Swallowing seems simple until it stops working. You eat a bite of food, and it feels stuck. Not just uncomfortable-impossible. That’s dysphagia, and for many, it’s not just a nuisance. It’s a sign something deeper is wrong with the esophagus. When the muscles that push food down don’t fire right, you’re dealing with an esophageal motility disorder. These aren’t rare. They’re underdiagnosed, often mistaken for heartburn or GERD. But the truth is, proton pump inhibitors won’t fix a broken esophagus.
What Exactly Is Going On in Your Esophagus?
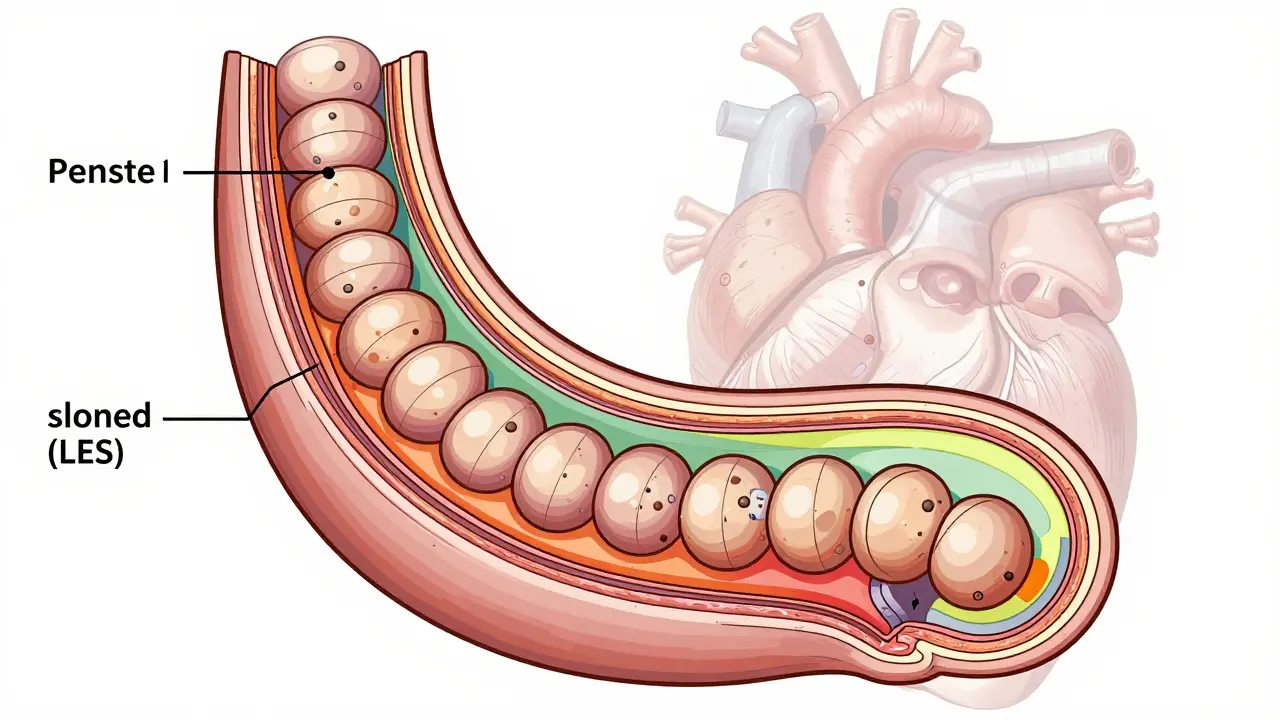
Your esophagus isn’t just a tube. It’s a muscular highway. Every time you swallow, coordinated waves-called peristalsis-squeezes food toward your stomach. At the bottom, the lower esophageal sphincter (LES) opens just enough to let food through, then snaps shut to keep stomach acid from creeping back up. When this system fails, things get messy.Some disorders are clear-cut. Achalasia, for example, means the LES won’t relax. The esophagus stops contracting. Food piles up. People with achalasia often lose weight, regurgitate undigested food, and wake up choking. Others have wild, uncoordinated contractions-like nutcracker esophagus, where every swallow feels like a muscle spasm, or jackhammer esophagus, where contractions are so strong they cause chest pain that mimics a heart attack.
Then there are the secondary causes. If you have scleroderma, your body attacks its own tissues. The esophagus gets stiff, thin, and weak. Up to 80% of scleroderma patients develop motility problems. It’s not the esophagus failing on its own-it’s a symptom of a bigger disease.
Dysphagia: The Symptom Everyone Ignores
Dysphagia sounds like a medical term, but it’s simple: trouble swallowing. The problem isn’t always obvious. At first, it’s just hard to get down solids. Then liquids. Then saliva. Patients often say, “I’ve been eating soft foods for years.” They don’t realize their body is struggling. By the time they see a doctor, they’ve lost 15 to 20 pounds on average.What makes dysphagia tricky is that it looks like other things. Chest pain from a spastic esophagus? People rush to the ER thinking it’s a heart attack. Regurgitation? They assume it’s acid reflux. And for years, they take PPIs-medications that reduce stomach acid-but those don’t help if the issue is muscle failure, not acid.
A 2022 survey from the International Foundation for Gastrointestinal Disorders found that nearly 70% of people with motility disorders waited 2 to 5 years for a correct diagnosis. Many saw three or more doctors. One patient wrote online: “I was on PPIs for eight years before manometry showed I had jackhammer esophagus.” That’s not just delay-it’s harm.
Manometry: The Only Way to See the Real Problem
You can’t diagnose these disorders with blood tests or X-rays alone. You need to see the muscles in action. That’s where high-resolution manometry (HRM) comes in.HRM uses a thin, flexible tube with 36 pressure sensors spaced every centimeter. It’s passed through the nose into the esophagus. As you swallow water, the sensors record pressure changes in real time. The result? A color-coded map showing exactly where the contractions are weak, strong, or chaotic.
This isn’t new tech-it’s the standard now. Before HRM, doctors used older methods that missed up to 22% of achalasia cases. HRM catches 96%. It’s the reason we now classify achalasia into three clear types: Type I (no contractions), Type II (pan-esophageal pressurization), and Type III (spastic contractions). Each type guides treatment.
The Chicago Classification v4.0, updated in 2023, is the rulebook everyone uses. It defines what’s normal, what’s abnormal, and what’s just noise. Before this, doctors disagreed on diagnoses. Now, with HRM and standardized criteria, agreement between specialists has jumped from moderate to excellent.
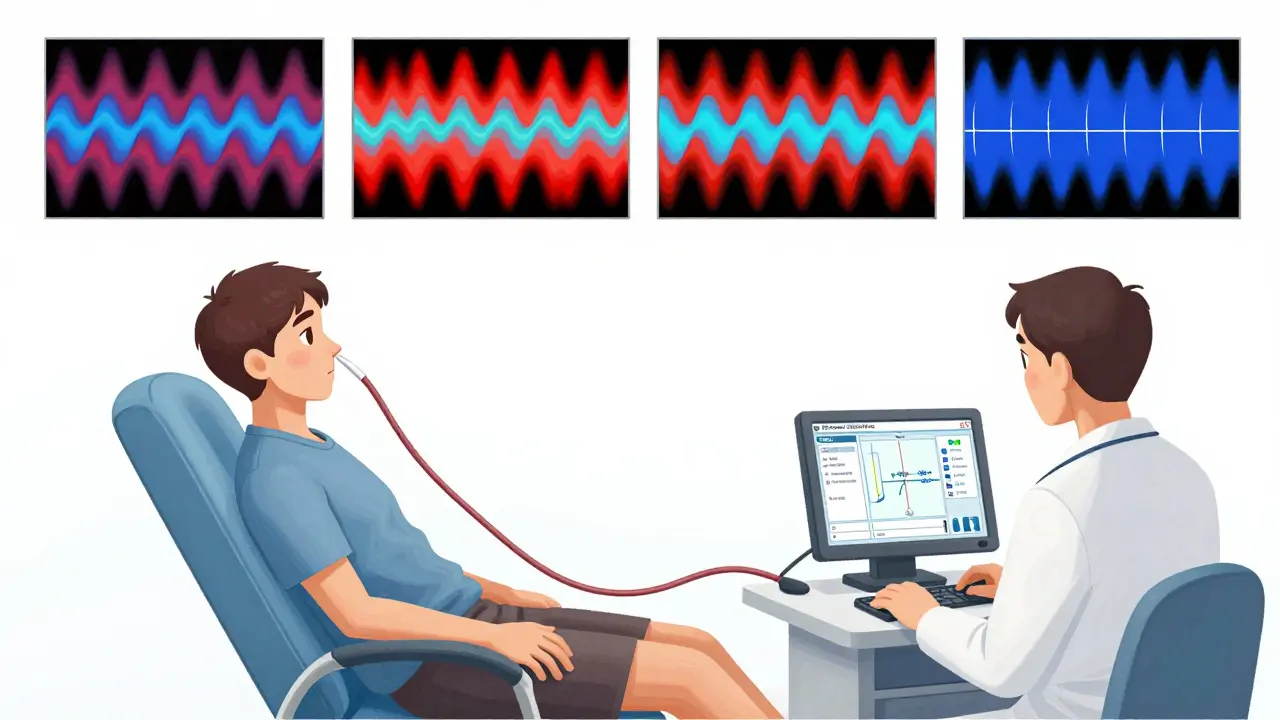
What Manometry Reveals That Other Tests Miss
Barium swallow used to be the go-to test. You drink chalky liquid, and X-rays track how it moves. But it’s blurry. It shows structure, not function. A barium swallow might miss a weak squeeze or a sphincter that won’t open. HRM catches it.EndoFLIP is another tool. It measures how stretchy the esophagus is-useful for checking if the LES is too stiff. But it’s not a replacement. It’s a complement. HRM tells you how the muscles contract. EndoFLIP tells you how much they can stretch. Together, they give a full picture.
Even newer is the wireless capsule-SmartPill. You swallow a pill that records pressure and pH for 24 to 48 hours as you go about your day. It’s less invasive, and early data shows it matches HRM in 85% of cases. But it’s not yet ready to replace HRM for detailed diagnosis.
One big downside? HRM is uncomfortable. About 35% of patients report pain or nausea during the test. That’s why education matters. Patients who know what to expect report 78% satisfaction. Those who don’t? Only 45%. Clear instructions-like “swallow when I say so”-make all the difference.
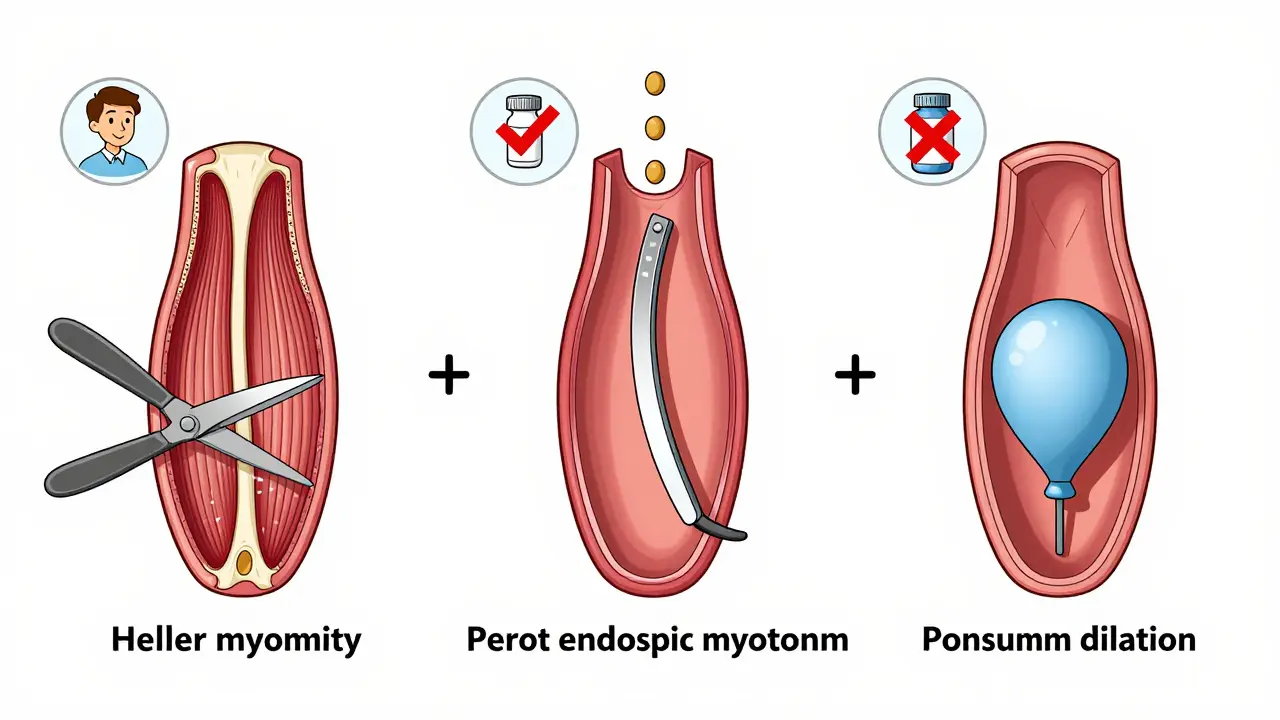
Treatment: From Surgery to New Tech
Treatment depends on what’s broken. For achalasia, the goal is to open the LES. There are three main options:- Laparoscopic Heller myotomy (LHM): Surgeons cut the muscle fibers of the LES. It’s effective-85% to 90% of patients feel better after five years. But it can cause reflux.
- Peroral endoscopic myotomy (POEM): A scope goes down the throat, and the surgeon cuts the muscle from inside. Just as effective as LHM, but more likely to cause reflux (44% at two years vs. 29% with LHM).
- Pneumatic dilation: A balloon is inflated in the LES to stretch it open. Works for 70% to 80% of people at first, but many need repeat treatments within five years.
For spastic disorders like nutcracker or jackhammer esophagus, medications like calcium channel blockers or Botox injections can help. But they’re temporary. Surgery isn’t usually an option here.
Newer tools are emerging. The LINX device-a ring of magnetic beads placed around the LES-helps some patients with preserved peristalsis. It’s not for everyone, but early results show 75% symptom improvement in a year.
And then there’s AI. Researchers are training algorithms to read HRM tracings. In one study, AI identified achalasia with 92% accuracy-better than untrained doctors. It’s not replacing specialists yet, but it’s helping them spot patterns faster.
Why Diagnosis Takes So Long-and What You Can Do
The delay in diagnosis isn’t just bad luck. It’s systemic. HRM machines cost $50,000 to $75,000. Only academic centers and big GI practices have them. Community hospitals? Often don’t. Rural areas? Rarely.Doctors aren’t always trained to think of motility disorders. If a patient says, “My chest hurts,” the default is cardiac workup. If they say, “I can’t swallow,” the default is endoscopy for cancer or strictures. Motility testing only happens if those are ruled out.
Here’s what you can do: If you’ve had dysphagia for more than a few months, and PPIs aren’t helping, ask for a referral to a motility specialist. Bring your symptom history. Note when it started, what foods trigger it, if you’ve lost weight, if you regurgitate. That’s the data they need.
And if you’re told, “It’s just GERD,” but you’re not improving-push back. Ask: “Could this be an esophageal motility disorder?” It’s not rude. It’s smart.
The Future Is More Precise, But Access Is Still Unequal
The field is moving fast. Chicago Classification v4.0 made diagnosis reliable. AI tools are speeding up interpretation. Wireless capsules are making testing less invasive. The global market for esophageal diagnostics is growing at 7.5% a year.But access? Still a problem. In North America and Europe, 95% of academic centers have HRM. In low-income countries, it’s under 10%. That’s not just a tech gap-it’s a health equity gap.
What’s clear is this: esophageal motility disorders aren’t rare quirks. They’re real, treatable conditions that wreck lives when ignored. The tools to fix them exist. The knowledge is there. What’s missing is awareness-among patients and doctors alike.
If you’re struggling to swallow, don’t wait for it to get worse. Don’t assume it’s acid. Ask for the right test. Because sometimes, the thing that’s blocking your food isn’t in your stomach-it’s in your esophagus, and it can be fixed.






13 Comments