When your shoulder starts to hurt and won’t move-no matter how hard you try-you’re not just having a bad day. You might be dealing with frozen shoulder, or adhesive capsulitis. It doesn’t come from a fall, a sports injury, or lifting something heavy. It creeps in slowly. At first, it’s just a dull ache that gets worse at night. Then, you notice you can’t reach behind your back, comb your hair, or even put on a coat without pain. And no matter how much you stretch, it doesn’t get better. That’s because this isn’t a muscle issue. It’s your shoulder joint capsule, the bag of tissue that holds everything together, slowly shrinking and tightening like a dried-out rubber band.
What’s Really Happening Inside Your Shoulder?
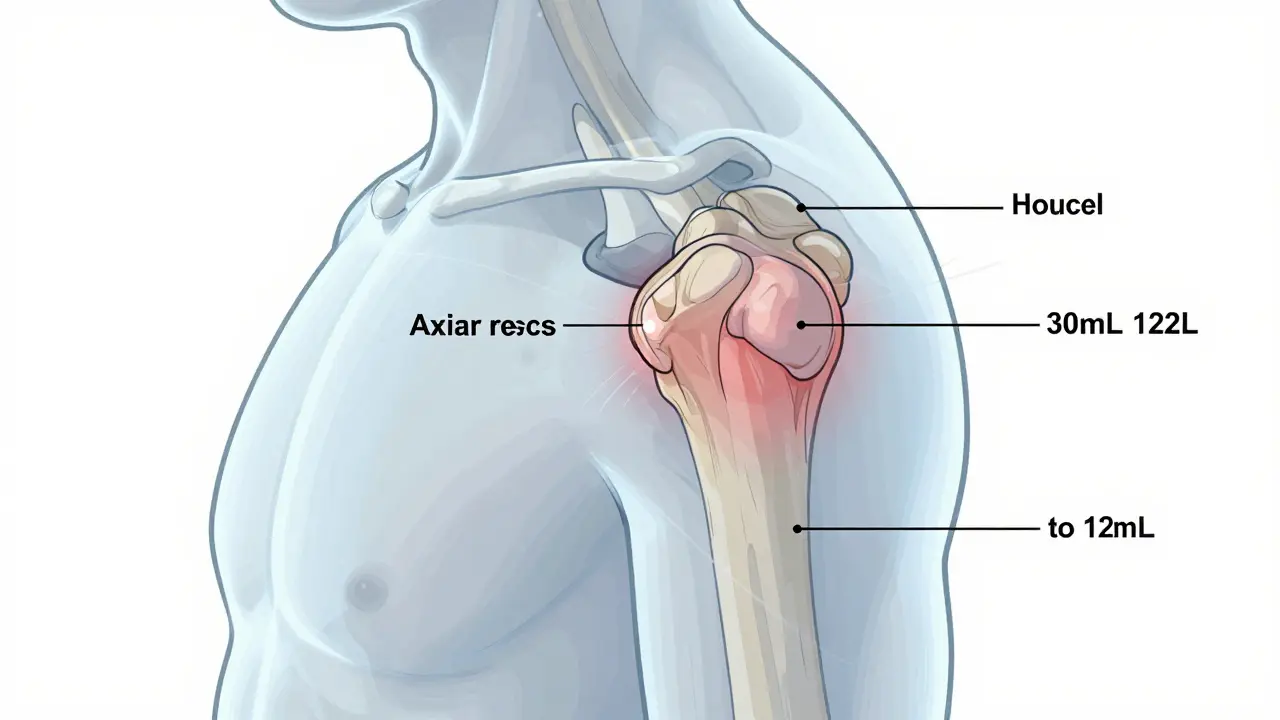
Adhesive capsulitis isn’t about adhesions sticking things together, despite what the name suggests. Histology studies show the joint capsule thickens, inflames, and contracts-losing nearly half its volume. A healthy shoulder capsule holds about 30-35 milliliters of fluid. In frozen shoulder, that drops to just 10-15 mL. This isn’t just stiffness. It’s structural change. The most affected areas? The front and top of the joint, especially the axillary recess and coracohumeral ligament. These are the spots that normally let your arm rotate freely. When they tighten, your shoulder locks up.
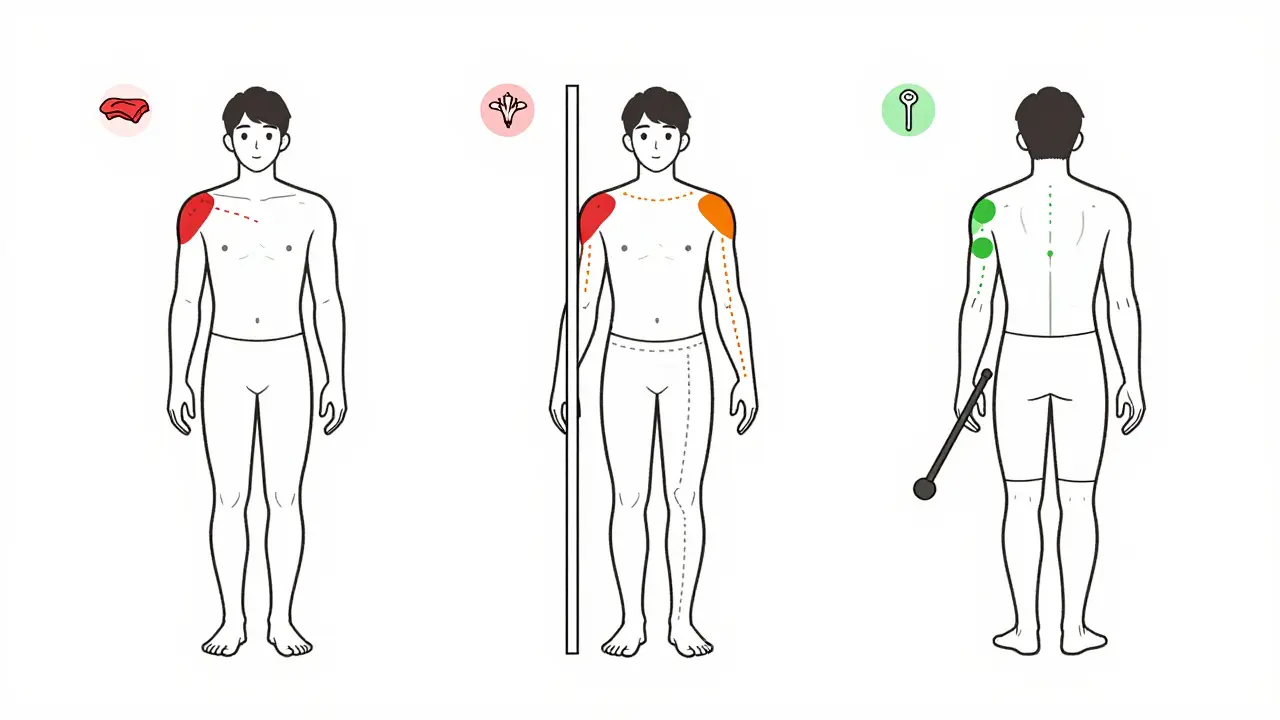
The pattern of restriction is unmistakable. External rotation (turning your palm up while your elbow is at your side) is the first to go-often 60-70% lost. Then comes abduction (raising your arm out to the side), followed by internal rotation (reaching behind your back). This exact order is a fingerprint for frozen shoulder. If you can still move your shoulder passively-someone else moves it for you-it’s not a rotator cuff tear. That’s a key difference. With a torn rotator cuff, you can’t lift your arm on your own, but someone else can still move it. With frozen shoulder, even passive movement is restricted. That’s why misdiagnosis is so common. Up to 40% of cases in primary care are initially labeled as tendonitis or arthritis.
The Three Stages: What to Expect and When to Act
Frozen shoulder doesn’t hit you all at once. It unfolds in three clear stages, each with its own rules for what helps and what hurts.
Stage 1: Freezing (6 weeks to 9 months)-This is the pain phase. Your shoulder aches constantly, especially at night. You might wake up because your arm feels locked. Movement triggers sharp pain. This is the most critical time to act. Many people rest, thinking they need to let it calm down. But research shows that gentle, consistent movement during this stage cuts recovery time in half. The goal isn’t to force motion-it’s to prevent further tightening. Pain should guide you, not stop you. If it hurts more than a 5 out of 10 during movement, ease off.
Stage 2: Frozen (4 to 6 months)-Pain starts to fade, but stiffness stays. This is when you realize you can’t reach your back pocket, fasten a bra, or reach for a high shelf. The joint capsule is now in full contraction. This is the ideal window for mobilization. Your body isn’t in active inflammation anymore, so you can safely push further. This is when physical therapy makes the biggest difference. Studies show patients who start supervised therapy during this phase recover 28% faster than those who wait.
Stage 3: Thawing (6 months to 2 years)-Motion slowly returns. You don’t need aggressive treatment here. Just keep moving. Most people regain 80-90% of their range naturally. But if you skipped therapy earlier, this stage can drag on. The good news? 87% of people fully recover within two years, even without surgery.
Mobilization Strategies That Actually Work
Not every stretch helps. Some make it worse. The key is timing, technique, and consistency.
Pendulum exercises-Start here, especially in the freezing phase. Lean over a table, let your arm hang loose, and gently swing it like a pendulum. Do this for 5 minutes, 2-3 times a day. It’s low-risk, low-pain, and keeps the joint lubricated. One Reddit user reported gaining 20 degrees of external rotation in four weeks just by doing this before bed.
Towel stretch-Grab a towel with both hands. Hold one end with your good arm, the other with your affected arm. Use the good arm to gently pull the towel upward, guiding the stiff arm into a stretch. Keep your elbows straight. This targets internal rotation. Do it 3 times a day for 30 seconds each.
Doorway stretch-Stand in a doorway. Place your hand on the frame at shoulder height. Gently lean forward until you feel a stretch in the front of your shoulder. Hold for 30 seconds. Repeat 3 times. This loosens the tight front capsule.
Wand exercises-Use a broomstick or a specialized rehab wand. Lie on your back. Hold the wand with both hands. Slowly lift it overhead, letting your stiff arm follow as far as it can without pain. This helps regain abduction. Do 10 reps, twice daily.
Heat before stretching is non-negotiable. A warm shower or heating pad for 10 minutes loosens the capsule and makes stretches more effective. Never stretch cold.

What Doesn’t Work (And What Could Make It Worse)
Forcing your arm beyond pain doesn’t speed things up-it triggers more inflammation. One patient on Cleveland Clinic’s portal reported that a forced cross-body stretch during the freezing phase spiked his pain from 4/10 to 8/10 for three weeks. That’s not progress. That’s damage.
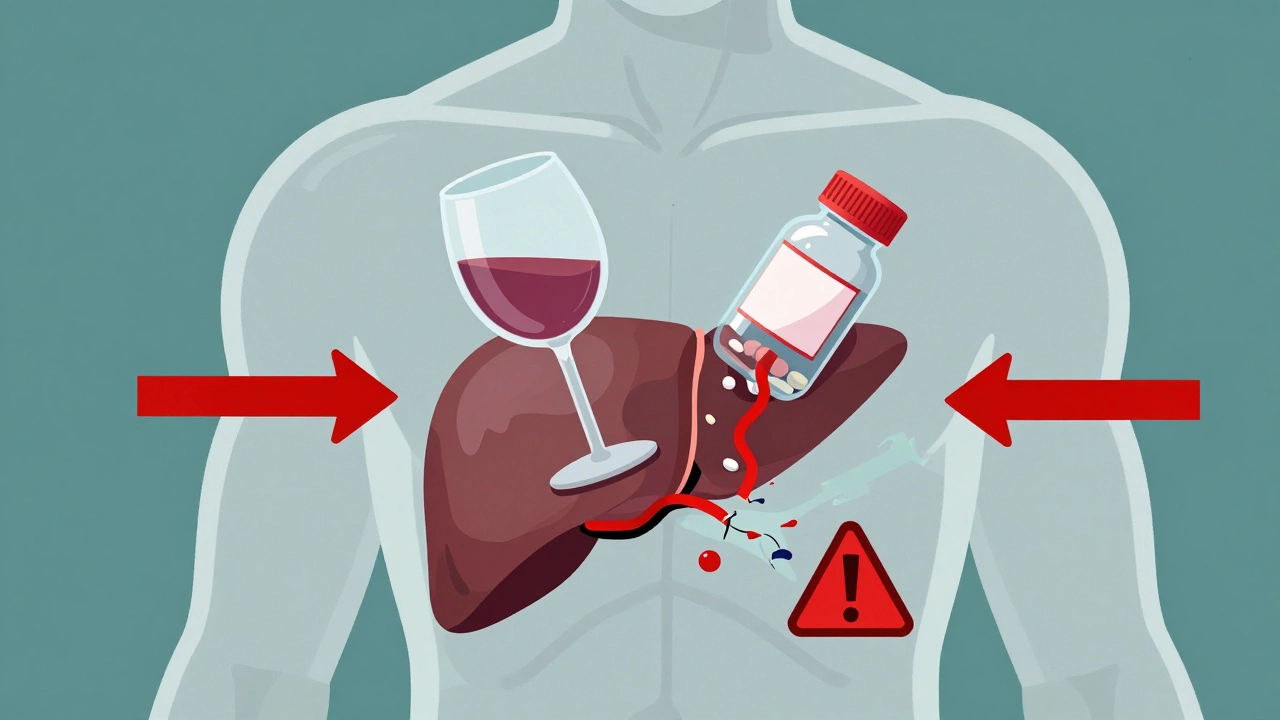
Corticosteroid injections? They offer short-term relief-maybe 4 to 8 weeks-but studies show no real improvement in long-term motion at 12 weeks. They’re not a cure. They’re a pause button. Some doctors still use them for severe pain, but they shouldn’t replace movement.
Manipulation under anesthesia? It sounds dramatic, and it is. Surgeons crack the joint open under sedation to break up tight tissue. But it’s risky-fractures, nerve damage, and re-freezing can happen. Guidelines say wait at least 6 months of conservative therapy first. Only consider it if you’ve tried everything and still can’t lift your arm above 90 degrees.
When to See a Professional
You don’t need to wait until you’re miserable. If you’ve had shoulder stiffness for more than 3 weeks with no trauma, see a physical therapist. Early intervention is the biggest predictor of success. Patients who start therapy within 8 weeks of symptoms report 65% pain reduction at 6 months. Those who wait? Only 32%.
Also, watch for red flags. Fever, night sweats, unexplained weight loss? That’s not frozen shoulder. That’s something else-maybe infection or cancer. Don’t assume. Get checked.
Tools and Support
You don’t need expensive gear. A towel, a broomstick, and a doorway are all you need. But if you want structure, a $25 shoulder rehab kit with a wand and resistance bands helps. Some people use the ShoulderROM device, a new FDA-cleared tool that gives real-time feedback on your range of motion. Clinical trials show it cuts recovery time by 32% compared to standard home exercises.
Online support matters too. The Adhesive Capsulitis Support Group on Facebook has over 12,000 members sharing videos, progress photos, and tips. Seeing someone else go through the same thing makes the journey less lonely.
What’s Next for Frozen Shoulder Treatment?
Research is shifting. The old idea was to rest and wait. Now, we know movement-even in pain-is the best medicine. The American Academy of Family Physicians updated its guidelines in 2023 to recommend early mobilization within pain tolerance. That’s a big change.
Future treatments may be personalized. The NIH is studying IL-6, an inflammatory marker, to predict who responds best to stretching versus injections. Imagine a blood test telling you whether you’ll recover faster with daily pendulums or need a different approach. That’s coming soon.
For now, the path is clear: start early, move gently, stay consistent. Frozen shoulder doesn’t vanish overnight. But with the right strategy, it doesn’t have to rule your life for years either.





15 Comments