Getting life-saving medication shouldn’t mean choosing between rent and refills. Yet for millions of Americans, high drug prices make that choice daily. Patient Assistance Programs from drug companies offer free or low-cost prescriptions to those who qualify-but knowing who qualifies isn’t simple. These programs aren’t one-size-fits-all. They’re complex, inconsistent, and often confusing. If you’re struggling to afford your meds, here’s what you actually need to know to get help.
Who Can Apply for Patient Assistance Programs?
The most universal rule across all major programs is income. Nearly every drug company sets eligibility based on your household income as a percentage of the Federal Poverty Level (FPL). For 2023, 500% of the FPL means $75,000 a year for a single person and $153,000 for a family of four. But here’s the catch: not all programs use the same number. Pfizer’s RxPathways program, for example, uses different thresholds depending on the drug. For common prescriptions like Eucrisa, you must earn less than 300% FPL ($43,200 for one person). For cancer drugs like Keytruda, the cutoff jumps to 500-600% FPL ($64,800-$77,760). GSK’s Patient Assistance Foundation sets a hard cap: $58,650 for a single person, $120,570 for a family of four. If your income is even $100 over, you’re automatically disqualified-even if you’re paying $2,000 a month out of pocket.Insurance Status Matters More Than You Think
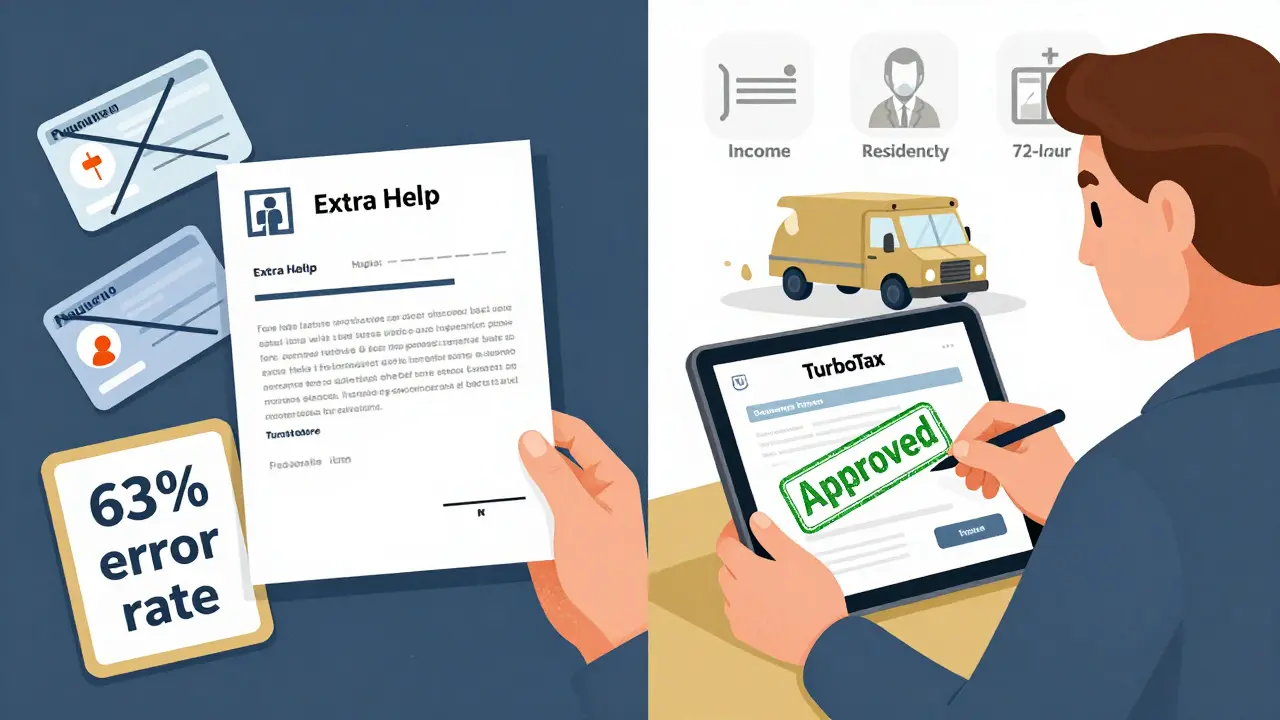
This is where most people get tripped up. Contrary to what you might assume, being uninsured doesn’t automatically make you eligible. In fact, 97% of independent charity PAPs won’t help you if you have no insurance at all. But here’s the twist: most manufacturer programs require you to be uninsured or underinsured. Pfizer’s Patient Assistance Program explicitly says: “You must be uninsured or on government assistance.” If you have commercial insurance-even if your deductible is $10,000-you’re typically ineligible. Merck is an exception. They allow insured patients to apply only if they can prove “special financial and medical hardship.” But even then, if your insurance plan tells you to apply for manufacturer help first, you’re out of luck. That’s because CMS rules forbid manufacturers from stepping in when insurers are supposed to cover the cost. Medicare beneficiaries face an even trickier landscape. If you’re on Medicare Part D and earn below 150% FPL ($20,385 for one person), you’re supposed to qualify for Extra Help. But if you applied and got denied? Takeda’s Help At Hand program will consider you-but only if you submit that denial letter. If you didn’t apply for Extra Help first? Your PAP application gets rejected.What You Need to Prove: Documents That Actually Work
It’s not enough to say you’re low-income. You have to prove it. Every program requires documentation-and it’s not always what you expect. Most require:- Completed application forms signed by both you and your doctor
- Proof of income: W-2s, recent pay stubs, or your last tax return
- Proof of U.S. residency: utility bill, lease, or driver’s license
- Proof of treatment by a U.S.-licensed doctor
Medicare Part D and the Hidden Trap
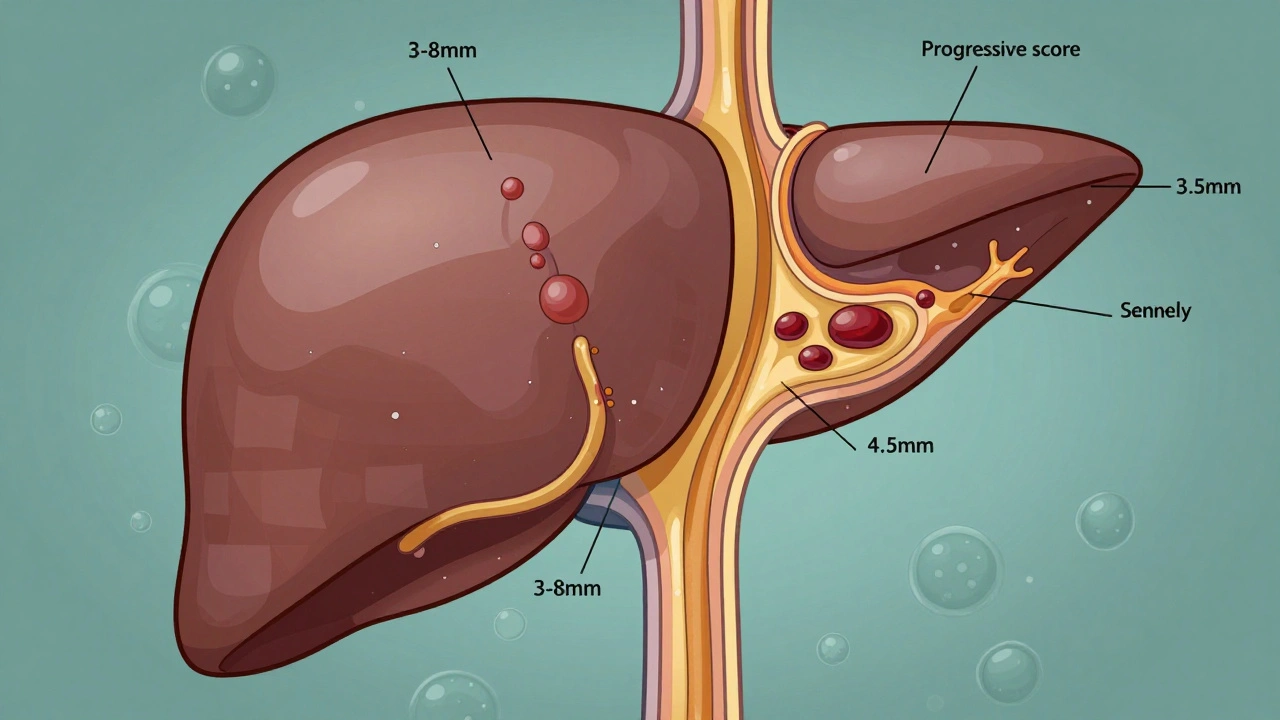
If you’re on Medicare, you’re caught in a system designed to keep you from getting help. Here’s how it works: PAPs are supposed to operate “outside the Part D benefit.” That means the value of your free drugs doesn’t count toward your True Out-of-Pocket (TrOOP) costs. You still need to pay $8,000 out of pocket in 2024 to hit catastrophic coverage. That’s why some beneficiaries with income between 135-150% FPL are stuck. They earn too much for Extra Help but too little to afford their co-pays. They don’t qualify for manufacturer PAPs because they have Medicare. And they can’t use charity PAPs because they’re insured. This is called the “Medicare Part D gap”-and it’s real. The Medicare Rights Center found 58% of rejections were due to insurance status alone.What Drugs Are Covered? Not All Are Equal
PAPs don’t cover every medication. They focus on high-cost, brand-name drugs-especially in oncology, autoimmune diseases, and rare conditions. IQVIA found 98% of branded cancer drugs have PAP support. For heart medications? Only 76% do. The average annual cost of a drug covered by a PAP is $1,157. For non-covered drugs? Just $367. That tells you who these programs are really for: patients on expensive specialty meds. If you’re on a generic blood pressure pill, don’t expect help. Even if you’re struggling, your drug might not be eligible.How Long Does It Take? And What Happens After Approval?
Once you submit your application, don’t expect instant results. The average processing time is 14.7 days. But if your paperwork is incomplete? You’ll get a denial letter-and a 37% chance you’ll need to reapply. The Medicare Rights Center found 42% of applicants needed three or more tries to qualify. Once approved, you won’t get a check. You’ll get a prescription card or a shipment of pills directly from the pharmacy. Most people get their meds within 72 hours. But you’re not done. You’ll need to re-verify eligibility every 3-12 months, depending on the drug. GSK requires annual re-enrollment. Pfizer asks for updates every quarter for specialty meds.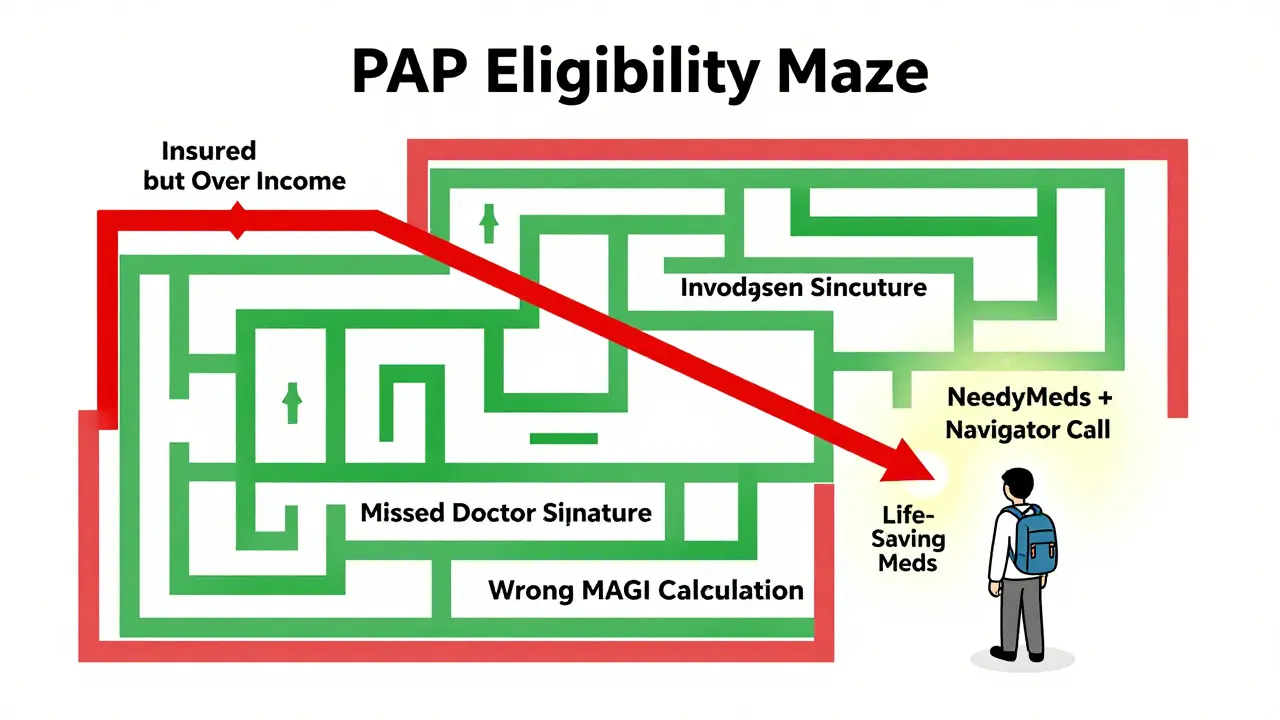
Where to Start: Real Tips That Work
If you’re overwhelmed, here’s what actually helps:- Find your drug’s manufacturer website. Search “[Drug Name] patient assistance.”
- Use the Medicine Assistance Tool (MAT) from NeedyMeds-it pulls data from 100+ programs.
- Call the PAP navigator. 78% of programs have one. Wait times are 11 minutes on average, but 18 minutes for Medicare patients.
- Don’t skip the doctor’s signature. Merck reports 28-day delays if the form isn’t signed.
- Double-check household size and MAGI. These are the top two reasons for denial.
Why This System Is Broken-and What’s Changing
Critics say PAPs let drug companies avoid lowering prices. Harvard’s Dr. Aaron Kesselheim calls them “a band-aid on a broken system.” In 2022, pharmaceutical companies spent $32.7 billion on these programs-more than most hospitals spend on charity care. Yet drug prices keep rising. But change is coming. Starting in 2025, Medicare Part D will cap out-of-pocket costs at $2,000 a year. That could reduce PAP use by 35-40% among seniors. By 2026, Medicare will start negotiating prices for 10 high-cost drugs. That could shrink the need for PAPs by 15-20%. Still, 27.5 million Americans are underinsured. They have coverage-but not enough to afford their meds. For them, PAPs remain essential. The real fix? Lower drug prices. Until then, these programs are the only lifeline for millions.What If You’re Denied?
Denials happen. Don’t give up. Most are due to paperwork errors, not income. Review your denial letter. Did you miss a signature? Did you use gross income instead of MAGI? Call the PAP and ask for a second review. Many will reopen your case if you fix the mistake. You can also turn to independent charities like the PAN Foundation or HealthWell Foundation. They have stricter income limits (usually 500% FPL) but may help even if you have insurance. They don’t cover every drug-but they cover more than you think.Can I get help if I have Medicare?
Yes, but only under specific conditions. If you’re on Medicare Part D and earn below 150% of the Federal Poverty Level, you should first apply for Extra Help. If denied, you can then apply for manufacturer PAPs like Takeda’s Help At Hand. If you have commercial insurance alongside Medicare, most PAPs won’t help you. Check each program’s rules carefully.
Do I need to be uninsured to qualify?
Not always. Most manufacturer programs require you to be uninsured or on government assistance. But some, like Merck’s, allow insured patients to apply if they prove financial hardship. Independent charities like PAN Foundation may help even if you have insurance, as long as your out-of-pocket costs are high.
What if my income is just above the limit?
You won’t qualify for most programs. But some manufacturers offer tiered assistance. For example, Pfizer’s oncology programs extend to 600% FPL. Also, some charities offer sliding-scale copay assistance-even if you’re slightly over the income limit. Call and ask. Don’t assume you’re ineligible.
How often do I need to reapply?
It depends on the drug. For primary care medications, you usually reapply once a year. For specialty or cancer drugs, you may need to re-verify every 3 months. GSK requires annual re-enrollment. Pfizer asks for quarterly updates for high-cost meds. Always mark your calendar-missing a deadline means losing your meds.
Can I apply for multiple programs at once?
Yes. If you take multiple high-cost drugs, apply to each manufacturer’s program. You can also combine manufacturer PAPs with independent charities like PAN or HealthWell. Just make sure you’re not violating any program rules-some don’t allow stacking assistance.
What if I can’t get my doctor to sign the form?
This is a common roadblock. Doctors are busy. Call the PAP’s help line-they often have templates or fax forms directly to your provider’s office. Some programs even offer nurse navigators who can help coordinate with your clinic. Don’t wait until the last minute-start this process early.





15 Comments