For decades, obesity was seen as a simple matter of eating too much and moving too little. If you just had more willpower, the thinking went, you could lose the weight. But that idea doesn’t match what science now knows. Obesity isn’t a lifestyle choice-it’s a chronic, progressive disease. It’s not about laziness. It’s about biology. Your body’s hormones, brain signals, fat tissue function, and even your genes are working against you in ways most people don’t understand.
Why Obesity Is a Disease, Not a Choice
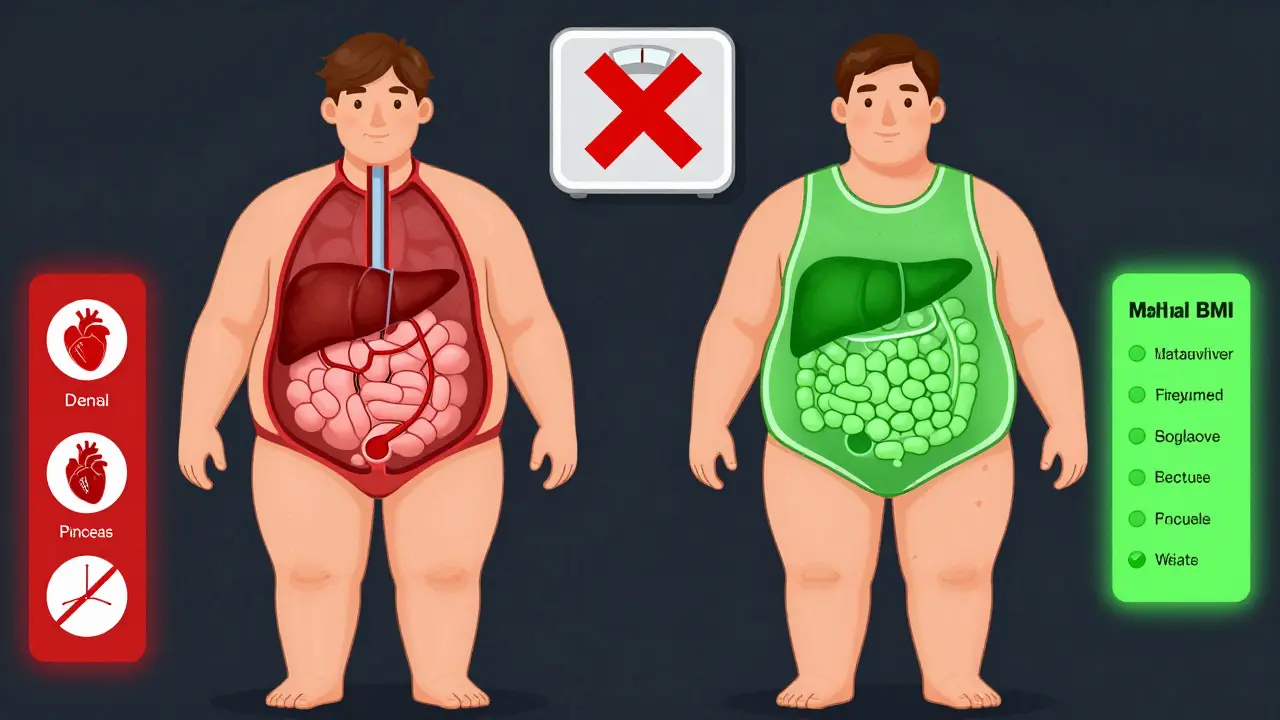
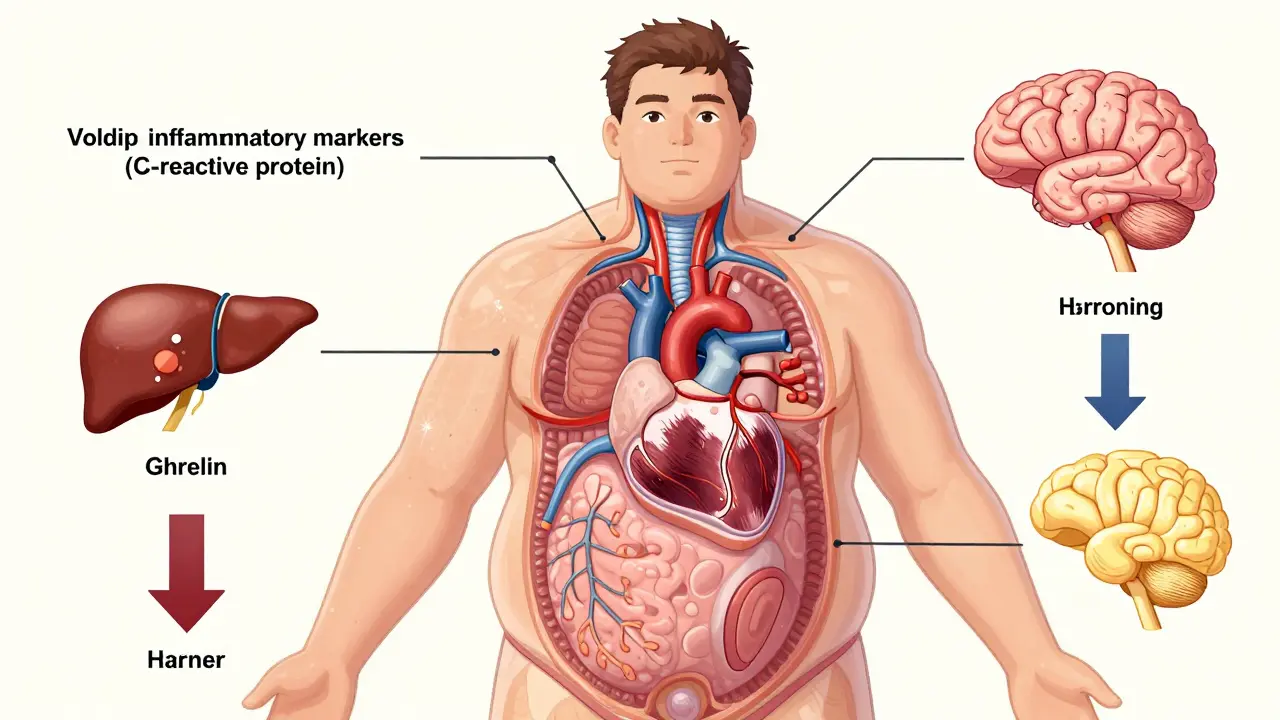
In 2013, the American Medical Association officially recognized obesity as a disease. That wasn’t just a change in wording-it changed how doctors think about treatment. Before that, many saw obesity as a personal failure. Now, they’re trained to treat it like diabetes or high blood pressure: with ongoing care, medication, and lifestyle support. The World Health Organization defines obesity as a body mass index (BMI) of 30 or higher. But BMI alone doesn’t tell the whole story. Two people can have the same BMI, but one might have dangerous fat buildup around the liver and heart, while the other stores fat mostly under the skin. That’s why experts now focus on metabolic health, not just the number on the scale. Obesity triggers real changes in your body. Fat tissue isn’t just storage-it becomes inflamed. It releases chemicals that mess with insulin, raise blood pressure, and increase cancer risk. People with obesity often have 2 to 3 times higher levels of C-reactive protein, a key marker of body-wide inflammation. That’s not something you can fix with a diet. That’s a disease process.The Biology Behind Weight Gain and Regain
Your body doesn’t want you to lose weight. Not because you’re weak, but because evolution wired you to survive famines. When you lose weight, your body fights back. Hunger hormones like ghrelin go up. Satiety hormones like leptin drop. Your metabolism slows down. Studies show that after losing weight, your body burns 300-500 fewer calories per day than someone who never lost weight-even if you’re the same size. That’s why 90% of people who lose weight through dieting alone regain it within five years. There’s also a psychological loop. Carrying extra weight makes movement harder, which reduces daily activity by 15-20%. Less movement means fewer calories burned. Stress from stigma or frustration raises cortisol, which increases cravings for sugary, fatty foods. Poor sleep-common in people with obesity-cuts leptin by 18% and spikes ghrelin by 15%, making you hungrier the next day. And genetics? They play a huge role. Twin studies show 40-70% of obesity risk comes from genes. Over 250 gene variants have been linked to body weight. Some people have mutations in the MC4R gene, which controls appetite. That’s not a choice. That’s biology.Metabolic Health: It’s Not Just About the Scale
You can be overweight and metabolically healthy. You can also be normal weight and metabolically unhealthy. That’s why doctors now look beyond BMI. Key markers of metabolic health include:- Insulin sensitivity (how well your body uses sugar)
- Triglyceride and HDL cholesterol levels
- Blood pressure
- Waist circumference (over 40 inches for men, 35 for women signals higher risk)
- Liver fat (non-alcoholic fatty liver disease affects 75% of people with BMI over 35)
Effective Weight Strategies: What Actually Works
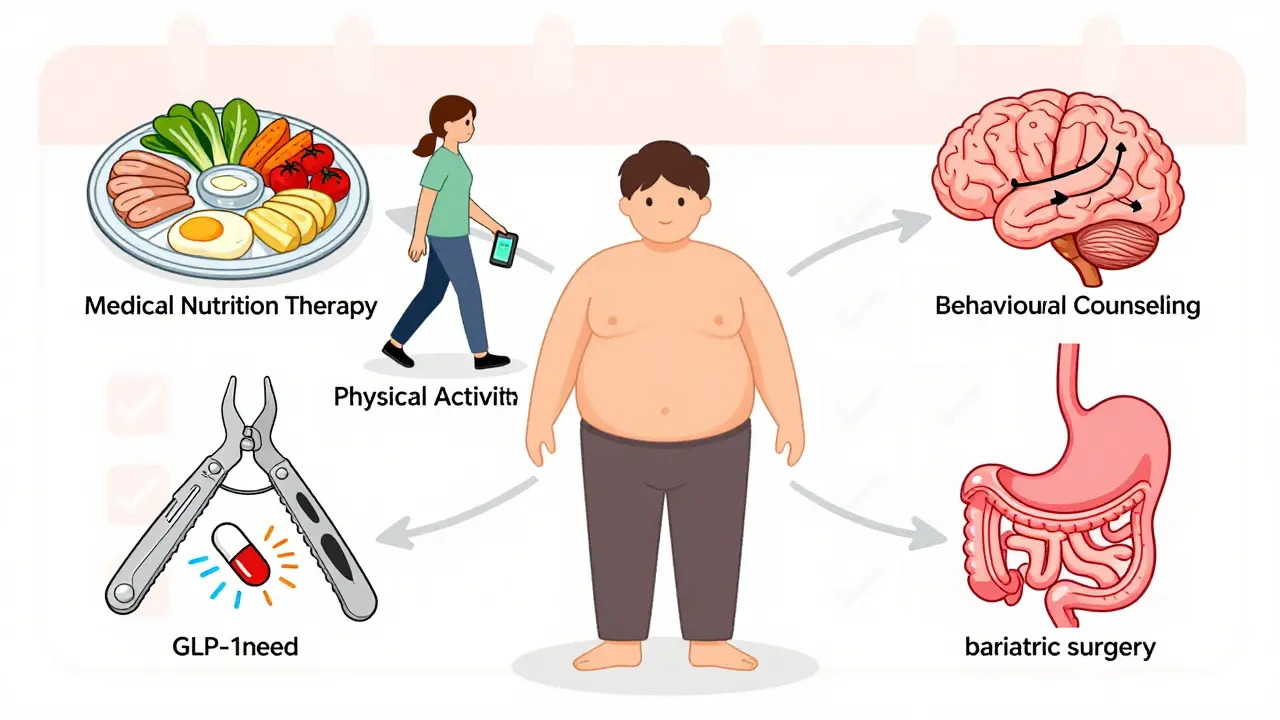
There’s no magic pill. But there are proven, science-backed approaches that work when used together. 1. Medical Nutrition TherapyNot every dietitian is trained for obesity. Look for someone certified in obesity medicine. They don’t just tell you to eat less. They help you build sustainable habits-portion control, mindful eating, meal timing, and food choices that stabilize blood sugar. Studies show each extra hour of counseling leads to 0.23% more weight loss. That adds up. 2. Physical Activity
You don’t need to run marathons. Just 150 minutes a week of moderate exercise-brisk walking, cycling, swimming-cuts heart disease risk by 30% and improves insulin sensitivity. Movement doesn’t have to be intense. It just has to be consistent. 3. Behavioral Counseling
This is where most programs fail. People lose weight but don’t learn how to keep it off. Counseling helps you identify triggers, manage stress without food, handle setbacks, and build a support system. The Obesity Medicine Association recommends at least 14 hours of this over six months for meaningful results. 4. Medications
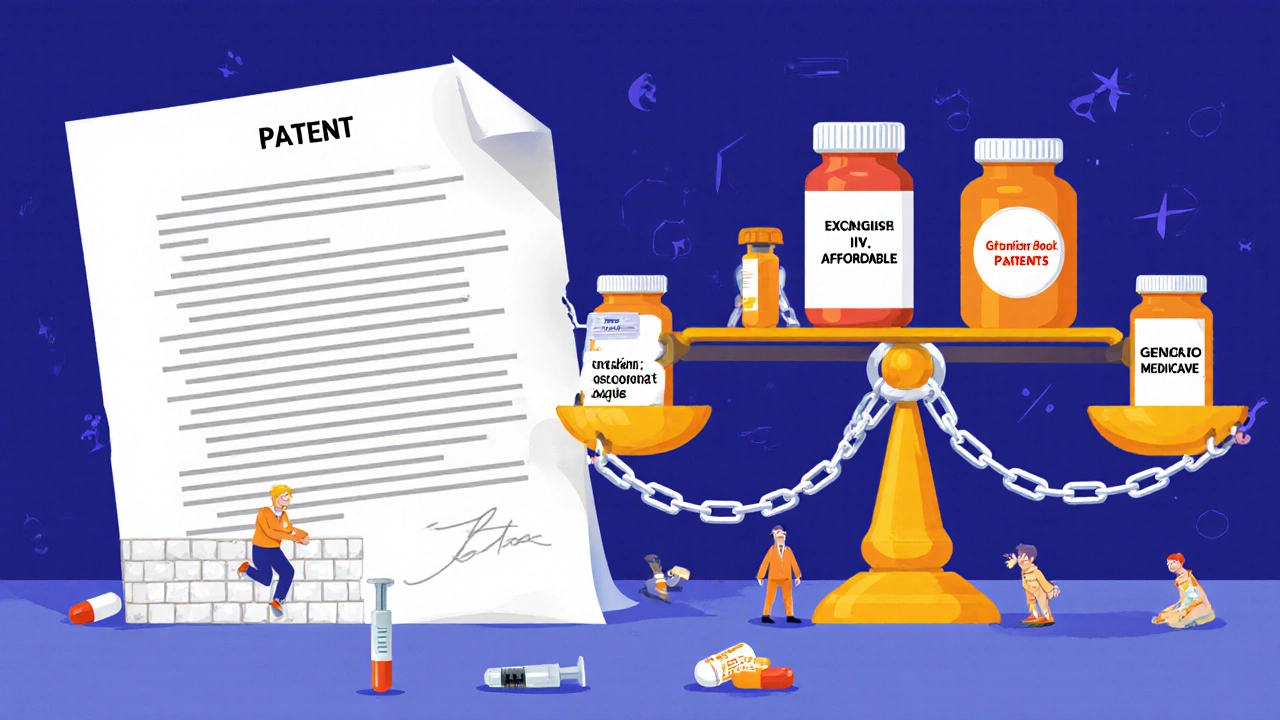
Five FDA-approved drugs are now available for chronic weight management. The most effective are GLP-1 receptor agonists like semaglutide (Wegovy) and tirzepatide (Zepbound). In clinical trials, users lost 15-20% of their body weight over a year. That’s not a miracle-it’s biology working with the drug to reduce hunger and improve metabolism. Side effects like nausea are common but often fade. These aren’t shortcuts. They’re tools that help your body reset its weight set point. 5. Bariatric Surgery
For people with severe obesity (BMI ≥40 or ≥35 with complications), surgery is the most effective long-term treatment. Procedures like gastric bypass or sleeve gastrectomy change gut hormones, reduce appetite, and improve insulin sensitivity. About 87% of patients have insurance coverage if they meet criteria. But it’s not a cure. Lifelong vitamin monitoring and follow-up care are required. About 41% report vitamin deficiencies, and 29% deal with dumping syndrome.
Why Most Programs Fail-and What to Do Instead
Most weight loss programs are designed for short-term results. They promise 10 pounds in 10 days. They don’t prepare you for the biology that kicks in after you lose weight. Real success comes from treating obesity like any other chronic disease: with ongoing management. That means:- Regular check-ins with a doctor who understands obesity as a disease
- Medication when appropriate-not as a last resort, but as part of a plan
- Access to behavioral support, not just a pamphlet
- Insurance coverage that doesn’t require endless paperwork
The Future Is Here: New Treatments and Better Understanding
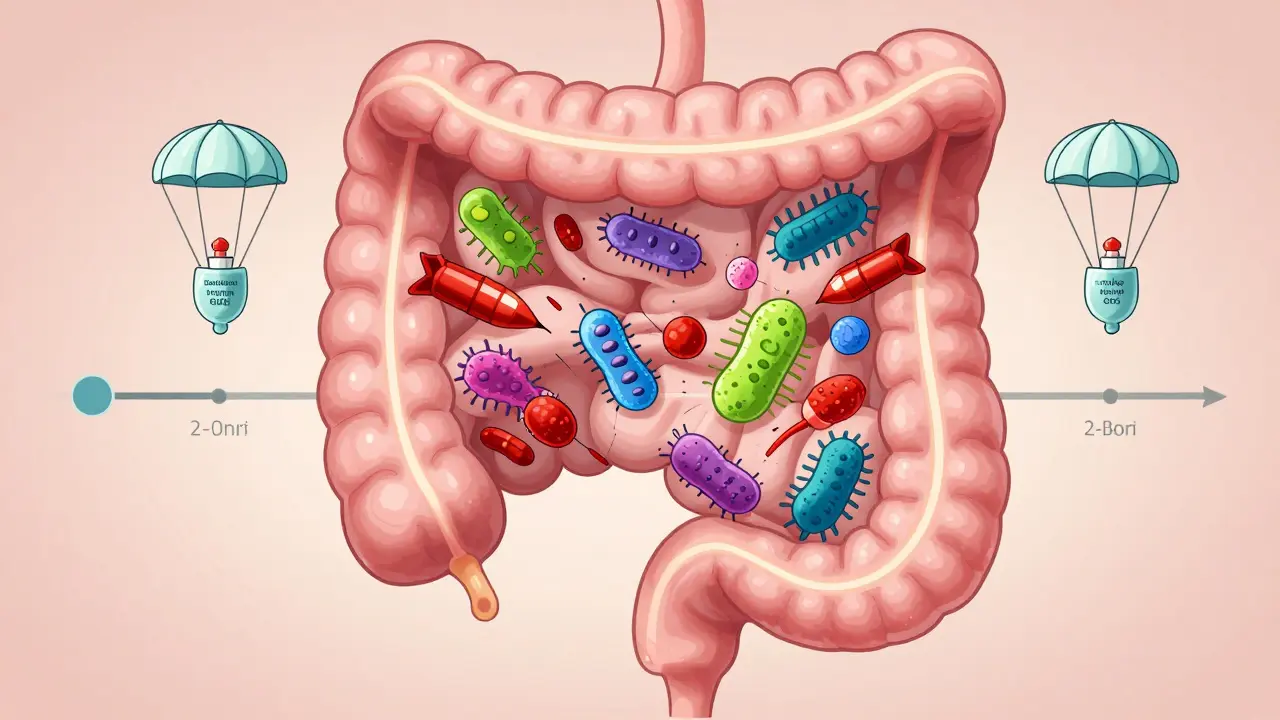
In July 2023, the FDA approved retatrutide, a triple hormone agonist that led to 24.2% average weight loss in trials-the most effective drug yet. The ICD-11 now includes detailed obesity staging that considers organ damage, not just BMI. And research into the gut microbiome shows certain bacteria are consistently lower in people with obesity, opening new doors for treatment. The American Heart Association now says obesity should be screened for like high cholesterol. That means checking for sleep apnea (affects 70% of people with obesity), fatty liver, and joint problems. These aren’t side effects-they’re part of the disease. The economic cost of obesity is $1.72 trillion globally. But integrated care models-combining digital tools, medication, and counseling-could cut U.S. healthcare costs by $190 billion annually by 2030. We have the tools. We just need to use them.What You Can Do Right Now
If you or someone you know is struggling with weight and metabolic health:- Ask your doctor: “Do you treat obesity as a chronic disease?” If they say no, find someone who does.
- Request screening for metabolic issues: blood sugar, liver enzymes, cholesterol, blood pressure.
- Don’t blame yourself. This isn’t about willpower. It’s about biology.
- Look for providers certified by the Obesity Medicine Association.
- Consider medication if lifestyle changes aren’t enough. It’s not failure-it’s medicine.
- Find support. Online communities like r/Obesity can help you feel less alone.
Is obesity really a disease, or just being overweight?
Yes, obesity is officially recognized as a chronic disease by the American Medical Association, the World Health Organization, and the Obesity Medicine Association. It’s not just being overweight-it’s a complex condition where excess fat causes harmful changes in hormones, inflammation, and organ function. BMI is a screening tool, but metabolic health, fat distribution, and organ damage are what define the disease.
Why do I keep gaining weight back after losing it?
Your body fights weight loss. After losing weight, hunger hormones increase, satiety hormones drop, and your metabolism slows down by 300-500 calories per day. This is a biological survival response, not a lack of willpower. That’s why 90% of people regain weight within five years on diets alone. Long-term success requires ongoing medical support, not just short-term changes.
Are weight-loss medications safe and effective?
Five FDA-approved medications are now available for chronic weight management, including semaglutide and tirzepatide. In clinical trials, they help people lose 15-24% of body weight. Side effects like nausea are common at first but usually improve. These drugs work by helping your brain reset its weight set point. They’re not magic pills, but they’re proven tools that work better than dieting alone-especially when combined with lifestyle changes.
Does bariatric surgery work long-term?
Yes, for people with severe obesity, bariatric surgery is the most effective long-term treatment. Studies show 70-80% of patients keep off 50% or more of their excess weight after 10 years. It also improves or resolves type 2 diabetes in 80% of cases. But it’s not a quick fix. Lifelong vitamin monitoring, follow-up care, and dietary changes are required. About 41% of patients develop vitamin deficiencies, so regular blood tests are essential.
Can you be healthy at a higher weight?
Yes. You can have a higher BMI but still have healthy blood pressure, normal blood sugar, good cholesterol, and no fatty liver. That’s called metabolically healthy obesity. The real goal isn’t just losing weight-it’s improving metabolic health. Focusing only on the scale misses the bigger picture. Improving movement, sleep, stress, and nutrition can reduce disease risk even if the number on the scale doesn’t change much.
Why don’t doctors treat obesity better?
Many doctors weren’t trained to treat obesity as a disease. Only 10% of U.S. medical schools require obesity education. Insurance often doesn’t cover medications or counseling. And weight stigma is still common-67% of patients report being judged by healthcare providers. Change is happening, but slowly. If your doctor doesn’t offer evidence-based treatment, ask for a referral to an obesity medicine specialist.



9 Comments