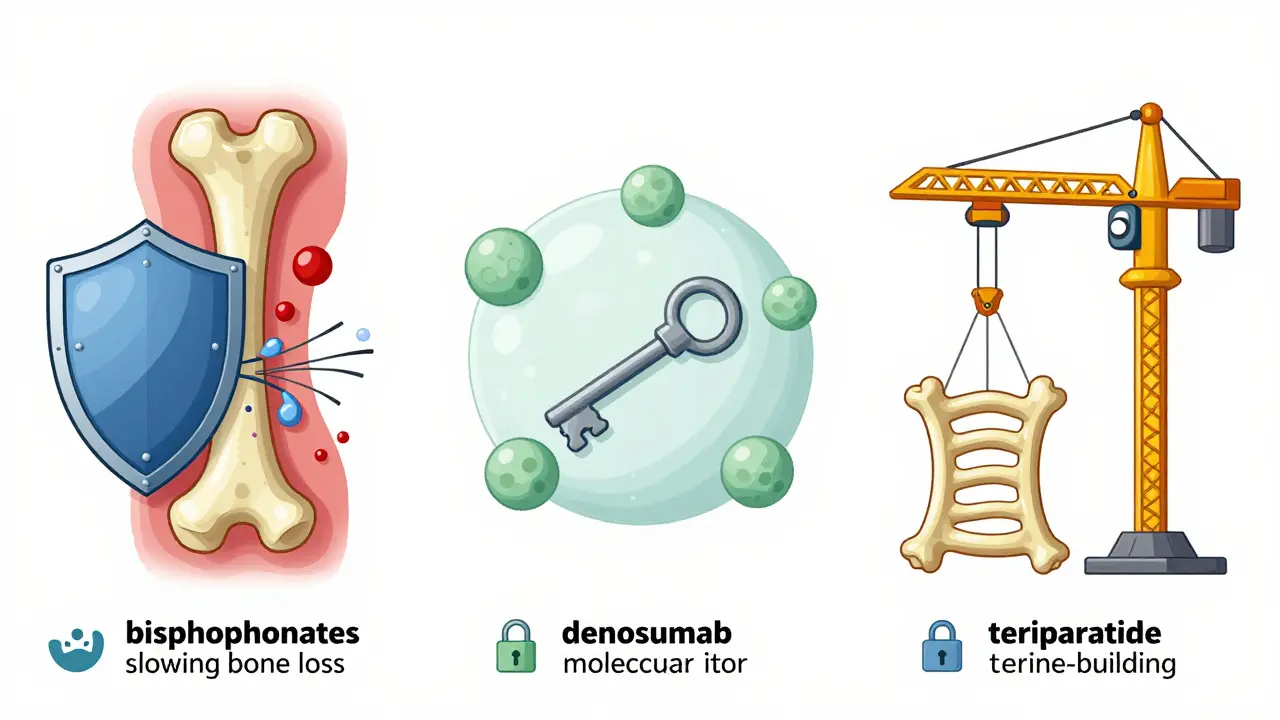
Bisphosphonates don’t rebuild bone - they stop it from falling apart. These drugs stick to bone surfaces and block the cells that break bone down: osteoclasts. By slowing bone loss, they give your body a chance to rebuild what’s been lost. That’s why they’re the go-to for most people starting treatment.
There are two types: non-nitrogen and nitrogen-containing. The nitrogen ones - like alendronate (Fosamax), risedronate (Actonel), ibandronate (Boniva), and zoledronic acid (Reclast) - are stronger and more effective. They work by disrupting a key enzyme in osteoclasts, which eventually causes those cells to die. Less bone breakdown means higher bone density over time.
Studies show alendronate cuts vertebral fracture risk by 48% and hip fracture risk by 51% over three years. Zoledronic acid, given as a yearly IV infusion, reduces fractures by about 40%. These aren’t small numbers. For someone who’s already had a fracture, this can mean the difference between living independently and needing long-term care.
How You Take Bisphosphonates Matters
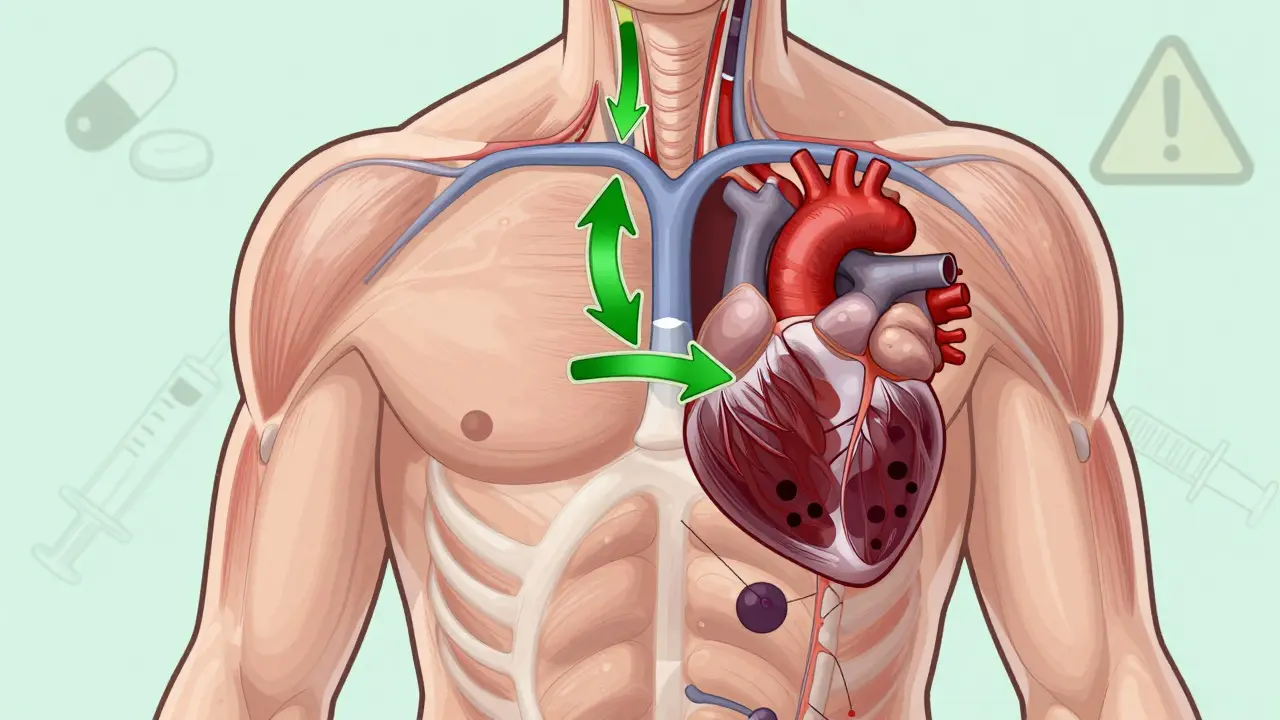
These medications are powerful, but only if you take them right. Oral bisphosphonates - the most common form - have strict rules:
- Take them first thing in the morning, on an empty stomach.
- Swallow with a full glass of plain water (8 ounces).
- Stay upright for at least 30 to 60 minutes - no lying down, no bending over.
- Avoid food, coffee, juice, or other meds for at least 30 minutes after taking it.
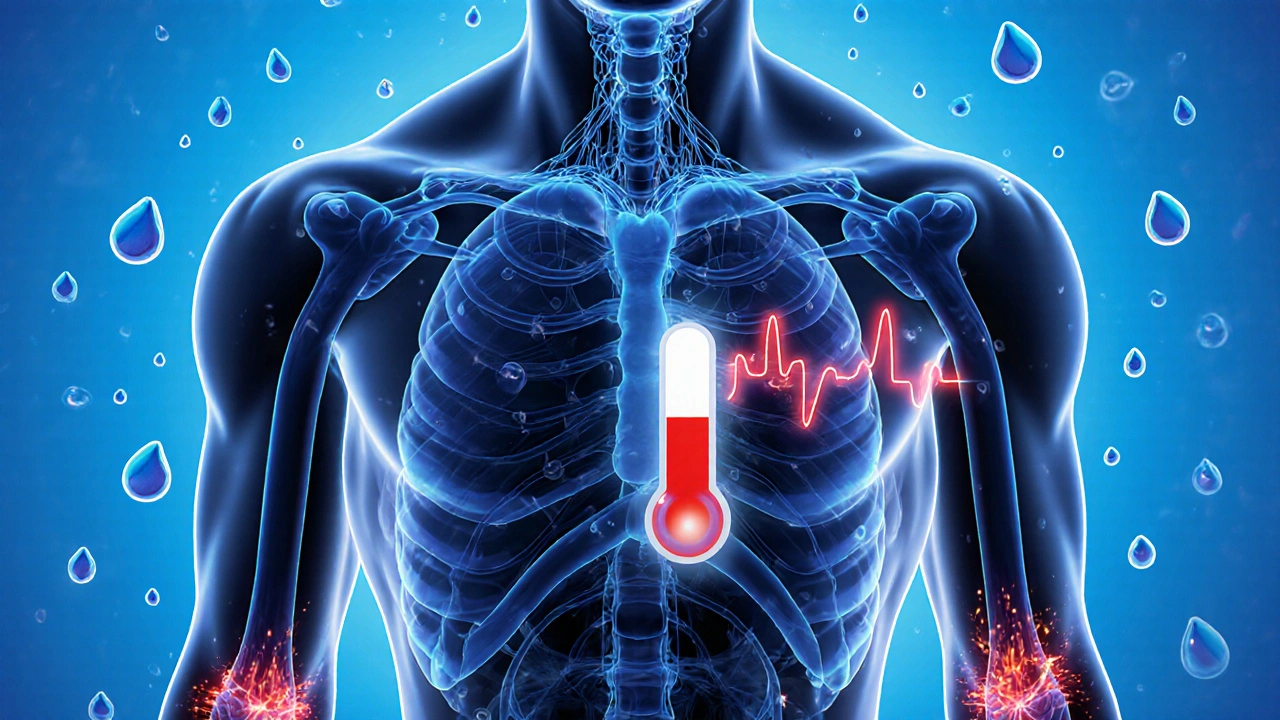
Why? Because if you don’t follow these steps, the drug can irritate your esophagus. About 10-15% of people on oral bisphosphonates get heartburn, nausea, or even esophageal pain. That’s why some switch to the yearly IV version - zoledronic acid. No stomach issues, no dosing rules. Just one 15-minute infusion once a year.
But adherence is a problem. Only about half to 70% of people stick with oral bisphosphonates after a year. The rules are hard. The side effects are real. And if you miss doses, the protection fades.
What Are the Risks?
No drug is perfect. Bisphosphonates have rare but serious side effects.
Atypical femoral fractures - these are breaks in the thigh bone that happen with little or no trauma. They’re unusual, occurring in about 3 to 5 cases per 10,000 patient-years. But they’re real. They often start as a dull ache in the thigh and get worse over weeks.
Osteonecrosis of the jaw - this is when part of the jawbone dies, usually after dental surgery or trauma. It’s even rarer - 0.01% to 0.04% of patients. Risk goes up if you’re on long-term therapy, have poor dental health, or get invasive dental work while on the drug.
That’s why dentists and doctors now talk about a drug holiday. If you’ve been on bisphosphonates for 3 to 5 years and your fracture risk is low, you might stop taking them for a while. Your bones still hold onto the drug for years, so protection doesn’t vanish overnight. Studies show many people stay protected for 1-2 years after stopping. But if your risk is high - you’ve had a fracture, or your BMD keeps dropping - you keep going.
How Do Bisphosphonates Compare to Other Treatments?
Bisphosphonates aren’t the only option, but they’re still the most common - about 65% of prescriptions in the U.S. are for them.
Denosumab (Prolia) is a shot every six months. It works differently - it targets a protein that activates osteoclasts. It’s more effective at increasing bone density than some bisphosphonates. But here’s the catch: if you stop, your bone density plummets, and you can have a spike in spinal fractures. You can’t just quit. You have to switch to another drug.
Teriparatide (Forteo) is different. It doesn’t slow bone loss - it makes new bone. It’s an injectable daily hormone that stimulates bone growth. It can increase BMD by 9-13% in 18 months. But it’s expensive - around $1,800 a month - and you can only use it for two years. It’s usually for people with severe osteoporosis who haven’t responded to other treatments.
Romosozumab (Evenity) is newer. It builds bone and blocks breakdown at the same time. It cuts vertebral fractures by 73% in the first year. But it comes with a black box warning: increased risk of heart attack and stroke. So it’s not for people with heart disease.
Bisphosphonates still win on cost, safety data, and ease of use. Generic alendronate costs $20-$40 a month. Teriparatide is 90 times more expensive. For most people, especially those just starting treatment, bisphosphonates make the most sense.
Who Should Be Tested and When?
Not everyone needs a bone scan. But if you’re a woman over 65, or a man over 70, get tested. Sooner if you’ve had a fracture after 50, if you’re on long-term steroids, if you’ve lost more than 1.5 inches in height, or if you have a family history of hip fractures.
The Fracture Risk Assessment Tool (FRAX) helps doctors estimate your 10-year risk. If your chance of a major fracture is over 20%, or your hip fracture risk is over 3%, treatment is recommended. DXA scans are done before starting bisphosphonates and repeated every 1-2 years to track progress.
Renal function matters too. If your kidneys aren’t working well - creatinine clearance below 30-35 mL/min - some bisphosphonates aren’t safe. Zoledronic acid requires at least 35 mL/min. Your doctor will check this before prescribing.
What Do Patients Really Say?
On review sites, alendronate has a 5.4 out of 10 rating. Some say: “It stopped my bone loss after my wrist broke.” Others: “I couldn’t handle the stomach pain - switched to the IV shot and it’s been fine.”
One common worry: “How do I know when to stop?” That’s where your doctor comes in. If your BMD is stable, you haven’t had new fractures, and your risk is low, a drug holiday might be right. If your BMD drops again, or you break a bone, it’s time to restart.
Adherence is the biggest hurdle. Taking a pill right after waking up, staying upright for an hour, avoiding coffee - it’s a lot. That’s why many switch to the yearly infusion. It’s easier. And it works just as well.
What’s Next for Osteoporosis Treatment?
The field is moving toward personalization. Not everyone needs the same drug for the same length of time. The 2023 DATA-HD study showed that after 10 years of combined teriparatide and alendronate, bone density stayed high - challenging the idea that you can’t use these drugs long-term.
Researchers are now looking for better biomarkers to tell when a drug holiday is safe. Blood tests that show bone turnover rates could one day replace the need for frequent scans.
But for now, bisphosphonates remain the backbone of osteoporosis care. They’re affordable, well-studied, and proven. For most people, they’re the best first step.
Key Takeaways
- Osteoporosis is a silent disease that weakens bones and increases fracture risk - especially after menopause.
- Bisphosphonates like alendronate and zoledronic acid are first-line treatments because they slow bone loss and reduce fractures by up to 50%.
- Oral bisphosphonates require strict dosing rules to avoid esophageal irritation; IV versions avoid this issue.
- Rare side effects include atypical femur fractures and osteonecrosis of the jaw - but these are uncommon.
- A drug holiday after 3-5 years may be safe for low-risk patients to reduce long-term risks.
- Bisphosphonates are cheaper and have more long-term safety data than newer drugs like denosumab or teriparatide.
- DXA scans and FRAX scores guide treatment decisions - don’t skip them.
Can bisphosphonates rebuild bone or just stop it from breaking down?
Bisphosphonates don’t rebuild bone - they stop it from breaking down too fast. This lets your body’s natural bone-building process catch up. Over time, bone density improves because less is lost. But they don’t create new bone like anabolic drugs such as teriparatide or romosozumab do.
Is it safe to take bisphosphonates for more than 5 years?
For high-risk patients - those who’ve had fractures or have very low bone density - yes, longer use is often necessary. But for low-risk patients, guidelines recommend a drug holiday after 3 to 5 years. This reduces the risk of rare side effects like atypical fractures. Your doctor will monitor your bone density and fracture risk to decide when to pause or restart.
Why do I have to stay upright after taking oral bisphosphonates?
Oral bisphosphonates can irritate your esophagus if they sit there too long. Staying upright helps the pill move quickly into your stomach. Lying down, bending over, or eating too soon increases the chance of heartburn, pain, or even esophageal damage. It’s a small step that prevents a big problem.
What happens if I stop taking bisphosphonates suddenly?
Unlike denosumab, bisphosphonates don’t cause a sudden rebound in bone loss. The drug stays in your bones for years after you stop, so protection lasts. Bone density may slowly decline over time, but not rapidly. That’s why a drug holiday is possible. Still, if your fracture risk increases again, you may need to restart.
Are there natural ways to improve bone density without medication?
Yes - but they won’t replace medication if you have osteoporosis. Weight-bearing exercise (walking, dancing, lifting weights), enough calcium (1,200 mg daily), vitamin D (800-1,000 IU daily), and avoiding smoking and excess alcohol help. But if your bone density is already low, these alone won’t reduce fracture risk enough. Medication is needed for that.




15 Comments