Imagine you’re trying to copy a secret recipe-not by reading the ingredient list, but by tasting the dish and guessing what’s in it. That’s what generic drug makers face when trying to replicate complex medications like inhaled asthma treatments, topical creams for eczema, or long-acting injectables. These aren’t your ordinary pills. They’re complex generic formulations, and proving they work just like the brand-name version is one of the toughest challenges in modern medicine.
What Makes a Generic Drug ‘Complex’?
Not all generics are created equal. Simple generics-like a generic version of ibuprofen-are easy to copy. The active ingredient is a single chemical, the tablet dissolves predictably, and blood levels tell you everything you need to know. But complex generics? They’re different. The FDA defines them as products where the way the drug is delivered, formulated, or packaged makes it hard to prove it works the same way as the original. These include:- Liposomes and nanoparticles that trap drugs inside tiny fat bubbles
- Inhalers that spray medicine deep into the lungs
- Topical gels and creams that need to penetrate skin layers
- Extended-release injectables that slowly release drug over weeks
- Drug-device combos like auto-injectors or nasal sprays
Why Blood Tests Don’t Work for Complex Drugs
For most drugs, bioequivalence is proven by measuring how much of the drug enters the bloodstream and how fast. The standard? The 90% confidence interval for AUC and Cmax must fall between 80% and 125% of the brand-name drug. Simple. Clean. Proven. But what if the drug isn’t meant to enter the bloodstream at all? Take a corticosteroid cream for eczema. Its job is to sit on the skin and reduce inflammation-not to get absorbed into the blood. Measuring blood levels tells you nothing about whether the cream is working where it’s supposed to. Same with an inhaler: the goal is for the drug to land in the lungs, not show up in your plasma. But current regulations still demand blood tests. That’s like trying to prove a paintbrush works by measuring how much paint ends up in your coffee cup. That’s why regulators and scientists are stuck. Traditional bioequivalence methods were built for systemic drugs. They don’t fit complex, locally acting products. And without a way to measure drug delivery at the site of action, manufacturers are forced to guess.The Reverse-Engineering Nightmare
Generic manufacturers don’t get the original formula. They don’t know the exact ratios of excipients, the manufacturing temperature, the mixing speed, or how the drug was crystallized. They only have the final product. So they reverse-engineer it. They break it down, analyze it, test it, and try to rebuild it. It’s like trying to rebuild a car from the exhaust fumes. One study found that developing a complex generic takes 2.5 to 3 times longer than a simple one. And more than 70% of applications fail at the bioequivalence stage. Even small differences matter. A change in the type of emulsifier in a cream. A 1-micron shift in particle size in an inhaler. A different drying process for a lyophilized injectable. These aren’t just technical tweaks-they can change how the drug performs. One manufacturer told regulators that switching from one stabilizer to another caused the drug to clump, reducing lung deposition by 40%.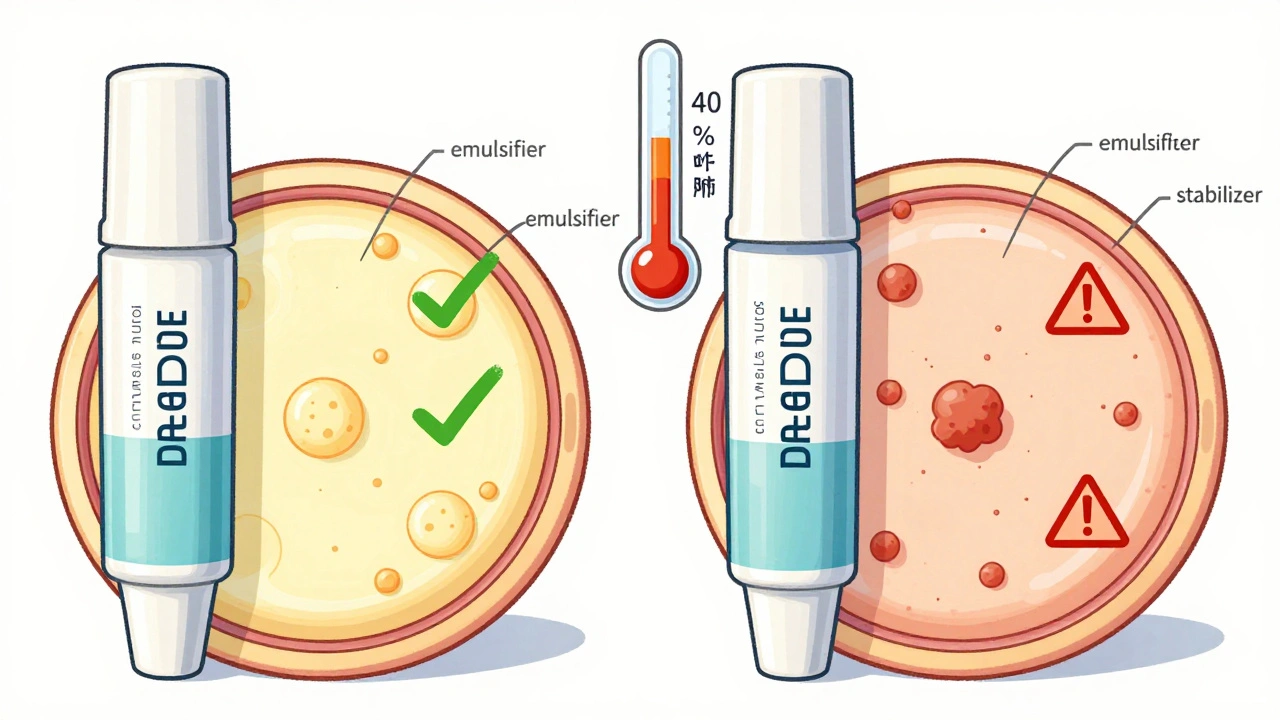
Regulatory Chaos Around the World
The FDA has guidelines. The European Medicines Agency has others. The World Health Organization has its own. And none of them fully agree on how to prove bioequivalence for complex products. For example, the FDA might accept an in vitro test showing that a topical product releases drug at the same rate as the brand. The EMA might demand a clinical endpoint study-like measuring skin redness over weeks. That means a company has to run two separate development programs just to get approval in both markets. It’s expensive. It’s slow. And it’s why so few complex generics ever make it to market. A 2020 survey found that 89% of generic manufacturers said bioequivalence testing was their biggest hurdle. Stability was close behind-76% said it was a nightmare. And 68% couldn’t even agree on how to characterize their own products.What’s Changing? New Tools and New Thinking
The good news? The FDA is trying to fix this. They’ve created the Complex Generic Drug Products Committee. They’ve published 15 new guidance documents since 2022 for products like inhaled budesonide, testosterone gels, and topical corticosteroids. They’re pushing for Quality by Design (QbD)-a strategy where manufacturers build stability and performance into the product from day one. Instead of testing after the fact, they plan for it: choosing excipients that won’t degrade, mapping out how environmental changes affect the product, running compatibility tests early. They’re also investing in new tools:- Imaging tech that shows exactly how deep a cream penetrates skin
- Models that simulate how particles deposit in the lungs
- Physiologically-based pharmacokinetic (PBPK) modeling, which can predict drug behavior without human trials

The Bigger Picture: Cost, Access, and Innovation
There are about 400 complex brand-name drugs on the U.S. market with no generic alternatives. That’s a $120 billion opportunity. These are often high-cost specialty drugs-used for cancer, autoimmune diseases, chronic respiratory conditions. Patients pay hundreds or thousands of dollars a month. Generics could slash those costs. But the path is narrow. Only 10-15% of complex generic applications get approved, compared to over 80% for simple ones. Development costs can hit $50 million per product. And the timeline? 18 to 24 months longer than a traditional generic. Still, the market is moving. Complex generic sales are projected to grow from $15 billion in 2023 to $45 billion by 2028. That’s a 24.6% annual growth rate. Why? Because patients, insurers, and governments are demanding cheaper alternatives. And because science is catching up.What’s Next?
The future of complex generics isn’t about making better pills. It’s about building better tools to measure what matters. Standardized methods for particle size. Validated in vitro models for skin and lung delivery. Global regulatory alignment through ICH guidelines-especially the Q3D standard for elemental impurities, expected in late 2024. The biggest barrier isn’t science. It’s mindset. We’ve spent decades measuring blood levels. Now we need to learn how to measure delivery-where the drug actually works. For manufacturers, it means investing in advanced analytics. For regulators, it means being flexible. For patients, it means hope-hope that one day, a life-changing drug won’t cost a fortune just because it’s hard to copy.FAQ
Why can’t we just use blood tests for complex generics like we do for regular ones?
Blood tests only work if the drug needs to enter the bloodstream. For products like inhalers, topical creams, or eye drops, the drug is meant to act locally-on the skin, lungs, or eyes. Measuring blood levels tells you nothing about whether the drug reached its target. That’s why regulators are turning to new methods like imaging, in vitro models, and computer simulations to assess delivery at the site of action.
How long does it take to develop a complex generic compared to a regular one?
Developing a complex generic takes 18 to 24 months longer than a traditional generic-often 3 to 4 years total. The development cost is also 2.5 to 3 times higher. More than 70% of complex generic applications fail at the bioequivalence stage, mostly because manufacturers can’t prove the product behaves the same way as the brand-name version under real-world conditions.
What’s the biggest challenge for generic manufacturers?
The biggest challenge is reverse-engineering a product without knowing its formula. Manufacturers have to figure out the exact particle size, excipient ratios, manufacturing process, and stability profile just by analyzing the final product. Even minor changes-like a different mixing speed or drying temperature-can ruin bioequivalence. This turns drug development into a high-stakes puzzle with no instruction manual.
Why are regulatory requirements different between the FDA and EMA?
Regulatory agencies have different historical approaches and scientific priorities. The FDA may accept an in vitro test showing drug release matches the brand. The EMA might require a full clinical trial proving the same symptom improvement. This lack of global alignment forces manufacturers to run duplicate studies, increasing costs and delaying access. Harmonization efforts through ICH are underway but still in progress.
Are there any new technologies helping with bioequivalence testing?
Yes. New tools like advanced imaging (to track skin penetration), in vitro lung deposition models, and physiologically-based pharmacokinetic (PBPK) modeling are being adopted. PBPK modeling, in particular, can predict how a drug behaves in the body using computer simulations, reducing the need for human trials. The FDA has funded research into these tools and published guidance on their use for products like inhalers and topical creams.
Why aren’t there more complex generics on the market?
Because the scientific, regulatory, and financial barriers are so high. Only 10-15% of complex generic applications get approved, compared to over 80% for simple generics. Development costs can exceed $50 million, and failure rates are above 70%. With so many risks and so little certainty, many manufacturers avoid these products-even though the market demand is huge.








14 Comments