Chemotherapy isn’t magic. It’s not a cure-all. But for millions of people facing cancer, it’s one of the most powerful tools doctors have. It works by attacking cells that divide fast - the kind of cells that make up tumors. The problem? So do your hair follicles, your gut lining, and your bone marrow. That’s why chemotherapy brings side effects that feel just as harsh as the disease itself.
How Chemotherapy Actually Kills Cancer Cells
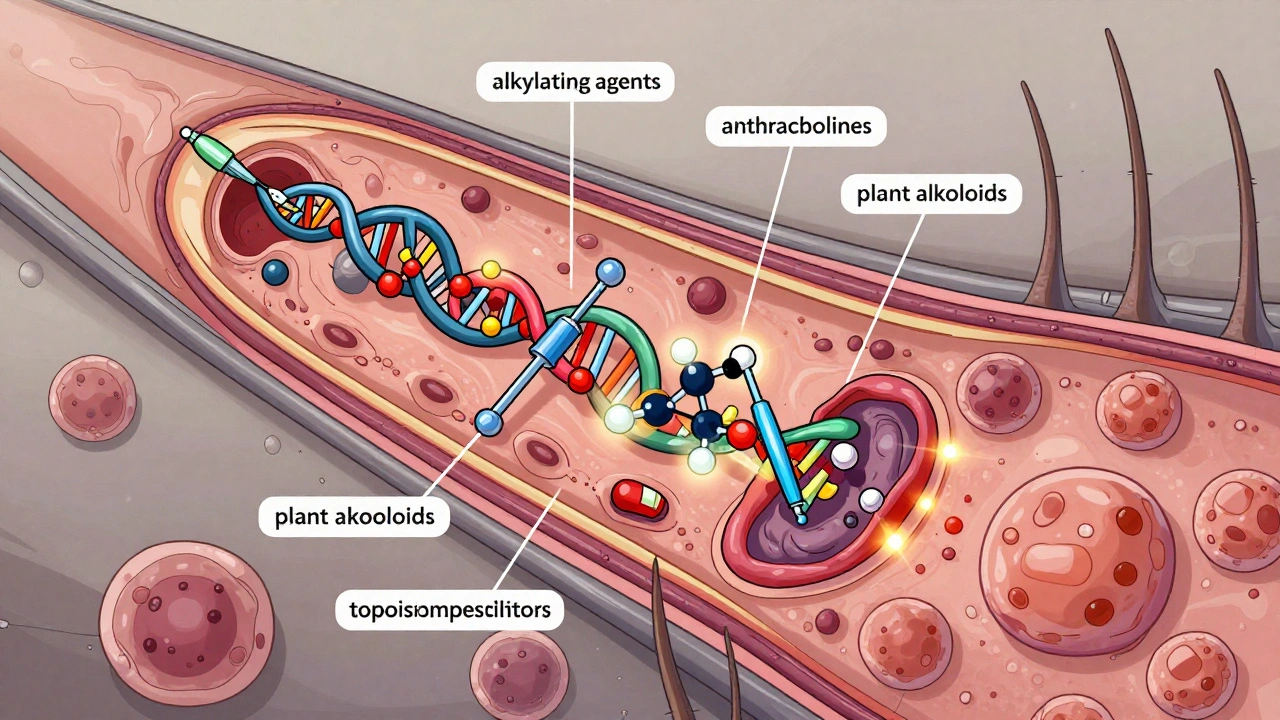
Chemotherapy drugs are called cytotoxic because they’re designed to kill cells. They don’t care if a cell is cancerous or not - they go after anything that’s dividing quickly. That’s the key. Cancer cells multiply nonstop. Healthy cells usually take breaks. Chemo exploits that difference. There are over 100 different chemotherapy drugs, grouped into six main types based on how they work. Alkylating agents like cyclophosphamide damage DNA directly, making it impossible for the cell to copy itself. Antimetabolites like 5-fluorouracil pretend to be nutrients the cell needs, then sabotage DNA and RNA production. Anthracyclines, such as doxorubicin, slip into the DNA double helix and snap it apart. Plant alkaloids like vincristine freeze the cell’s internal skeleton during division, trapping it mid-split. Topoisomerase inhibitors like etoposide stop enzymes that untangle DNA before replication. Each type hits at a different stage of the cell cycle. Most chemotherapy is given through an IV - about 65% of treatments. Some, like capecitabine (Xeloda), are pills you take at home. Others go directly into the spinal fluid, the abdomen, or even an artery feeding the tumor. Treatment isn’t continuous. It’s given in cycles - two to six weeks apart - so your body can recover. A single infusion might last 20 minutes or stretch over three days, depending on the drug. For breast cancer, paclitaxel (Taxol) is often given at 175 mg per square meter of body surface every three weeks. That’s not random. It’s based on decades of research showing that’s the sweet spot between killing cancer and letting healthy cells bounce back.Why Chemotherapy Still Matters in 2025
You might hear that targeted therapies and immunotherapies are replacing chemo. That’s true - in some cases. For metastatic breast cancer with HER2 mutations, drugs like trastuzumab can work better with fewer side effects. In lung cancer with EGFR or ALK mutations, targeted pills often come first. But chemo is still the backbone for a lot of cancers. It’s used in 95% of ovarian cancer cases, 85% of colorectal cancers, and 70% of breast cancers. Why? Because it works where other drugs don’t. It doesn’t need a specific genetic marker. It doesn’t rely on your immune system being strong. It just kills fast-dividing cells - no questions asked. That makes it essential for cancers with mixed cell types, where some cells might be resistant to targeted drugs. It’s also the first-line treatment for 78% of blood cancers like acute myeloid leukemia and aggressive lymphomas. It’s also critical before surgery. In breast cancer, giving chemo before removing the tumor (called neoadjuvant therapy) can shrink tumors so much that a mastectomy becomes a lumpectomy. Studies show patients who achieve a complete pathologic response - meaning no cancer is left in the removed tissue - have much better long-term survival. That’s not a small win. It’s life-changing.The Real Side Effects: What Patients Actually Experience
Side effects aren’t just a list on a pamphlet. They’re daily realities. Fatigue hits hardest. Eighty-two percent of patients on Reddit’s cancer forums say it’s worse than nausea or hair loss. It’s not just being tired. It’s a bone-deep exhaustion that sleep doesn’t fix. A 2023 review of 17 trials found that 30 minutes of moderate exercise - a brisk walk, light cycling - cuts fatigue by 25 to 30%. That’s not a suggestion. It’s medical advice backed by data. Hair loss? Seventy-eight percent of patients report it. Scalp cooling caps, now recommended by the National Comprehensive Cancer Network, can cut that risk from 65% down to 25% for those on taxane-based chemo. But they’re not perfect. Some people still lose hair. Others get patchy regrowth. And the cold can be unbearable. Nausea has improved dramatically. In the 1980s, over 70% of patients on strong chemo regimens threw up. Today, thanks to drugs like ondansetron and aprepitant, that’s down to 10-20%. But here’s the catch: those drugs work great for the first 24 hours. After that, delayed nausea kicks in. Only 32% of patients say anti-nausea meds help with nausea that starts a day or two after treatment. That’s when eating small, bland meals - toast, rice, bananas - becomes your best friend. Then there’s chemo brain. Seventy-five percent of patients report trouble focusing, memory lapses, mental fog during treatment. One in three still feel it six months later. It’s not in their head. Brain scans show real changes in activity patterns. Meditation apps like Calm or Headspace, used 20 minutes a day, have been shown in studies to reduce these symptoms by 30-40%. It’s not a cure. But it’s a tool. Peripheral neuropathy - tingling, numbness, or pain in hands and feet - affects 30-40% of people on taxanes or platinum drugs. Five to ten percent end up with permanent nerve damage. The key? Report it early. Avoid cold drinks, wear gloves when washing dishes, don’t walk barefoot. Your doctor might lower the dose or switch drugs if it gets bad.What No One Tells You About Managing Side Effects
Most people think side effects are just something you endure. But smart management changes everything. Hydration matters. Drinking 1-2 liters of water a day helps flush toxins and reduces fatigue and constipation. It’s simple. But most patients forget until they’re dizzy. Nutrition isn’t about eating healthy. It’s about eating something. If you can’t stand meat, try eggs. If you hate the taste of water, try flavored ice chips. The metallic taste? Try lemon water or sucking on hard candy. It’s not glamorous, but it keeps calories and nutrients coming. Neutropenic fever - a temperature of 100.4°F or higher with low white blood cells - is a medical emergency. You don’t wait. You call your oncology team immediately. Infections can turn deadly fast when your immune system is down. And then there’s the emotional stuff. Hair loss isn’t just cosmetic. It’s identity. A woman in Auckland told me her daughter cried every morning when she saw her bald head in the mirror. That’s why some clinics now offer wig fittings and scarves before treatment even starts. Support groups, whether online or in person, aren’t optional. They’re part of the treatment plan.What’s New in Chemotherapy (2025)
The field isn’t standing still. In 2023, the FDA approved trilaciclib (Cosela), the first drug designed to protect bone marrow during chemo. It doesn’t stop cancer. It gives your blood cells a shield. That means fewer transfusions, fewer infections, and less time spent in the hospital. Medical cannabis is gaining traction. A 2023 study showed CBD and THC combinations reduced neuropathic pain by 55% in patients who didn’t respond to standard painkillers. It’s not approved everywhere, but it’s being studied seriously. Scalp cooling is now standard in many centers. It’s not magic, but for breast cancer patients on taxanes, it’s a game-changer. Many choose it not just for appearance, but for dignity. The biggest shift? Chemo is no longer used alone. It’s paired with immunotherapy. For lung cancer, for melanoma, for bladder cancer - combining chemo with drugs that wake up the immune system has improved survival rates. The future isn’t chemo or targeted therapy. It’s chemo and targeted therapy - together.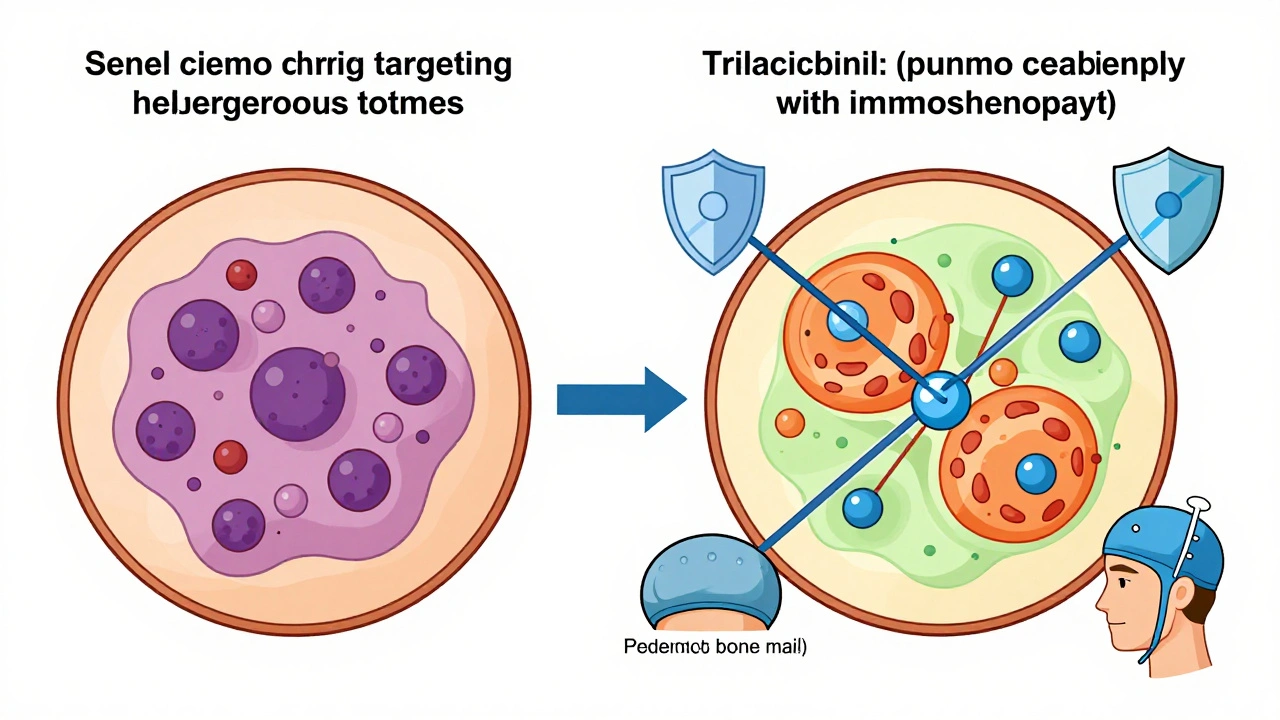
When Chemotherapy Isn’t the Answer
It’s not for everyone. Some cancers, like slow-growing prostate cancer, respond far better to hormone therapy. Giving chemo there does more harm than good. The goal isn’t to use chemo as much as possible. It’s to use it where it works best. Doctors now test tumors for genetic markers before deciding. If a tumor has a targetable mutation, they’ll often start with a pill that only hits that mutation - fewer side effects, better outcomes. Chemo is saved for when those options run out, or when the cancer is too aggressive to wait.What Patients Need to Know
You’re not alone. You’re not weak. You’re not failing if you struggle. Side effects aren’t a sign the treatment isn’t working - they’re proof it’s working on your body too. Track your symptoms. Write down when nausea hits, how tired you feel, what helps. Bring it to your appointments. Your oncologist can’t help if they don’t know. Ask about supportive care. There are specialists in nutrition, physical therapy, mental health, and pain management who work alongside your oncologist. They’re part of your team. And remember: this isn’t forever. Most chemo cycles last three to six months. You will get through it. Not because you’re strong. Because you’re human. And humans adapt.Does chemotherapy always cause hair loss?
No. Hair loss depends on the drug, dose, and individual biology. Some chemo drugs, like capecitabine or vinblastine, rarely cause it. Others, like doxorubicin or paclitaxel, almost always do. Scalp cooling caps can reduce hair loss by up to 60% in patients receiving taxane-based regimens. Not everyone qualifies, but it’s an option worth asking about.
Can you work during chemotherapy?
Many people do - but it’s different for everyone. Fatigue and chemo brain make focus hard. Some work remotely, reduce hours, or take days off around treatment days. Studies show 57% of working patients report cognitive issues affecting their job performance. Talk to your employer about accommodations. You’re protected under disability laws in most countries.
Is chemotherapy painful?
The infusion itself usually isn’t painful - it feels like getting an IV for fluids. But side effects can be. Nerve pain from neuropathy, mouth sores, muscle aches, and abdominal cramps from diarrhea are common. Pain isn’t inevitable. Medications like gabapentin, lidocaine patches, or even low-dose antidepressants can help. Tell your team if you’re hurting. There’s always something to try.
How do you know if chemotherapy is working?
You won’t feel it. Tumors shrink slowly. Doctors use scans (CT, MRI, PET), blood tests, and tumor markers to track progress. Sometimes, the first sign is that side effects are getting worse - meaning the drugs are hitting cells hard. Don’t wait for symptoms to change. Trust the tests. And remember: even if the tumor doesn’t disappear, slowing its growth is a win.
Can chemotherapy cause cancer?
Rarely, yes. Some chemo drugs, especially alkylating agents and topoisomerase inhibitors, can damage DNA in healthy cells enough to cause a second cancer years later. The risk is low - about 1-2% over 10 years - and is weighed against the immediate threat of the original cancer. For most, the benefit far outweighs the risk. Your oncologist will discuss this if your treatment plan includes high-risk drugs.
Why do some people need chemo after surgery?
Even if the surgeon removes the tumor, microscopic cancer cells might still be floating in your body. That’s called micrometastasis. Chemo after surgery - called adjuvant therapy - kills those hidden cells. It’s not about what you can see. It’s about what you can’t. Studies show it cuts recurrence risk by 30-50% in breast, colon, and lung cancers.
Are there natural ways to reduce chemo side effects?
Some strategies are backed by science: acupuncture for nausea, ginger for vomiting, meditation for brain fog, and moderate exercise for fatigue. But don’t rely on supplements. Many - like high-dose antioxidants - can interfere with chemo’s ability to kill cancer cells. Always check with your oncologist before taking anything new, even vitamins.
How long do side effects last after chemo ends?
Most fade within weeks or months. Fatigue, brain fog, and neuropathy can linger for six months to a year. For some, nerve damage or early menopause is permanent. Recovery isn’t linear. Some days are better than others. Give yourself time. Support groups and rehab programs can help rebuild strength and confidence.






8 Comments