When your monthly medication bill feels like a second rent payment, you’re not alone. Nearly 29% of Americans say they struggle to afford their prescriptions. But here’s the truth: you don’t have to pay full price just because your doctor wrote a script. There’s a proven, safe, and often overlooked way to cut those costs without losing effectiveness-therapeutic alternative medication.
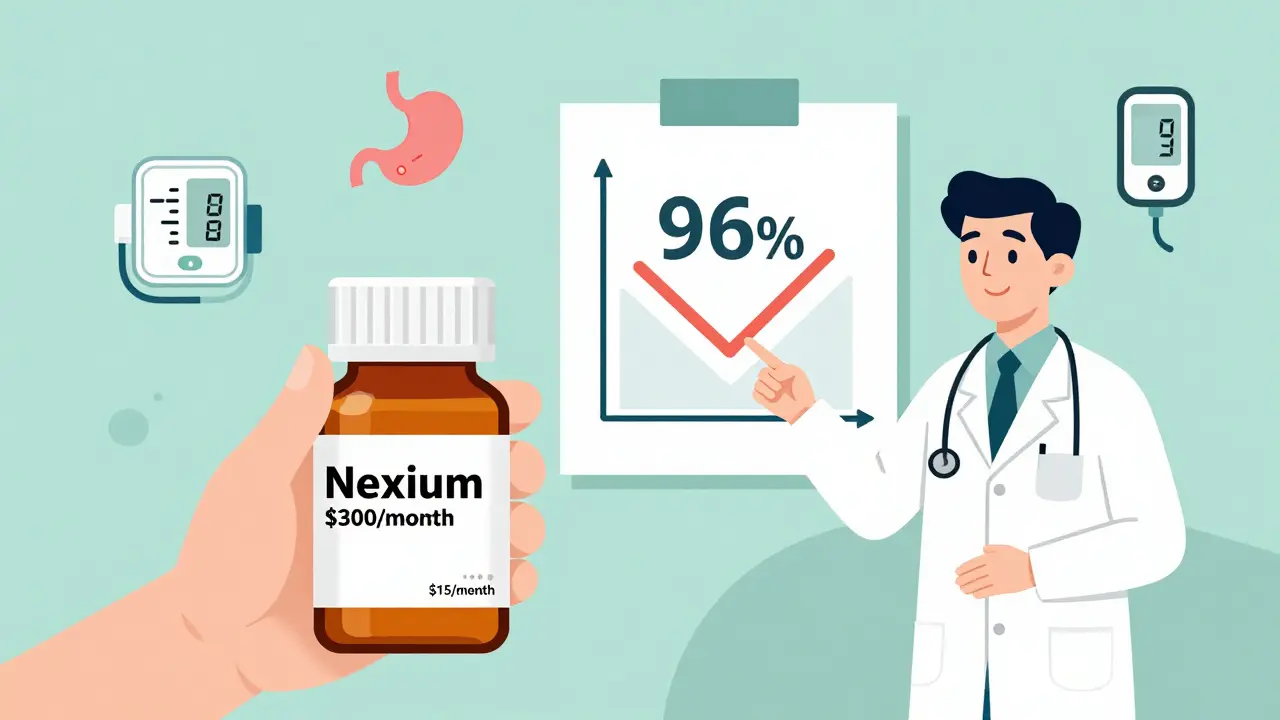
Therapeutic interchange isn’t about switching to a generic version of the same drug. It’s about swapping your current medication for a different one that works just as well-only cheaper. For example, switching from brand-name esomeprazole (Nexium) to generic omeprazole can drop your annual cost from $365 to just $15. That’s not a typo. It’s a 96% savings. And this isn’t rare. It happens every day in clinics across the country.
What Is a Therapeutic Alternative?
A therapeutic alternative is a different drug that treats the same condition with similar effectiveness and safety. It’s not the same chemical compound, but it does the same job. For high blood pressure, lisinopril and benazepril are both ACE inhibitors. For acid reflux, famotidine and omeprazole both reduce stomach acid. For depression, sertraline and escitalopram are both SSRIs. These aren’t random swaps. They’re backed by clinical studies, FDA guidelines, and decades of real-world use.
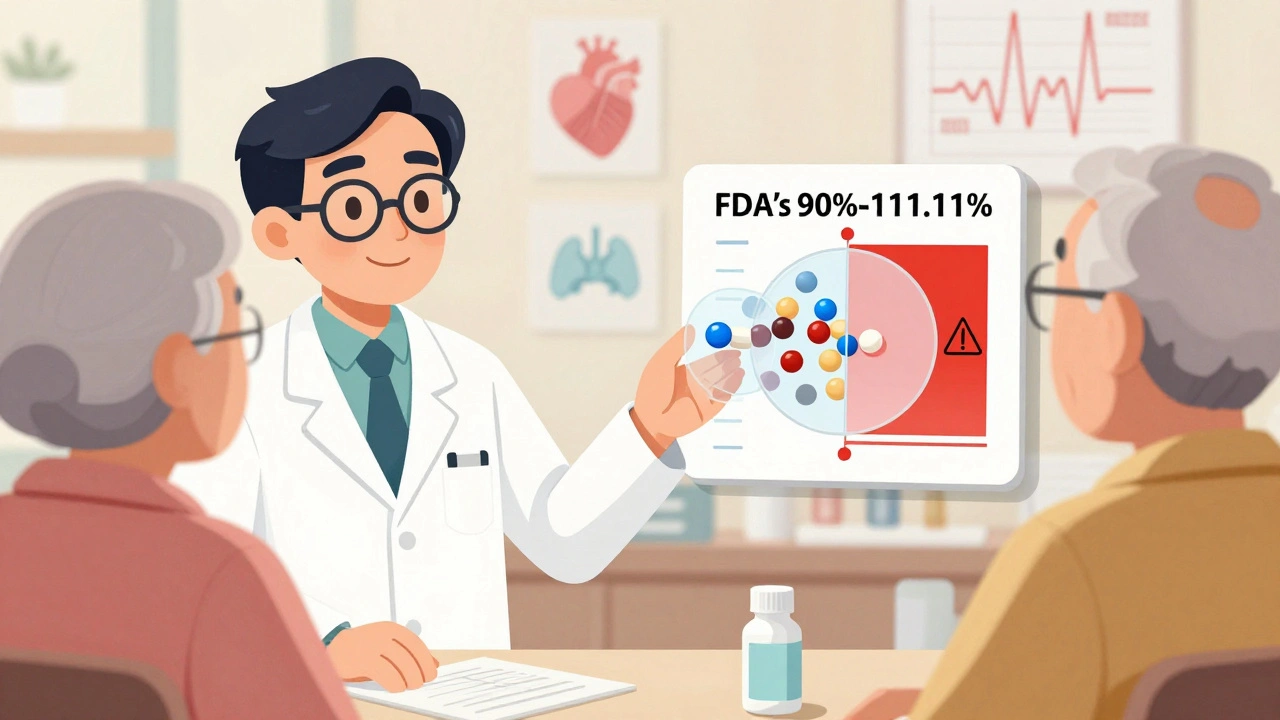
Unlike generic substitution-where you get the exact same drug at a lower price-therapeutic interchange opens up more options. Sometimes, the brand-name drug you’re on doesn’t even have a generic version. But there might be another drug in the same class that does. That’s where the savings kick in.
According to a 2023 study from the American Academy of Family Physicians, 78% of primary care doctors regularly use therapeutic interchange when cost is an issue. And patients who make the switch save an average of $47 per month. That’s over $500 a year. For chronic conditions like diabetes, heart disease, or arthritis, those savings add up fast.
When It Works (and When It Doesn’t)
Therapeutic alternatives work best for common, long-term conditions: high blood pressure, high cholesterol, acid reflux, depression, type 2 diabetes, and asthma. These are conditions where multiple drugs have been proven equally effective in head-to-head trials. For example, switching from brand-name Crestor (rosuvastatin) to generic atorvastatin can save $380 a month. From Eliquis to warfarin? Up to $450 monthly.
But it’s not magic. It doesn’t work for everything. In cancer, rare autoimmune diseases, or complex neurological conditions, there often aren’t interchangeable options. About 15% of specialty drug classes have no viable alternatives. And even in common conditions, some people respond differently. One patient might switch from Jardiance to metformin and see their blood sugar soar. Another might feel great. That’s why this isn’t a DIY swap. You need your doctor’s input.
A 2024 case in JAMA showed what happens when the swap goes wrong: a patient switched from Taltz (a biologic for psoriasis) to methotrexate. Their condition flared up, leading to $18,000 in emergency care. That’s why you don’t just ask for a cheaper drug-you ask for the right cheaper drug.
How to Ask for a Therapeutic Alternative
Asking your doctor for a cheaper option sounds scary. But it’s not. Doctors want you to take your meds. They just don’t always know what you’re paying. Here’s how to do it right:
- Start with cost: Say, “I’m having trouble affording my medication. Is there another option that works just as well but costs less?” That’s it. No jargon. No pressure. Just honesty.
- Do your homework: Use GoodRx or your pharmacy’s $4 list (Walmart, CVS, Walgreens all have them). Look up your drug and see what alternatives are on the list. For example, if you’re on gabapentin, check if pregabalin is cheaper. If you’re on metformin, see if other diabetes drugs are priced lower.
- Bring the data: Print or show your doctor the prices. “I saw that omeprazole 20mg is $15 a month here, but esomeprazole is $300. Can we switch?” You’re not challenging them-you’re helping them help you.
- Ask for specifics: Don’t just say “something cheaper.” Say, “Could I try lisinopril instead of benazepril?” or “Is there a generic version of this that’s been proven just as effective?”
Doctors are more likely to agree if you come prepared. A 2023 survey found that 68% of patients who asked with specific alternatives got their request approved. Those who just said, “It’s too expensive,” were turned down more often.

What to Do If Your Doctor Says No
Some doctors hesitate because they’re not familiar with alternatives. Others worry about side effects or efficacy. Here’s how to respond:
- Ask why: “What’s your concern about switching?” Sometimes, it’s just habit. They’ve always prescribed the brand. You can say, “I understand, but I found studies showing these two work the same. Can we try it for a month?”
- Use trusted sources: Point them to the Agency for Healthcare Research and Quality or the Institute for Clinical Systems Improvement. They have free, evidence-based guidelines for therapeutic interchange in 125 conditions.
- Request a trial: “Can we try the alternative for 30 days? If it doesn’t work, we switch back.” Most doctors will agree to that.
- Ask for a tiering exception: If you’re on Medicare Part D, your plan may cover your current drug at a higher tier. You can request an exception. The law says they must respond within 72 hours for urgent cases or 14 days otherwise.
One patient on Reddit switched from Lyrica (pregabalin) to generic gabapentin after showing her neurologist a study. The doctor was hesitant at first-then agreed. Her monthly cost dropped from $450 to $15. She’s been on it for a year. No side effects. No loss of pain control.
Other Ways to Cut Costs Alongside a Therapeutic Swap
Therapeutic interchange is powerful, but it’s not the only tool. Combine it with these strategies:
- 90-day prescriptions: Many insurers charge the same copay for a 90-day supply as they do for 30 days. That’s a 25% savings per refill. Ask if your drug can be dispensed in 90-day amounts.
- Manufacturer coupons: If your drug is brand-name, check the manufacturer’s website. Most offer copay cards that can reduce your cost to $0 for 12 months. Examples: Novo Nordisk for Ozempic, Eli Lilly for Mounjaro.
- Patient assistance programs: Programs like NeedyMeds, RxAssist, and the HealthWell Foundation help low-income patients get free or low-cost meds. Eligibility is often up to 400% of the federal poverty level ($60,000/year for an individual in 2024).
- Compare pharmacy prices: A 2023 GoodRx study found prices can vary by 5,000% between pharmacies for the same drug. Use GoodRx or SingleCare to find the lowest price near you-even for brand-name drugs.
One patient saved $720 a year by switching from brand-name Xarelto to warfarin, getting a 90-day supply, and using a GoodRx coupon. That’s not luck. That’s strategy.
What’s Changing in 2025
Therapeutic interchange is getting easier. In January 2025, the American Medical Association updated its guidelines to include 17 new drug classes, including GLP-1 agonists for diabetes and weight loss. Electronic health records from Epic and Cerner now auto-suggest alternatives at the point of prescribing. One hospital system saw a 15.3% increase in therapeutic swaps after adding the tool.
Medicare Part D now requires all plans to use standardized criteria for therapeutic interchange. That means fewer denials. And the Inflation Reduction Act is slowly lowering prices for top-tier drugs, which could reduce the need for swaps in some cases.
But experts agree: even with price negotiation, therapeutic interchange will still save billions. Oliver Wyman estimates the U.S. could save $127 billion a year if every eligible patient switched to a cost-effective alternative.
Real Stories, Real Savings
Here’s what real people have done:
- Carol, 68: Switched from Eliquis to warfarin. Saved $450/month. Took a blood test every 4 weeks. No clots. No hospital visits.
- Mark, 52: Switched from brand-name Crestor to generic atorvastatin. Saved $380/month. Cholesterol stayed under control.
- Janet, 41: Switched from Otezla (for psoriasis) to methotrexate. Saved $600/month. Had a mild flare-up at first-her doctor adjusted the dose. Now she’s stable.
And the failures? They’re rare-but real. One man switched from a biologic for Crohn’s to an older drug. His symptoms returned. He ended up in the ER. That’s why you never switch alone. Always with your doctor’s guidance.
Final Thoughts: You Have Power
Prescription drug prices in the U.S. are 2.5 times higher than in other developed countries. That’s not your fault. But you don’t have to accept it. Therapeutic alternatives are a legal, safe, and proven way to take back control.
You don’t need to be an expert. You don’t need to argue. You just need to ask. And if your doctor says no, ask again-with data. You’re not asking for a favor. You’re asking for care that fits your life.
Medication shouldn’t be a luxury. It should be accessible. And with the right swap, it can be.




11 Comments