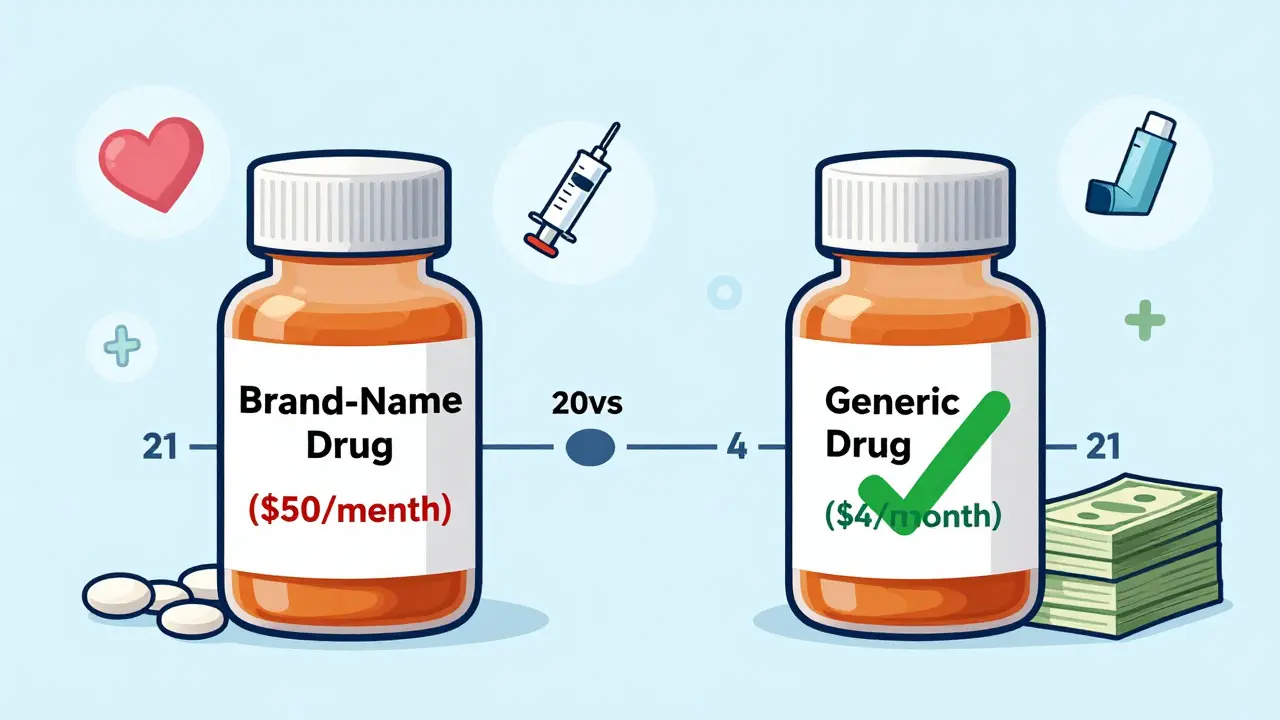
For millions of people managing chronic conditions like high blood pressure, diabetes, or asthma, the real cost isn’t just the price of the pill-it’s the price of skipping it. A $50 monthly brand-name drug might seem manageable until you realize you’re paying that every month, for life. But what if you could cut that bill by 80%-without losing effectiveness? That’s the power of generic medications.
What Exactly Are Generic Drugs?
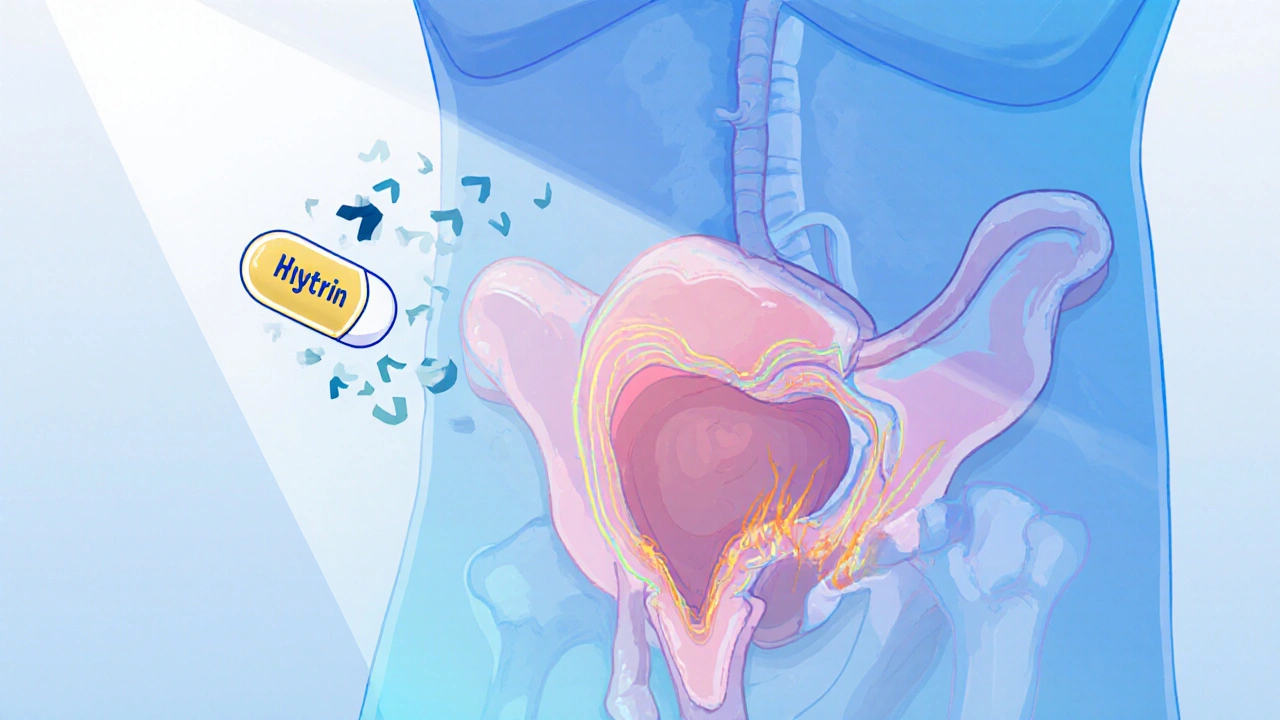
Generic drugs are exact copies of brand-name medications, down to the active ingredient. They work the same way, in the same dose, and deliver the same results. The FDA requires them to meet the same strict standards for strength, purity, and performance as the original. The only differences? The shape, color, or inactive ingredients like fillers-and the price.Take lisinopril, a common blood pressure medication. The brand version, Prinivil, costs about $40 to $50 a month. The generic? Around $4. Same drug. Same effect. Same safety profile. But the savings? Over $1,200 a year. For someone on this medication for 20 years, that’s more than $24,000 saved. And that’s just one drug.
Why Generics Are So Much Cheaper
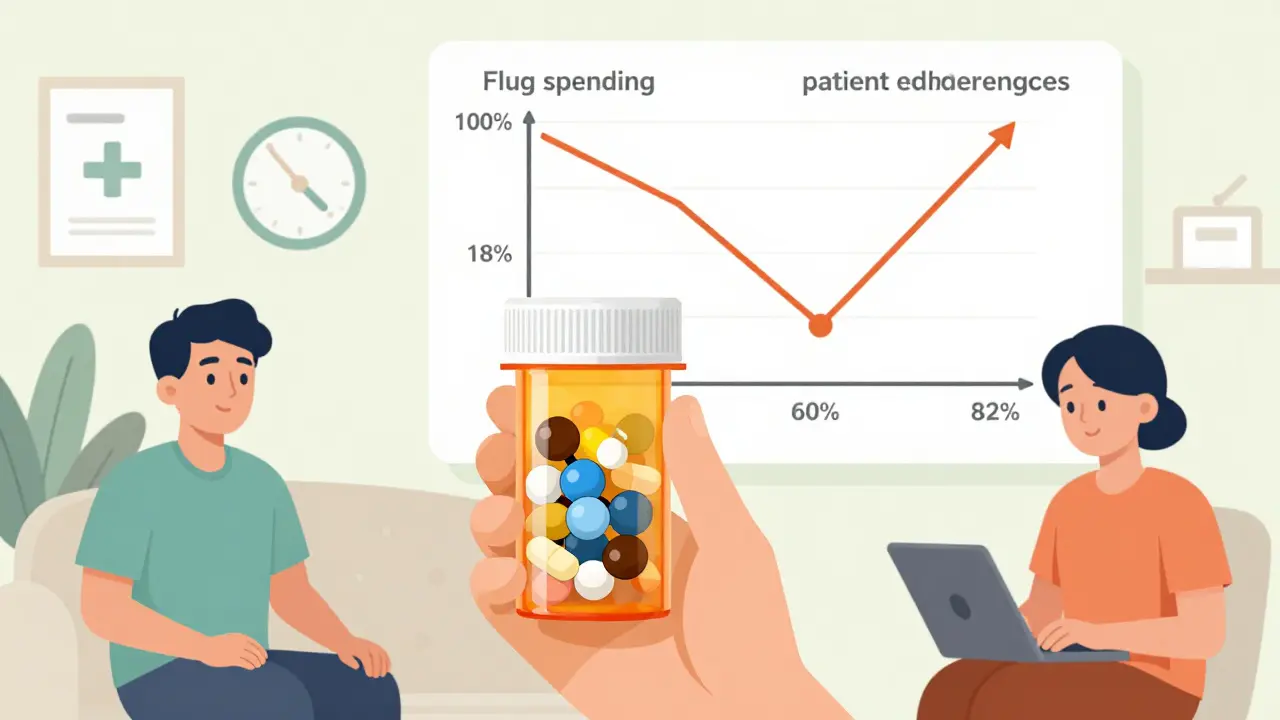
Brand-name drug companies spend years and billions developing a new medication. They need to recoup those costs, so they set high prices during their patent protection-usually 20 years. Once that patent expires, other manufacturers can produce the same drug without repeating the expensive research. They don’t need to run massive clinical trials because the original drug’s safety and effectiveness are already proven.The result? Competition. Dozens of companies can now make the same generic. That drives prices down fast. In the U.S., 97% of prescriptions filled are generics-when they’re available. But here’s the kicker: even though generics make up nearly all prescriptions, they account for only 18% of total drug spending. That’s how massive the savings are.
Real Savings for Real People
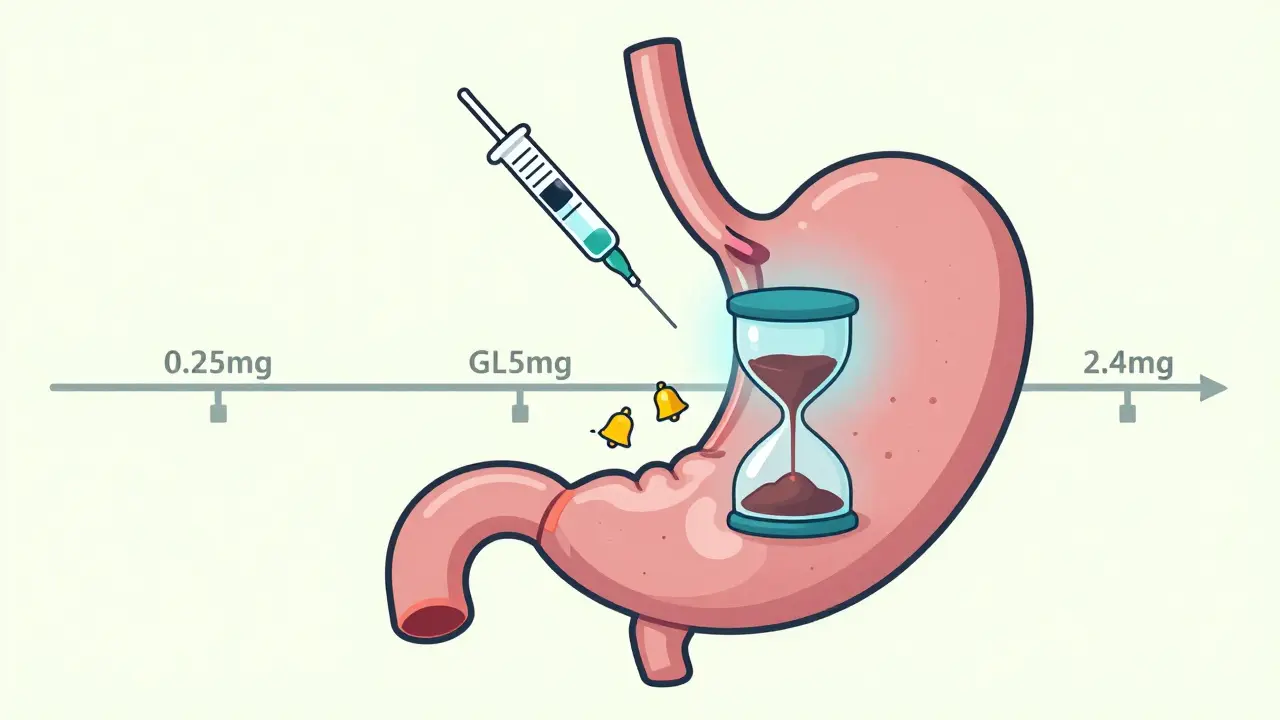
Let’s look at three common chronic conditions and what switching to generics can do:- Diabetes (Metformin): Brand-name Glucophage costs $150/month. Generic metformin? $10-$25. That’s $1,500-$1,800 saved per year.
- Asthma (Fluticasone): Flonase brand costs $60/month. Generic fluticasone propionate? $15. Annual savings: $540.
- High Cholesterol (Atorvastatin): Lipitor brand is $120/month. Generic atorvastatin? $5-$10. Annual savings: $1,300-$1,400.
For someone managing all three conditions, switching to generics could save over $3,000 a year. Over a 30-year span? More than $90,000. That’s not just money-it’s security. It means being able to afford groceries, pay rent, or take a vacation without choosing between meds and meals.
Does It Really Work the Same?
A lot of people worry: “If it’s cheaper, is it weaker?” The answer is no. The FDA requires generics to be bioequivalent-meaning they deliver the same amount of active ingredient into the bloodstream at the same rate as the brand. The acceptable range? Within 80% to 125% of the brand’s performance. That’s not a loophole-it’s a scientifically proven margin of safety.Studies show no difference in outcomes between brand and generic for conditions like heart disease, depression, or epilepsy. In fact, patients on generics are 18-22% more likely to stick with their medication because they can actually afford it. And adherence is everything. Skipping doses because of cost leads to hospitalizations, emergency visits, and worse outcomes. One study found that patients who took their generics consistently had 20-30% fewer hospital stays.
Why Don’t More People Use Them?
Misinformation. That’s the biggest barrier.Some patients believe generics are “inferior” because they look different. Others think the brand must be better because it’s more expensive. Pharmacists report that up to 40% of patients refuse generics at first-until they’re shown the data. Educational programs that explain FDA requirements increase patient acceptance by 45%.
Another issue? Insurance. Some plans still push brand-name drugs first, even when generics exist. Or they charge higher copays for generics than they should. That’s changing, though. The 2022 Inflation Reduction Act capped insulin at $35/month for Medicare patients-and many of those are generics. More states are now requiring insurers to cover generics at the lowest possible cost.
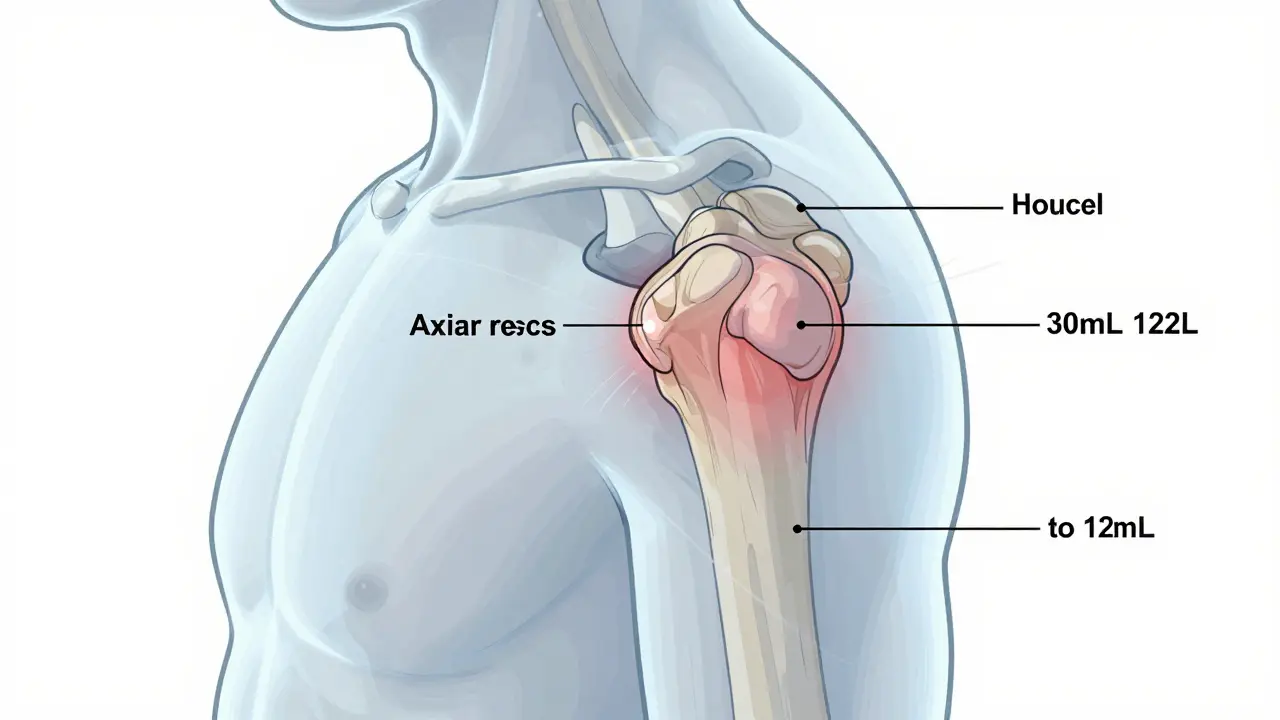
What About Complex Conditions?
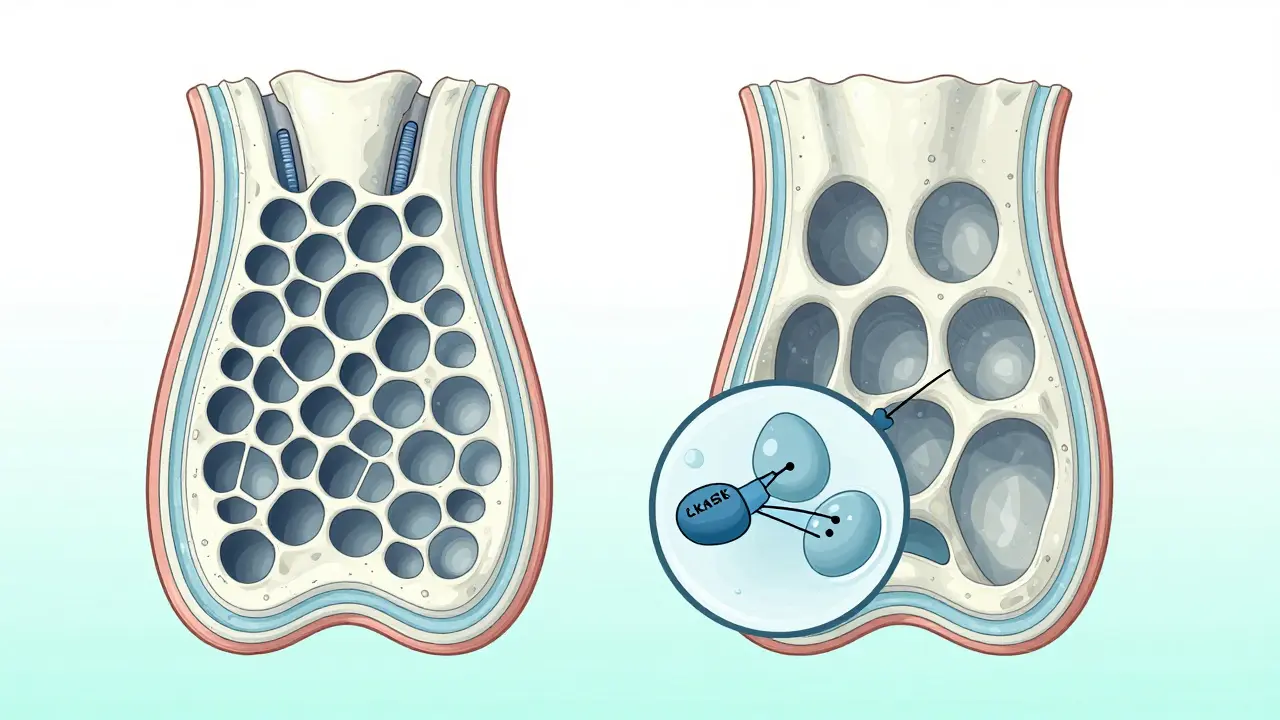
Some people think generics only work for simple conditions. That’s outdated. Today, generics exist for complex treatments like HIV, rheumatoid arthritis, and even some cancer drugs. In India, generic HIV medications increased treatment access by 40% and cut death rates by 25% between 2005 and 2015. Brazil’s national program for generic diabetes and hypertension drugs saved $1.2 billion in annual healthcare costs.Even biologics-complex, injectable drugs once thought too hard to copy-are now seeing biosimilars, which are generic-like versions. These are already saving the U.S. healthcare system billions, and that number is expected to hit $300 billion over the next decade.
How to Start Saving Today
You don’t need to wait for a policy change. Here’s how to get started:- Ask your doctor: “Is there a generic version of this drug?”
- Call your pharmacy and ask: “What’s the cash price for the generic?” Sometimes it’s cheaper than your insurance copay.
- Use the FDA’s Orange Book online to check if a generic is approved for your drug.
- Ask your pharmacist about Medication Therapy Management (MTM) programs. These are free for Medicare Part D patients and help you find cheaper alternatives.
- Check manufacturer patient assistance programs. Even brand-name companies offer discounts if you qualify.
Don’t assume your prescription can’t be switched. Many doctors assume patients know about generics-but they don’t. Be the one to ask.
The Bigger Picture
Between 2010 and 2020, U.S. use of generics saved $2.4 trillion in total drug spending. That’s not abstract. That’s real people keeping their homes, paying for childcare, and avoiding bankruptcy because they could afford their meds.By 2027, another $150 billion in brand-name drugs will lose patent protection. That means even more generics hitting the market. The trend is clear: generics aren’t just a cost-cutting trick-they’re the backbone of sustainable, long-term healthcare.
If you’re managing a chronic condition, your medication isn’t a luxury. It’s a lifeline. And you shouldn’t have to choose between your health and your finances. Generics make that choice unnecessary.
Are generic drugs as safe as brand-name drugs?
Yes. The FDA requires generics to have the same active ingredients, strength, dosage form, and route of administration as the brand-name drug. They must also meet the same strict manufacturing standards. Bioequivalence testing ensures they work the same way in your body. Thousands of studies confirm no difference in safety or effectiveness.
Why do generics look different from brand-name drugs?
By law, generics can’t look exactly like the brand-name version to avoid trademark infringement. That means different colors, shapes, or markings. But these are only inactive ingredients-like dyes or fillers-and they don’t affect how the drug works. The active ingredient is identical.
Can I switch from a brand to a generic anytime?
Almost always. Your doctor can prescribe the generic version directly, or your pharmacist can substitute it unless the prescription says “Dispense as Written.” Always check with your provider if you’re unsure, especially for narrow-therapeutic-index drugs like warfarin or thyroid meds-but even then, generics are usually safe and approved.
Why does my insurance sometimes make me pay more for the generic?
Some plans have outdated formularies or require prior authorization. Others charge higher copays for generics if they’re not on the lowest tier. Call your insurer and ask why. You can often appeal or switch plans during open enrollment. Many states now require insurers to cover generics at the lowest possible cost.
Are there any downsides to using generics?
The only real downsides are availability (some generics aren’t made yet) and rare reactions to inactive ingredients-like a dye or preservative. If you have allergies or sensitivities, talk to your pharmacist. But for the vast majority of people, there’s no downside. The savings are real, and the effectiveness is proven.
How do I know if a generic is approved for my drug?
Check the FDA’s Orange Book online. It lists all approved generic drugs and their brand-name equivalents. You can search by drug name or active ingredient. Your pharmacist can also look this up for you in seconds.
Do generics work for mental health conditions?
Yes. Generic versions of antidepressants like sertraline, fluoxetine, and citalopram are widely used and proven effective. Studies show no difference in symptom relief between brand and generic SSRIs. The key is consistency-taking the medication daily. Generics make that possible for people on fixed incomes.
Will switching to a generic affect my future health?
It’s likely to improve it. When people can afford their meds, they take them. Better adherence means fewer complications-fewer heart attacks, strokes, kidney failure, and hospitalizations. The long-term health benefit of generics isn’t just financial-it’s lifesaving.


8 Comments