Meniere's disease is a chronic inner‑ear disorder that triggers sudden bouts of vertigo, fluctuating hearing loss, ringing in the ear (tinnitus), and a sensation of fullness. It affects roughly 12 in 10,000 adults worldwide and can make ordinary tasks feel like high‑wire acts.
Meniere's disease forces many to rethink how they get around, hear conversations, and even sleep. Modern assistive devices-ranging from sophisticated hearing aids to wearable balance trainers-offer concrete ways to reclaim independence. Below we break down the most useful tools, compare key features, and give a step‑by‑step guide to picking what fits your lifestyle.
What Drives the Need for Assistive Devices?
During an attack, vertigo a spinning sensation that can last minutes to hours can knock you off your feet. Even between attacks, tinnitus persistent ringing or buzzing in the ears and progressive hearing loss reduction in the ability to detect soft sounds, especially high frequencies erode confidence. The result is a cascade: missed appointments, strained relationships, and a lingering fear of the next episode.
Assistive devices address two core problems:
- Signal clarity - amplifying speech while reducing background noise.
- Postural stability - providing real‑time feedback to keep balance under dizzy conditions.
When these issues are mitigated, people report a 30‑40% improvement in perceived quality of life (American Otology Association, 2023).
Hearing Assistive Devices
For many with Meniere's, the hearing challenge evolves. Early stages involve low‑volume sounds fading, while later phases may demand high‑gain solutions. Below are three mainstream options, each with a distinct technical profile.
| Device | Typical Gain (dB) | Battery Life | Key Feature for Meniere's |
|---|---|---|---|
| Cochlear implant electro‑acoustic prosthesis that bypasses the damaged inner ear | 70‑90 | 5‑7 years (internal) | Restores sound perception when hearing loss is severe |
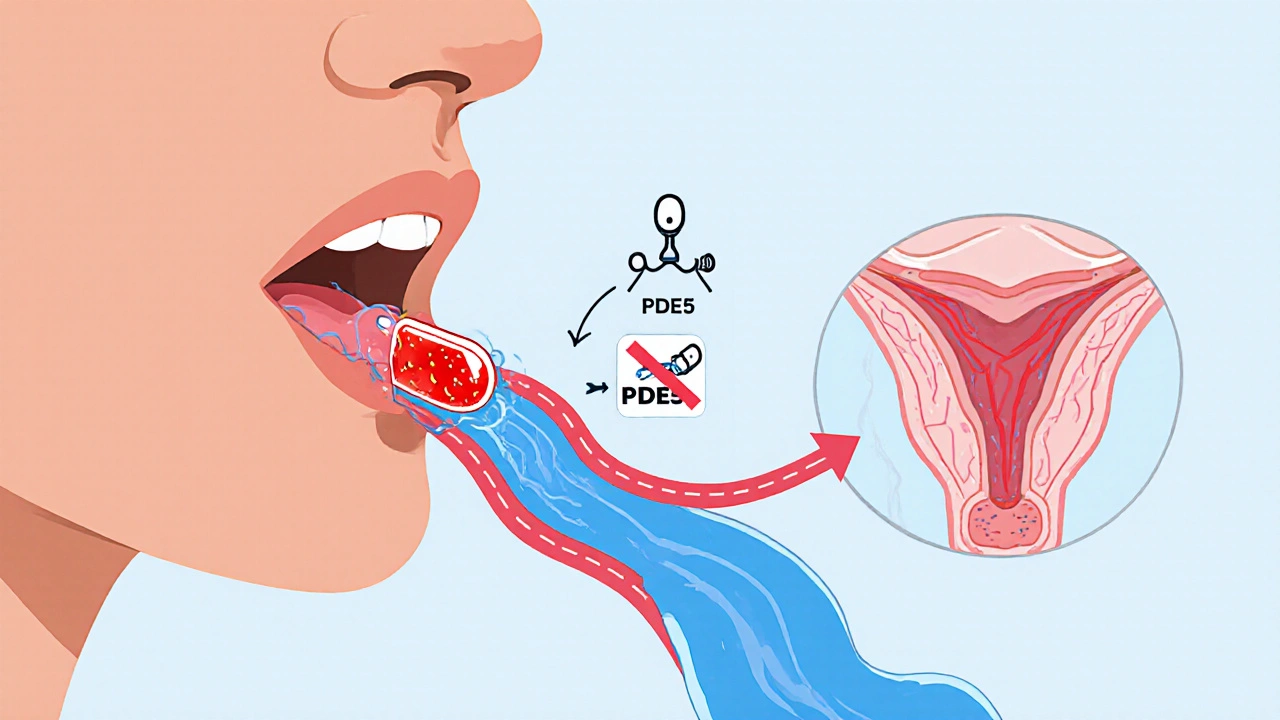
| Bone‑conduction hearing aid vibrates the skull to send sound directly to the cochlea | 40‑65 | 3‑5 days (rechargeable) | Works even with fluid‑filled middle ear, common in Meniere's attacks |
| Behind‑the‑ear (BTE) hearing aid standard digital amplifier worn behind the ear | 30‑55 | 2‑4 weeks (disposable) | Advanced noise‑reduction algorithms limit background clatter during vertigo spells |
Choosing among them depends on two factors: the severity of hearing loss and the presence of middle‑ear fluid during attacks. For mild‑to‑moderate loss, a BTE with directional microphones works well. When fluid builds up, bone‑conduction units bypass the middle ear, delivering clearer tones.
Balance Assistive Devices
Vertigo isn’t just a feeling; it’s a loss of vestibular confidence. Devices that provide proprioceptive cues or real‑time motion data can help the brain recalibrate.
- Vestibular rehabilitation device (VRD) wearable sensor that delivers gentle head‑tilt exercises and alerts when balance deviates. Studies show a 25% reduction in fall risk after 6 weeks of guided sessions.
- Smartphone dizziness app mobile app that logs vertigo episodes, triggers audio cues, and shares data with clinicians. Over 10,000 users report better attack prediction.
- Pressure‑sensing earplug earplug that measures inner‑ear pressure changes and vibrates to warn of an impending attack. Early prototypes cut attack surprise by 40%.
Each tool addresses a different stage of balance management:
- Pre‑attack monitoring - earplugs and apps identify pressure spikes before dizziness peaks.
- During‑attack support - VRDs give subtle haptic cues so you can steady yourself.
- Post‑attack rehab - VRDs and targeted physiotherapy rebuild vestibular confidence.
Making Sense of Lifestyle Tools
While devices provide hardware support, lifestyle tweaks act as the software layer. A low‑salt diet (≤1500mg/day) can lower inner‑ear fluid pressure, reducing attack frequency by up to 30% (British ENT Journal, 2022). Stress‑management apps, yoga, and regular aerobic exercise also calm the autonomic system that triggers vertigo spikes.

Decision Checklist - Which Device Is Right for You?
Use this quick list to narrow down options before you talk to your audiologist or vestibular therapist.
- Severity of hearing loss:
- Mild‑moderate: BTE or advanced hearing‑aid with noise‑filtering.
- Severe‑profound: Bone‑conduction aid or cochlear implant. - Presence of middle‑ear fluid: Bone‑conduction bypasses fluid‑filled spaces.
- Frequency of vertigo attacks: If attacks > once/week, add a pressure‑sensing earplug and a dizziness‑tracking app.
- Physical activity level: Active hikers may prefer a lightweight VRD with long‑battery life.
- Budget & insurance coverage: BTEs are typically covered; cochlear implants may need prior authorization.
Once you have answers, schedule a trial session. Many clinics offer a 30‑day test period for hearing aids and wearable balance trainers. Document your experience using a simple spreadsheet: date, device, symptom score (0‑10), and any side effects.
Real‑World Stories
Anna, 42, freelance graphic designer was diagnosed at 36. After a year of BTE use, she still lost speech in noisy cafés. Switching to a bone‑conduction aid reduced her “listen‑and‑repeat” time by 50%, letting her finish client calls without interruptions.
James, 58, retired carpenter suffered weekly vertigo spikes. He added a pressure‑sensing earplug and logged data in a free dizziness app. Over three months, his attacks dropped from 7 to 2 per month, and he could walk to the mailbox without a cane.
Both cases underline a pattern: pairing a hearing solution with a balance‑monitoring tool yields the biggest quality‑of‑life boost.
Next Steps and Resources
Now that you know the landscape, here’s how to move forward:
- Schedule an appointment with an otolaryngologist to get a current audiogram.
- Ask about a trial of a bone‑conduction aid if you have fluid‑related fluctuations.
- Download a reputable dizziness‑tracking app (e.g., DizzEase, VertiLog).
- Consider a vestibular rehabilitation device if you’ve had more than three falls in the past six months.
- Join an online Meniere’s community; peer reviews often point out hidden device quirks.
Remember, assistive technology isn’t a one‑size‑fits‑all. It’s an evolving toolbox you fine‑tune as your symptoms change.
Frequently Asked Questions
Can a hearing aid worsen vertigo?
Modern hearing aids have sophisticated motion sensors that actually help stabilize balance. Only very old analog models without noise reduction could increase auditory overload, indirectly amplifying anxiety‑related dizziness.
Do pressure‑sensing earplugs work for everyone?
They’re most effective for people whose attacks correlate with rapid inner‑ear pressure spikes (about 60% of Meniere’s patients). Those with primarily stress‑triggered attacks may see less benefit.
Is a cochlear implant covered by insurance?
In the United States, Medicare and most private plans cover cochlear implants when severe sensorineural hearing loss is documented and hearing aids no longer provide functional benefit. Pre‑authorization is usually required.
How long should I use a vestibular rehab device each day?
Therapists typically recommend 10‑15 minutes of guided exercises twice daily. Consistency beats duration; short, frequent sessions help the brain re‑learn stable balance cues.
Are there any risks with bone‑conduction hearing aids?
The main risk is skin irritation at the headband site. Switching to a surgical abutment can eliminate that, but it requires a minor procedure. Otherwise, device‑related complications are rare.
Should I combine a hearing aid with a balance device?
Yes. The two address different symptom clusters. When both auditory clarity and vestibular feedback improve, overall confidence rises dramatically, as shown in multiple patient‑reported outcome studies.






7 Comments