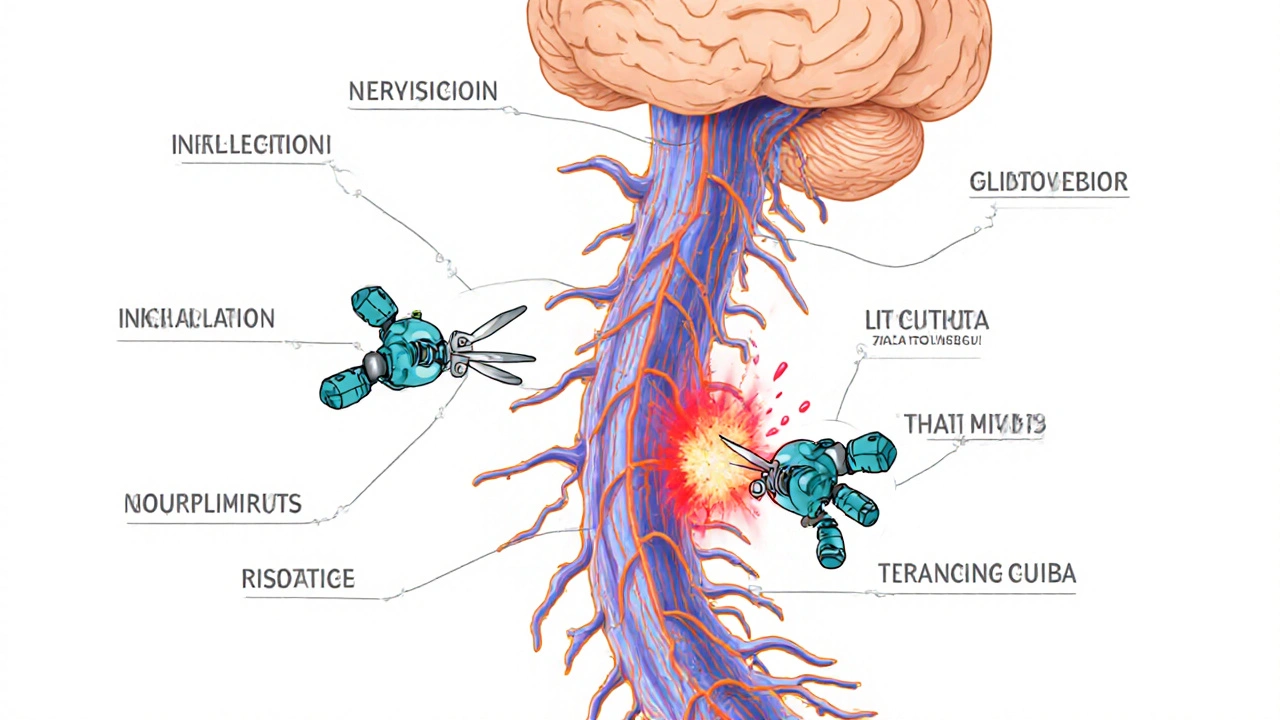
Multiple sclerosis, or MS, isn't just one disease-it's a complex breakdown in how your nervous system communicates with the rest of your body. At its core, MS is an autoimmune disease, meaning your own immune system turns against you. Instead of protecting your nerves, it attacks the protective coating around them called myelin. This coating is what lets electrical signals zoom through your brain and spinal cord at speeds up to 120 meters per second. When myelin gets damaged, those signals slow down, get scrambled, or stop altogether. The result? Symptoms that can range from mild fatigue to loss of movement, vision problems, or trouble thinking clearly.
How MS Actually Works in the Body
Imagine your nerves as electrical wires. Myelin is the rubber insulation wrapped around them. In MS, immune cells-mostly T-cells-cross the blood-brain barrier and start chewing through that insulation. This isn’t random damage. It’s targeted. The immune system mistakes myelin for a foreign invader, triggering inflammation. Over time, the damaged areas harden into scar tissue, called plaques or lesions. These show up clearly on MRI scans, especially when using gadolinium contrast, which highlights active inflammation.
What makes MS tricky is that the damage doesn’t happen all at once. Lesions appear in different spots across the brain and spinal cord-sometimes causing numbness in your hand, then later trouble walking. The McDonald Criteria, used by neurologists worldwide since 2017, require proof of damage in at least two different areas of the central nervous system and evidence that the damage happened at different times. That’s why diagnosis often takes months. You might have one episode of blurred vision, then a year later, tingling in your legs. Only when both show up on MRI does a diagnosis become certain.
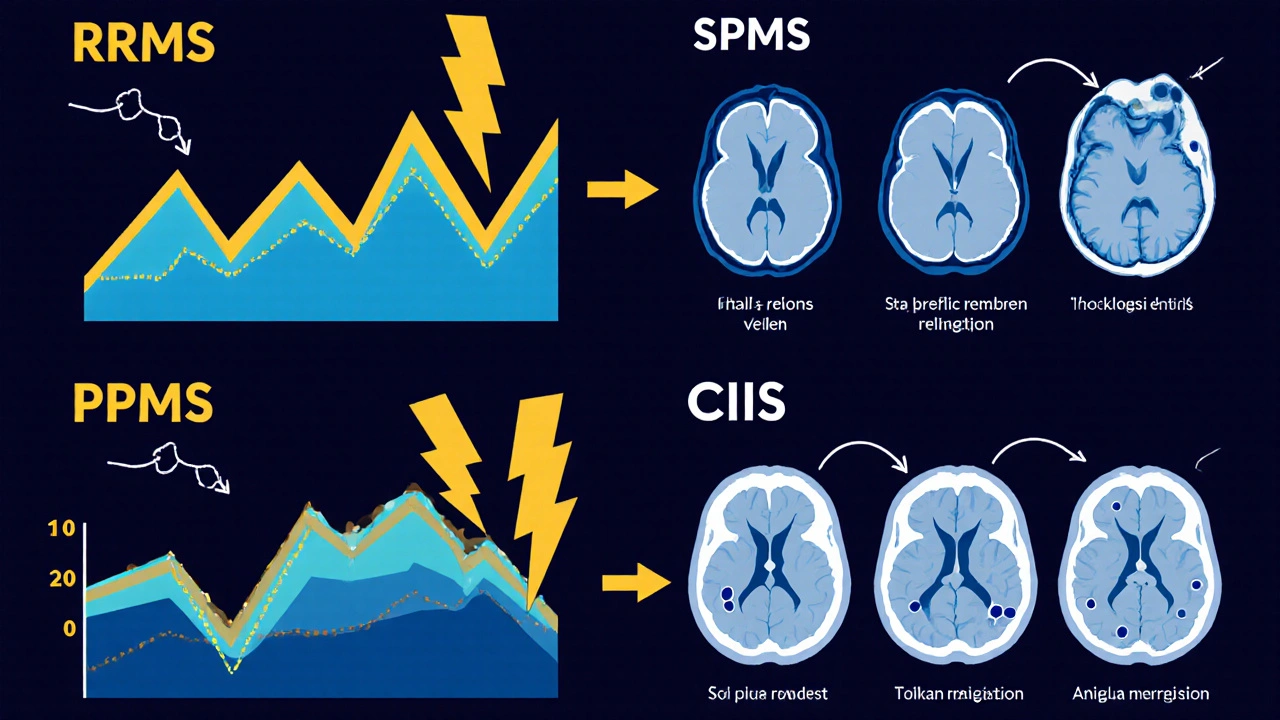
The Four Types of MS
Not everyone with MS follows the same path. There are four main types, and knowing which one you have helps guide treatment.
- Clinically Isolated Syndrome (CIS): This is often the first sign-a single neurological episode, like optic neuritis or sudden weakness, lasting at least 24 hours. About 60-80% of people with CIS who have MS-like lesions on MRI will go on to develop full MS within 10 years.
- Relapsing-Remitting MS (RRMS): This is the most common form, affecting 85% of people at diagnosis. You get clear flare-ups-called relapses-followed by periods where symptoms fade or disappear. Without treatment, people typically have 0.5 to 1 relapse per year.
- Secondary Progressive MS (SPMS): After living with RRMS for years, about half of people start to see steady worsening, even without obvious relapses. This shift usually happens 10 to 25 years after diagnosis. The body can’t repair the damage fast enough anymore.
- Primary Progressive MS (PPMS): This form affects 15% of people and looks different from the start. There are no clear relapses. Instead, symptoms slowly get worse from day one. Progression is measured on the Expanded Disability Status Scale (EDSS), with most people losing about 1-1.5 points per year.
Understanding which type you have isn’t just academic-it changes your treatment plan. For example, many drugs that work for RRMS don’t help much with PPMS.
Who Gets MS-and Why?
MS isn’t something you catch like a cold. It doesn’t spread from person to person. But certain factors make it more likely to develop.
Women are diagnosed 2 to 3 times more often than men. Most people are diagnosed between ages 20 and 40. Geography matters too. If you live near the equator, your risk is low-about 30 per 100,000 people. But if you live in Canada, Scotland, or Scandinavia, that number jumps to 300 per 100,000. Sunlight exposure and vitamin D levels play a big role. Studies show people in regions with less than 300 hours of sunshine per year have a 40% higher risk of MS.
Genetics also contribute. Over 230 gene variants are linked to MS risk. The strongest is HLA-DRB1*15:01, which triples your chance of developing the disease. But having the gene doesn’t mean you’ll get MS. It’s the combination with environment that triggers it.
One of the most surprising links is with the Epstein-Barr virus (EBV), which causes mononucleosis. Research from Harvard found people who’ve had mono have a 32-fold higher risk of MS. But not everyone who gets EBV develops MS-so something else must be involved. Some experts think it’s not the virus itself, but how your immune system responds to it years later.
What Symptoms Do People Really Experience?
MS symptoms vary wildly. Two people with the same diagnosis can feel completely different.
According to data from MyMSTeam, a community of over 150,000 people with MS, 78% say fatigue is their worst symptom. It’s not just being tired after a long day. It’s a crushing exhaustion that makes getting out of bed feel impossible. One user described it as "having your bones filled with lead."
Another common issue is "brain fog." On Reddit’s r/MS community, thousands of posts describe struggling to find words, forgetting names, or losing track of conversations. One user wrote: "I know what I want to say, but my brain just won’t let me say it." This isn’t memory loss-it’s slowed processing speed.
Other frequent symptoms include:
- Numbness or tingling in limbs
- Muscle stiffness or spasms
- Blurred or double vision
- Balance problems and dizziness
- Bladder or bowel control issues
- Depression and anxiety
Many people don’t realize how much MS affects mental health. The uncertainty, the fatigue, the isolation-it adds up. Depression is twice as common in MS patients compared to the general population.
How Is MS Diagnosed?
There’s no single blood test for MS. Diagnosis is a puzzle made of three pieces: medical history, neurological exam, and imaging.
Doctors start by ruling out other conditions-like Lyme disease, vitamin B12 deficiency, or lupus-that can mimic MS. Then comes the MRI. A 3 Tesla scanner is now standard because it finds 30% more lesions than older 1.5 Tesla machines. Gadolinium contrast helps spot active inflammation. Spinal fluid analysis may show abnormal antibodies, and evoked potential tests measure how fast signals travel along nerves.
The whole process often takes 6 to 12 months and involves 3 to 5 specialist visits. In the U.S., the out-of-pocket cost for initial testing can run between $2,500 and $5,000. That’s why many people delay diagnosis, especially without good insurance.
Treatment Options Today
There’s no cure for MS-but there are over 20 disease-modifying therapies (DMTs) that can slow progression, reduce relapses, and improve quality of life.
These drugs fall into six categories:
- Injectables: Like interferon beta and glatiramer acetate. These are older, cheaper options, but many people stop using them because of side effects-flu-like symptoms, injection site pain, or redness. One survey found 42% quit within a year.
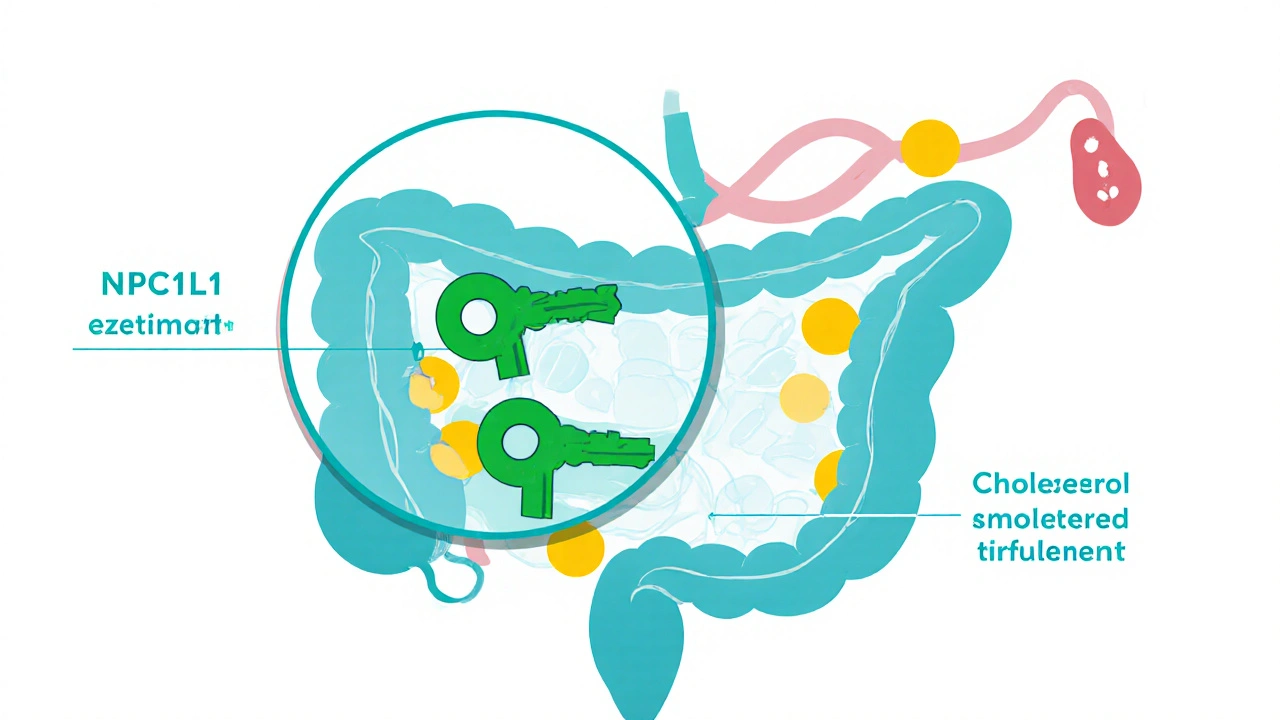
- Oral pills: Such as fingolimod, dimethyl fumarate, and teriflunomide. Easier to take, but come with risks like liver damage or increased infection.
- Infusions: Like ocrelizumab (Ocrevus) and ublituximab (Briumvi). Given every few months in a clinic. These are highly effective, especially for RRMS and PPMS. In trials, ocrelizumab cut relapses by 50% compared to older drugs.
Annual costs range from $65,000 for generic glatiramer acetate to $87,000 for newer drugs like ofatumumab. But 90% of U.S. patients get help through manufacturer copay programs. In countries without such support, access is a huge problem. The Multiple Sclerosis International Federation reports that half of low- and middle-income countries have no access to any DMTs.
Rehabilitation is just as important as medication. Physical therapy focused on balance reduces falls by 47%. Occupational therapy helps with daily tasks. Speech therapy can address "brain fog" and swallowing issues. Most people need 2-3 sessions per week for 8-12 weeks, with copays around $35 per visit under Medicare.
What’s on the Horizon?
Research is moving fast. Scientists are no longer just trying to stop damage-they’re trying to repair it.
One of the most exciting areas is remyelination. Drugs like opicinumab are being tested to help the body regrow myelin. In Phase II trials, it improved visual signal speed by 15%. Another promising drug, ANV419, a selective estrogen receptor beta agonist, reduced new brain lesions by 40% in 24 weeks.
Stem cell therapy is also being explored. As of early 2024, there were 127 active clinical trials worldwide. Some patients with aggressive MS have seen dramatic improvement after resetting their immune system with their own stem cells.
Even the gut microbiome is getting attention. Early trials using fecal transplants showed a 30% drop in inflammatory markers. The idea? Maybe changing gut bacteria can calm the immune system.
And then there’s the bad science. The "liberation procedure," which claimed MS was caused by blocked neck veins, was thoroughly debunked in 2022 after 10 randomized trials showed no benefit. Don’t fall for quick fixes.
Life With MS Today
The good news? Life expectancy for people with MS is now nearly normal. A 2023 Swedish registry found that 70% of people diagnosed after 2010 are still walking without assistance 20 years later. That’s up from just 45% for those diagnosed before 1990. Early treatment makes all the difference.
Workplace accommodations are crucial. Eighty-two percent of employed people with MS need adjustments. Flexible hours and remote work are the top requests. Many companies now offer these as standard.
MS isn’t a death sentence. It’s a chronic condition-one that requires ongoing management, but doesn’t have to define your life. With the right care, support, and treatment, many people continue working, traveling, raising families, and living full lives.
What Should You Do If You Suspect MS?
If you’ve had unexplained neurological symptoms-like sudden vision loss, numbness, or extreme fatigue that doesn’t improve-see a neurologist. Don’t wait. Early diagnosis means early treatment, which can change the course of the disease.
Keep a symptom journal. Note when things happen, how long they last, and what makes them better or worse. Bring it to your appointment. It helps doctors spot patterns.
And remember: you’re not alone. Communities like MyMSTeam and r/MS are full of people who get it. Sharing experiences can be as healing as any medication.
Is multiple sclerosis hereditary?
MS isn’t directly inherited like eye color, but genetics play a role. If a parent has MS, your risk is about 2-5%, compared to 0.1% in the general population. Over 230 gene variants increase susceptibility, with HLA-DRB1*15:01 being the strongest. But having these genes doesn’t mean you’ll get MS-you need the right environmental triggers too.
Can MS be cured?
There’s no cure yet, but treatments can dramatically slow progression. Disease-modifying therapies reduce relapses by up to 50% and delay disability. New research on remyelination and stem cells offers real hope for future repair, not just symptom control.
Do all people with MS end up in a wheelchair?
No. Most people with MS never need a wheelchair. In fact, 70% of those diagnosed after 2010 are still walking independently 20 years later. Progression varies widely. Early treatment, physical therapy, and healthy lifestyle choices make a huge difference.
Is MS more common in certain countries?
Yes. MS prevalence increases with distance from the equator. Rates are highest in Canada, Scotland, and Scandinavia (up to 300 per 100,000), and lowest near the equator (around 30 per 100,000). This is linked to sunlight exposure and vitamin D levels. People in northern latitudes have a much higher risk.
Can diet or supplements help with MS?
No diet cures MS, but some evidence suggests vitamin D, omega-3s, and a low-sodium, plant-rich diet may help reduce inflammation and fatigue. Vitamin D deficiency is a known risk factor, so maintaining levels above 30 ng/mL is recommended. Always talk to your doctor before starting supplements, especially if you’re on DMTs.
How does stress affect MS?
Stress doesn’t cause MS, but it can trigger relapses. Studies show that major life stressors-like job loss or divorce-are linked to a higher risk of flare-ups in the following weeks. Managing stress through mindfulness, therapy, or exercise can help reduce this risk. Mental health support is part of comprehensive MS care.






20 Comments