Most people don’t talk about hemorrhoids-until they have them. Then it’s all you can think about. Burning. Itching. Pain when you sit. Bright red blood on the toilet paper. You might feel embarrassed, but you’re not alone. About 75% of people will deal with hemorrhoids at some point in their lives. The good news? They’re treatable. And understanding the difference between internal and external hemorrhoids is the first step to getting relief.
What Exactly Are Hemorrhoids?
Hemorrhoids aren’t some strange growth or infection. They’re normal blood vessels in your rectum and anus that help with stool control. Think of them like cushions that support the anal sphincter. But when pressure builds up-because of constipation, pregnancy, long hours sitting, or heavy lifting-these veins swell, stretch, and become irritated. That’s when they turn into a problem.
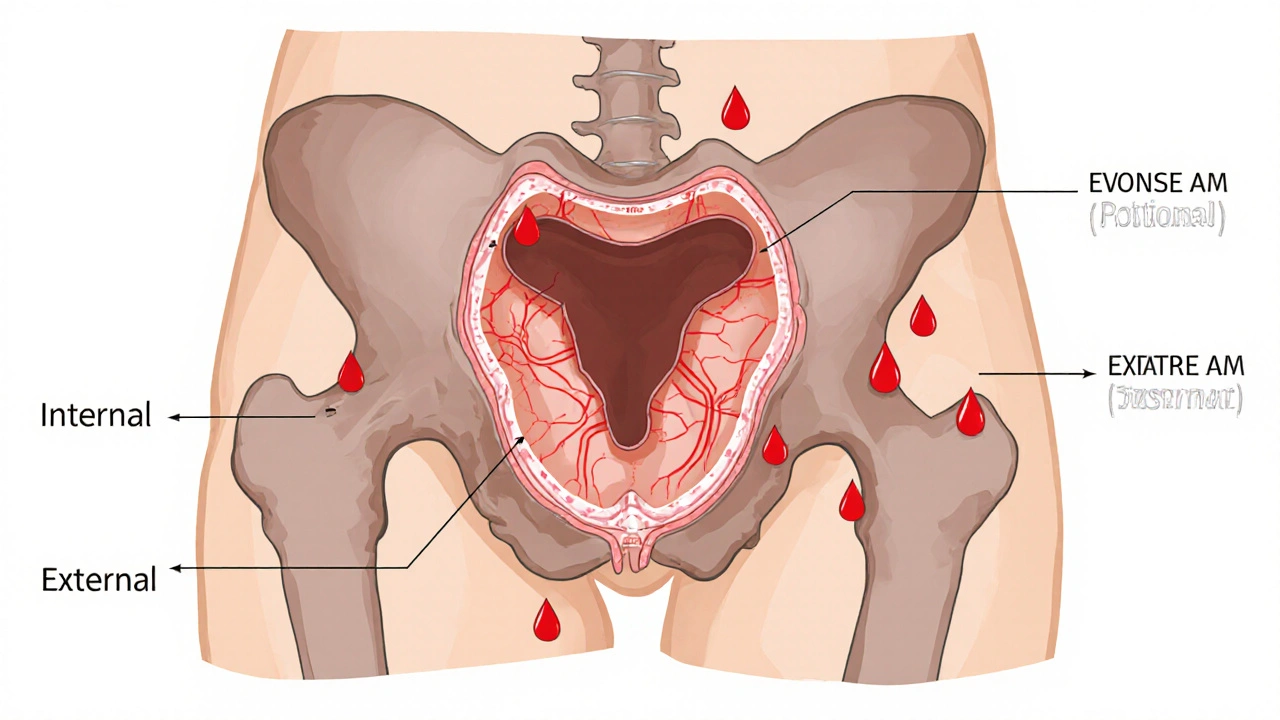
There are two main types, and they’re not the same. Where they form makes all the difference in how they feel and how they’re treated.
Internal Hemorrhoids: Silent But Not Harmless
Internal hemorrhoids form inside the rectum, above the dentate line. This area has no pain receptors, so even when they swell, you might not feel pain-at least not at first. That’s why so many people don’t realize they have them until they see blood.
The main symptom? Bright red blood during or after a bowel movement. You might notice it on the toilet paper, in the bowl, or streaked on your stool. Sometimes you’ll feel like you haven’t fully emptied your bowels, or you’ll feel a sense of fullness in your rectum. These are classic signs of Grade I or II internal hemorrhoids.
As they get worse, they can prolapse-meaning they push out through the anus. Grade III hemorrhoids come out during bowel movements but can be pushed back in. Grade IV are stuck outside and can’t be pushed back. That’s when things get uncomfortable, even if they don’t hurt. Prolapsed internal hemorrhoids often bleed more and can get irritated by clothing or wiping.
External Hemorrhoids: Painful and Visible
External hemorrhoids form under the skin around the anus. This area is packed with nerves. So when these veins swell, you feel it. A lot.
You’ll likely notice a soft, skin-colored lump near your anus. It might itch, burn, or ache-especially when you sit. The pain gets worse with pressure. If a blood clot forms inside the hemorrhoid, it becomes a thrombosed external hemorrhoid. That’s when things turn serious.
Thrombosed hemorrhoids look like firm, purple or blue lumps. They hurt. Badly. The pain hits suddenly, often after straining or lifting something heavy. Sitting becomes torture. Walking can feel uncomfortable. You might even feel like you can’t sit down at work or drive without wincing.
And here’s something people don’t realize: you can have both internal and external hemorrhoids at the same time. That’s why symptoms can feel confusing. Is the bleeding from inside? Is the pain from outside? A doctor can tell you for sure.
What Else Could It Be?
Not every bit of blood or lump is a hemorrhoid. Anal fissures-tiny tears in the lining of the anus-also cause bleeding and pain. But the pain from a fissure is sharp and tearing, usually right after a bowel movement. Hemorrhoids cause more of a dull ache or constant pressure. Fissures rarely cause swelling or lumps you can feel.
And here’s the big one: rectal bleeding can be a sign of something more serious-like colorectal cancer, inflammatory bowel disease, or polyps. That’s why if you’re over 45, or if you’ve never had a colonoscopy, or if the bleeding keeps coming back despite treatment, you need to see a doctor. Don’t assume it’s just hemorrhoids.
Home Treatments That Actually Work
For mild cases, you don’t need surgery. You need better habits.
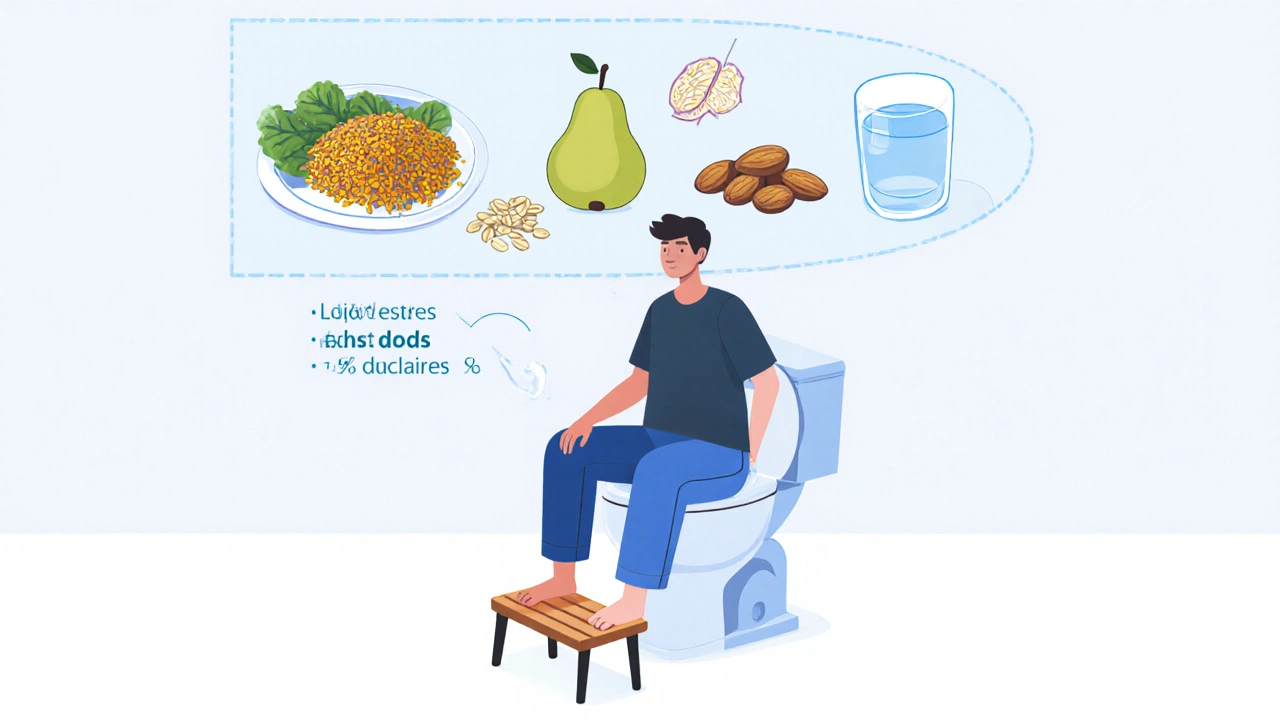
- Eat more fiber. Aim for 25-30 grams a day. That’s a cup of cooked lentils, a medium pear with skin, a cup of oats, and a handful of almonds. Fiber softens stool so you don’t have to strain.
- Drink water. At least 8-10 glasses a day. Fiber without enough water just makes things worse.
- Don’t sit on the toilet for long. Five minutes max. Reading the news or scrolling on your phone adds pressure. Use a small footstool to raise your knees above your hips-that reduces rectal pressure by about 30%.
- Try sitz baths. Sit in warm (not hot) water for 15-20 minutes, 2-3 times a day. It reduces swelling and soothes irritation.
- Use over-the-counter creams. Hydrocortisone cream helps with itching. Witch hazel pads can reduce swelling. But don’t use them for more than a week without checking with a doctor.
These steps won’t make hemorrhoids vanish overnight. But they stop them from getting worse-and they help most people feel better within a few days.
When You Need More Than Home Care
If home treatments don’t help after a week, or if symptoms are severe, it’s time to see a specialist.
For internal hemorrhoids, doctors have several minimally invasive options:
- Rubber band ligation: A tiny band is placed around the base of the hemorrhoid to cut off blood flow. It falls off in a few days. It’s 90% effective for Grades I-III. You might feel pressure or cramping for 24-48 hours after.
- Sclerotherapy: A chemical solution is injected into the hemorrhoid to shrink it. Less painful than banding, but slightly less effective.
- Infrared coagulation: Heat is used to scar the tissue and shrink the hemorrhoid. Good for small ones.
For thrombosed external hemorrhoids, the fastest relief comes from a simple procedure: a small cut to drain the clot. Done within 72 hours of the pain starting, it cuts recovery time in half. After that, the body slowly reabsorbs the clot, but the pain can last for weeks.
If you have large, recurring, or Grade IV hemorrhoids, surgery might be needed:
- Hemorrhoidectomy: The hemorrhoid is completely removed. It’s the most effective option-95% success rate. But recovery takes 2-4 weeks. Pain is common, and you’ll need prescription pain meds.
- Stapled hemorrhoidopexy: The tissue is lifted back into place and stapled. Less pain than removal, but higher chance of recurrence.
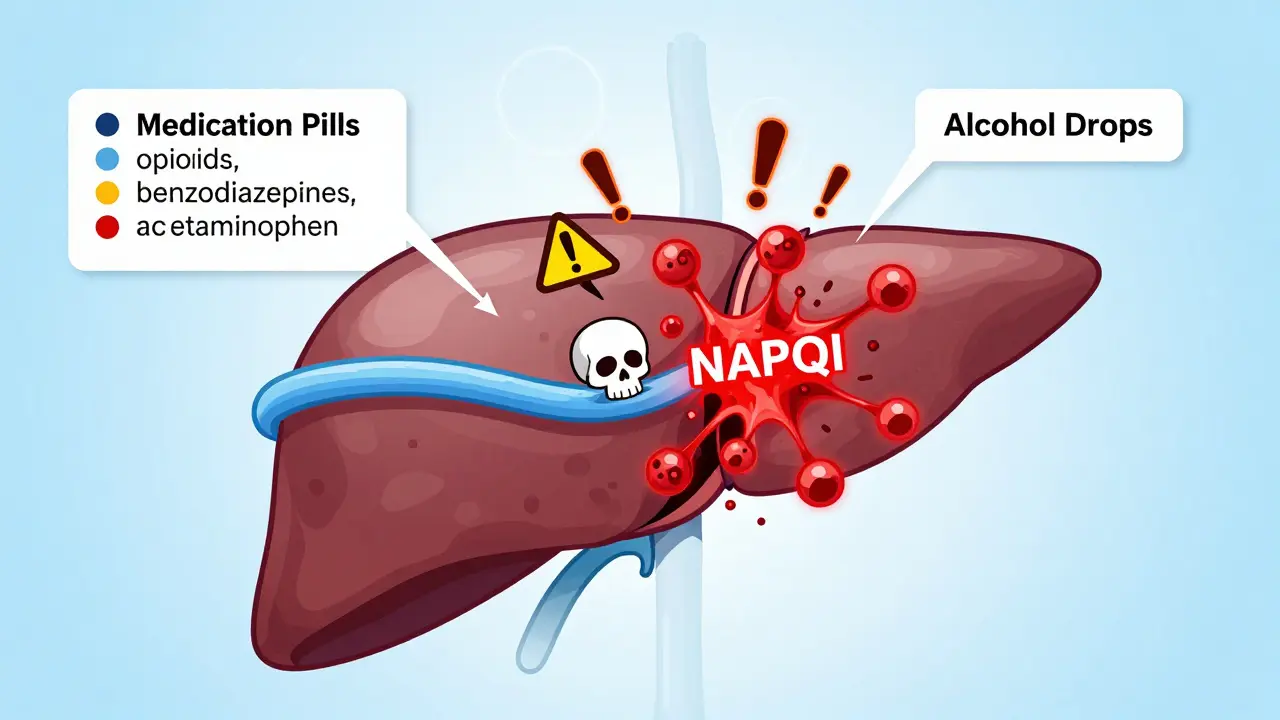
What Doesn’t Work (And Why You Should Avoid It)
There are tons of products online promising “miracle cures” for hemorrhoids: herbal oils, unregulated creams, detox teas, even devices that claim to shrink them with magnets or lasers.
None of them are backed by science. The American Gastroenterological Association and the American Society of Colon and Rectal Surgeons warn against them. Some can irritate the skin even more. Others delay real treatment, letting the problem get worse.
Stick to what’s proven: fiber, water, sitz baths, and doctor-approved procedures.
Prevention Is the Best Treatment
Hemorrhoids come back if you don’t change your habits. Studies show that if you stick to a high-fiber diet and avoid straining, your chance of recurrence drops to 5-10%. Without changes, it’s 50%.
For pregnant women-who have a 25-35% risk-pelvic floor exercises and sleeping on your left side help reduce pressure on the veins. Don’t wait until you’re in pain to start.
And if you’re sitting at a desk all day? Get up every hour. Walk for two minutes. Even standing helps. Pressure builds slowly. Small movements make a big difference.
When to See a Doctor
You don’t need to suffer in silence. See a doctor if:
- Bleeding continues after a week of home care
- You have severe pain, especially with a hard lump
- You feel dizzy or weak (signs of significant blood loss)
- Your bowel habits change-new constipation, diarrhea, or narrower stools
- You’re over 45 and haven’t had a colonoscopy
It’s not weakness to ask for help. It’s smart.
Can internal hemorrhoids turn into external ones?
No, they don’t turn into each other. They form in different areas. But an internal hemorrhoid can prolapse and hang outside the anus, which might look like an external one. The tissue is still the same-just in a different position. That’s why doctors check for both types together.
Is it safe to pop a thrombosed hemorrhoid at home?
Never try to pop or cut into a hemorrhoid yourself. You risk infection, excessive bleeding, or scarring. Thrombosed hemorrhoids need professional care. A simple 10-minute procedure in the doctor’s office can drain the clot and relieve pain within hours.
Do hemorrhoids go away on their own?
Small hemorrhoids can shrink on their own with better diet and hydration, usually within a few days. But they rarely disappear completely unless treated. Without lifestyle changes, they’ll likely come back. Think of it like a sprained ankle-you can rest it, but if you keep running on it, it won’t heal.
Can stress cause hemorrhoids?
Stress doesn’t directly cause hemorrhoids, but it can lead to behaviors that do. People under stress often eat less fiber, drink less water, and hold in bowel movements. Stress can also cause muscle tension and straining. So while it’s not the root cause, it’s a major contributor.
Will hemorrhoids affect my sex life?
External hemorrhoids can make anal sex painful or uncomfortable. Internal ones usually don’t interfere unless they’re prolapsed or bleeding. If you’re experiencing discomfort, wait until symptoms improve. Don’t push through pain-it can worsen swelling or cause tears. Talk to your doctor if it’s a recurring issue.
Can I exercise with hemorrhoids?
Yes-just avoid heavy lifting or exercises that increase abdominal pressure like squats or deadlifts until things calm down. Walking, swimming, and cycling are great. Exercise helps prevent constipation and improves circulation. But if you feel pain during a workout, stop. It’s a sign you’re putting too much strain on the area.




13 Comments