Nexium vs. PPI Alternatives Comparison Tool
Quick Takeaways
- Nexium (esomeprazole) is a potent proton pump inhibitor (PPI) used for acid‑related conditions.
- Common PPI alternatives include omeprazole, pantoprazole, lansoprazole and rabeprazole - all work similarly but differ in dose, cost and side‑effect profile.
- H2‑blockers such as famotidine and ranitidine provide a milder acid‑reduction effect and are often cheaper.
- Choosing the right drug depends on condition severity, insurance coverage, price and personal tolerance.
- In New Zealand, most PPIs are prescription‑only, while some lower‑dose versions are available over‑the‑counter.
Whether you’re dealing with frequent heartburn, gastro‑oesophageal reflux disease (GERD) or a stomach ulcer, the medication you pick can shape how quickly you feel better and how many side effects you endure. esomeprazole comparison is a common search because patients often wonder if Nexium is worth the premium price or if a cheaper alternative will do the job.
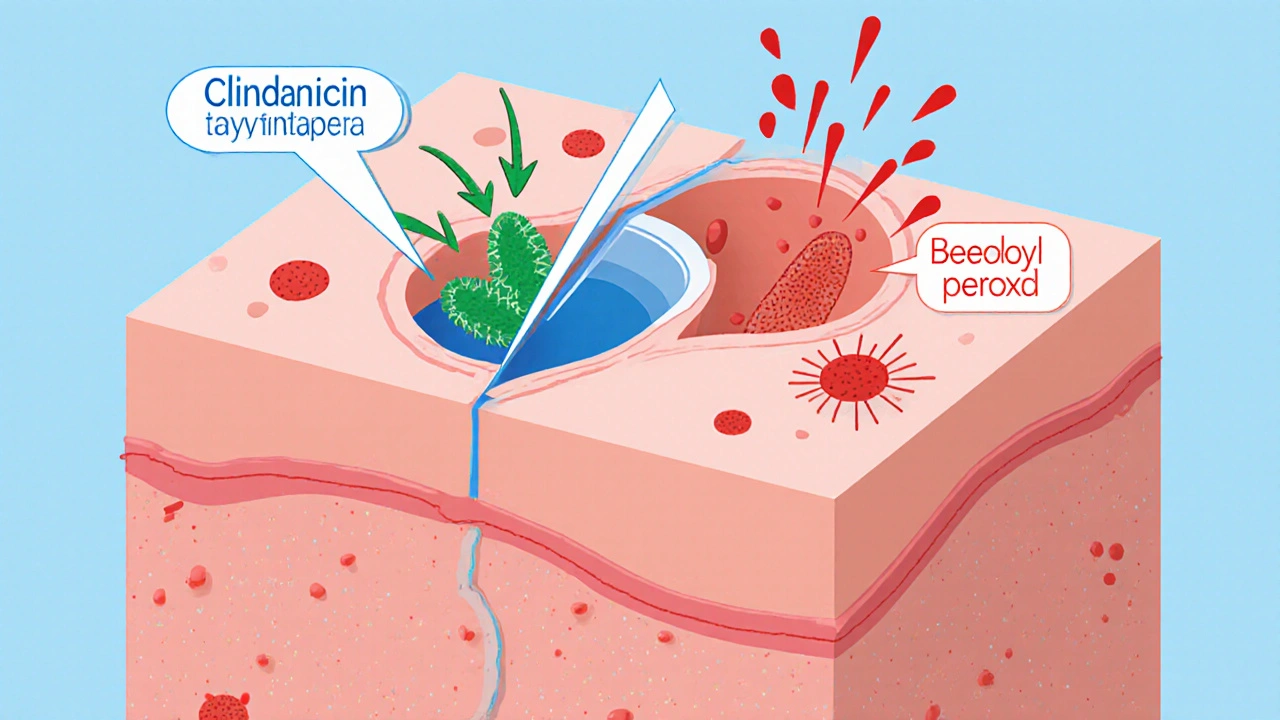
What is Nexium (Esomeprazole)?
Nexium is a brand name for esomeprazole, a proton pump inhibitor (PPI) that reduces stomach acid by blocking the H+/K+ ATPase pump in gastric parietal cells. First approved by the FDA in 2001, the drug is prescribed for GERD, erosive esophagitis, Zollinger‑Ellison syndrome and for protecting the stomach lining when patients take NSAIDs. In New Zealand, esomeprazole is listed on the PHARMAC schedule as a prescription‑only medicine, though a 20mg tablet is available OTC in some pharmacies.
Common Alternatives to Nexium
Below are the most frequently considered substitutes, each a PPI or an H2‑blocker. The first mention of each includes microdata for knowledge‑graph mapping.
Omeprazole is a generic PPI introduced in 1988. It shares the same mechanism as esomeprazole but is typically sold under the brand name Prilosec in the US and as Losec elsewhere.
Pantoprazole is a later‑generation PPI, marketed as Protonix. It is known for a slightly longer half‑life, which can be helpful for night‑time reflux.
Lansoprazole (brand Prevacid) entered the market in 1995 and is often chosen for patients who experience dyspepsia despite other PPIs.
Rabeprazole (brand Aciphex) is praised for a rapid onset of action, making it a good option for acute ulcer pain.
Famotidine belongs to the H2‑blocker class. It works upstream of PPIs by blocking histamine receptors on parietal cells, providing moderate acid suppression.
Ranitidine was a widely used H2‑blocker until 2020, when many formulations were withdrawn over NDMA contamination concerns. Some regions still offer NDMA‑tested versions.
Proton Pump Inhibitors (PPIs) represent a drug class that includes all the agents above except the H2‑blockers. They are the most potent acid‑suppressors available.
H2‑Blockers are a separate class that includes famotidine and ranitidine, typically providing less profound acid reduction but with fewer drug‑interaction concerns.

Side‑by‑Side Comparison
| Brand / Generic | Class | Typical Dose | OTC Availability (NZ) | Year Approved | Common Side Effects | Approx. Cost (NZD) per 30‑day supply |
|---|---|---|---|---|---|---|
| Nexium (esomeprazole) | PPI | 20‑40mg daily | 20mg OTC (limited) | 2001 | Headache, diarrhoea, abdominal pain | ~$30‑$45 |
| Omeprazole | PPI | 20‑40mg daily | OTC 20mg | 1988 | Nausea, flatulence, dizziness | ~$15‑$25 |
| Pantoprazole | PPI | 20‑40mg daily | Prescription only | 2000 | Diarrhoea, headache, rash | ~$20‑$35 |
| Lansoprazole | PPI | 15‑30mg daily | Prescription only | 1995 | Stomach cramps, nausea, dizziness | ~$18‑$30 |
| Rabeprazole | PPI | 20mg daily | Prescription only | 1997 | Upper‑resp tract infection, headache | ~$22‑$38 |
| Famotidine | H2‑Blocker | 20‑40mg daily | OTC 20mg | 1986 | Constipation, fatigue, dizziness | ~$8‑$12 |
| Ranitidine | H2‑Blocker | 150mg twice daily | Limited (NDMA‑tested) | 1981 | Headache, rash, nausea | ~$10‑$15 |
How to Choose the Right Acid‑Reducing Medication
Here’s a simple decision tree you can follow:
- Severity of symptoms: If you have frequent heartburn (≥3‑4 times a week) or diagnosed GERD, a PPI is usually preferred.
- Response to first‑line therapy: Try an OTC omeprazole or famotidine for two weeks. If symptoms persist, step up to prescription‑strength esomeprazole or pantoprazole.
- Cost considerations: Generic PPIs (omeprazole, lansoprazole) are 30‑50% cheaper than brand‑name Nexium.
- Drug‑interaction profile: If you’re on clopidogrel, warfarin or certain antifungals, discuss with your doctor because PPIs can alter metabolism.
- Long‑term safety: For therapy beyond 8 weeks, review risks like vitamin B12 deficiency, magnesium loss, or bone fractures. H2‑blockers often have a milder impact on nutrient absorption.
Safety, Interactions, and Long‑Term Concerns
All PPIs share a core safety record, but subtle differences matter:
- Infection risk: Suppressing acid can let Clostridioides difficile flourish. A 2022 NZ hospital study found a 1.3‑fold increase in C.diff infection after six weeks of PPI use.
- Nutrient absorption: Prolonged use (≥12 months) may lower magnesium, calcium and vitamin B12 levels, contributing to muscle cramps or anemia.
- Kidney disease: Recent cohort data from the Auckland Regional Health Board linked chronic PPI use to a modest rise in chronic kidney disease risk.
- Drug interactions: PPIs inhibit CYP2C19, affecting drugs like clopidogrel, diazepam, and certain HIV protease inhibitors. H2‑blockers have fewer CYP interactions but can affect the absorption of drugs that require an acidic environment (e.g., ketoconazole).
Always tell your pharmacist about every supplement and prescription you’re taking.

Cost and Insurance Landscape in New Zealand
PHARMAC subsidises many generic PPIs, which can drop the out‑of‑pocket price to under $10 for a 30‑day supply. Nexium, being a brand name, often sits outside the subsidy list, meaning you’ll pay the full market price unless your private health fund covers it. When budgeting, consider the following:
- Ask your doctor if a generic version (omeprazole or lansoprazole) will work for your condition.
- Check whether your insurer categorises PPIs as a Tier2 medication-some funds require a co‑pay of $5‑$10.
- For occasional heartburn, an OTC famotidine pack can be as low as $8, making it a sensible first‑line test.
Real‑World Scenarios
Case 1 - Young adult with sporadic heartburn: Jane, 28, tried a few OTC antacids with limited relief. She switched to famotidine 20mg daily, found quick symptom control and saved money.
Case 2 - Middle‑aged man with diagnosed GERD: Mark, 45, was on Nexium 40mg for a year and experienced persistent bloating. His doctor switched him to generic omeprazole 20mg, which controlled reflux equally well and cut his monthly cost by half.
Case 3 - Elderly patient on multiple meds: MrsNg, 73, needed ulcer protection while taking low‑dose aspirin. Her clinician chose pantoprazole because it has fewer drug‑interaction concerns compared with esomeprazole.
Bottom Line
If you need the strongest, most consistent acid suppression, Nexium remains a solid choice, but it’s rarely the only effective option. Generic PPIs usually give the same relief at a lower price, and H2‑blockers can be enough for mild, occasional symptoms. Always weigh severity, cost, and any existing medications before deciding.
Frequently Asked Questions
Can I switch from Nexium to a generic PPI without a doctor’s approval?
Yes, most patients can transition safely, but it’s best to discuss the change with a healthcare professional to ensure the dosage matches your condition and to monitor any symptom recurrence.
How long is it safe to take Nexium continuously?
Short‑term use (up to 8weeks) is generally safe for most adults. For longer courses, a doctor should evaluate risks like nutrient deficiencies and infection susceptibility.
Are there any foods that boost the effectiveness of PPIs?
Taking the medication 30‑60minutes before a meal, especially a breakfast with protein, helps the pill reach the bloodstream when the stomach is most active. Avoid grapefruit, which can interfere with drug metabolism.
What should I do if I miss a dose of Nexium?
Take the missed dose as soon as you remember, unless it’s almost time for the next one. In that case, skip the missed tablet and continue with your regular schedule-don’t double‑dose.
Is it okay to take an H2‑blocker and a PPI together?
Combining them provides little added benefit and can increase side‑effects. Doctors may prescribe an H2‑blocker at night only if a PPI alone isn’t controlling nighttime reflux.





18 Comments