Extended-Release Side Effect Estimator
When you pick up a prescription, you might not think twice about whether it’s a tablet, capsule, or extended-release pill. But the form you’re taking can make a big difference in how your body handles the drug - and how you feel while taking it. The difference isn’t just about size or shape. It’s about how and when the medicine gets into your system. And that directly affects your side effects, how often you need to take it, and even whether you stick with the treatment.
Immediate-Release Tablets: Fast On, Fast Off
Immediate-release tablets are the most common type. They’re designed to break down quickly in your stomach, releasing the full dose within 30 to 60 minutes. Peak drug levels hit your bloodstream in about 1 to 2 hours. That’s great if you need fast relief - like pain from a headache or a sudden flare-up of anxiety. But here’s the catch: that quick spike can also mean quick side effects. High peak concentrations are linked to 25-40% more concentration-dependent side effects, according to a review of 15 studies comparing immediate-release and extended-release versions of the same drug. For example, people taking immediate-release bupropion for depression report more nausea and jitteriness right after taking the pill. That’s because the drug hits hard and fast. Tablets also have a longer shelf life than capsules - often 2 to 3 years longer at room temperature. That makes them cheaper to store and easier for pharmacies to stock. But they take longer to dissolve than capsules. On average, capsules absorb 20-30% faster because their gelatin shells dissolve quicker than the compressed powder in tablets.Capsules: Faster Absorption, Less Stability
Capsules come in two main types: hard-shell and soft-gel. Both are filled with powder, liquid, or pellets. The outer shell dissolves fast, letting the drug enter your system more quickly than tablets. That’s why some medications, like certain antibiotics or sleep aids, are only available as capsules. But capsules aren’t perfect. They’re more sensitive to heat and moisture. If you leave them in a hot bathroom or a sunny car, they can stick together or degrade faster than tablets. That’s why they’re often packaged in blister packs instead of bottles. They also don’t last as long on the shelf - sometimes just 18 to 24 months. Side effects from capsules are similar to tablets because the drug inside is usually the same. But because they’re absorbed faster, the onset of side effects can feel more intense. People with sensitive stomachs often notice nausea or heartburn sooner with capsules than with tablets.Extended-Release (ER, XR, XL): Steady Dose, Fewer Peaks
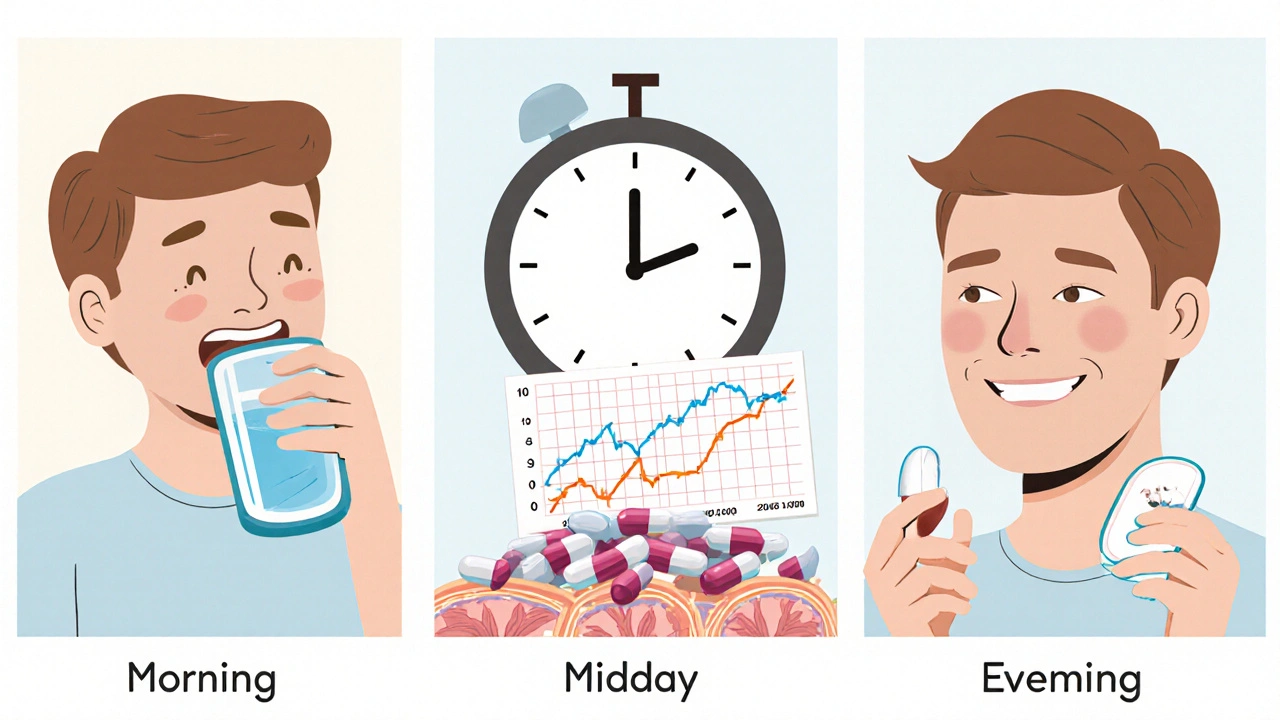
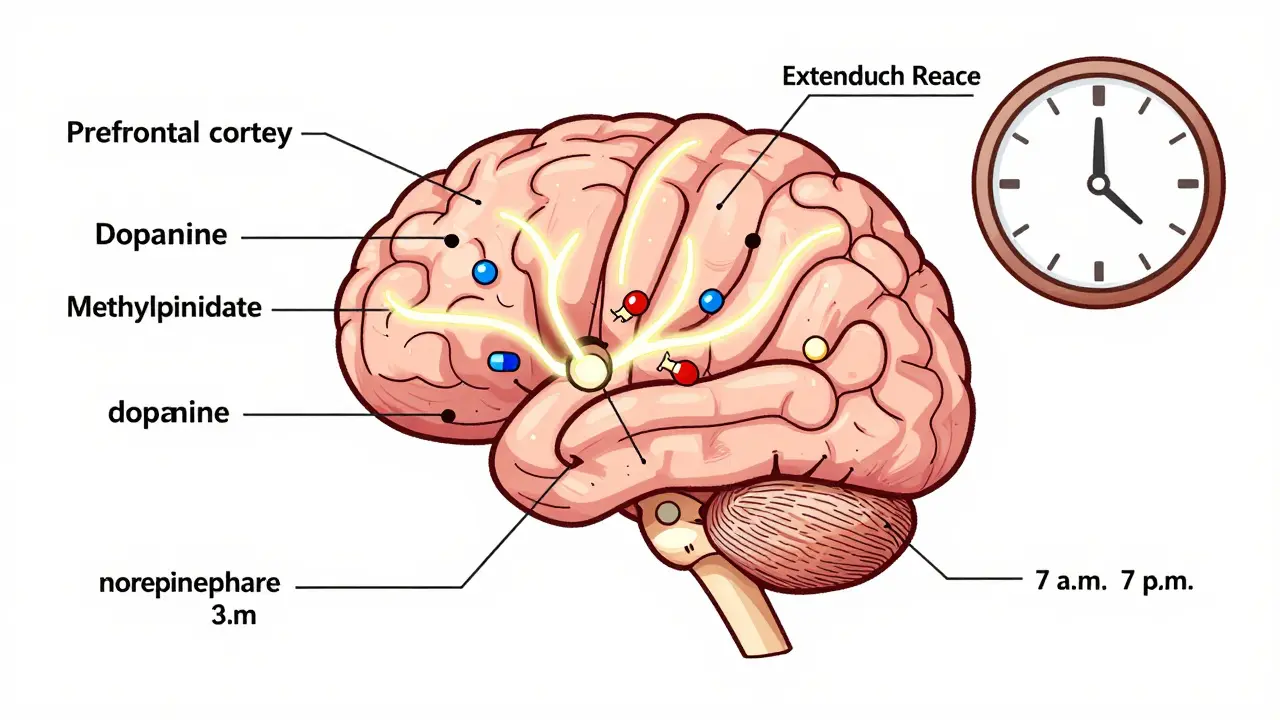
Extended-release formulations - labeled ER, XR, or XL - are designed to release medication slowly over 12 to 24 hours. Instead of one big spike, you get a steady trickle. That’s why drugs like Wellbutrin XL, Effexor XR, and Trokendi XR are taken just once a day, instead of two or three times. The technology behind these pills is complex. Some use hydrophilic matrices (like HPMC gel) that swell in your stomach and slowly release the drug. Others use hydrophobic polymers or osmotic pumps that push the medicine out through tiny laser-drilled holes. These systems are precise - but they’re also fragile. The biggest benefit? Fewer side effects. Clinical trials show extended-release bupropion reduces nausea by 30% compared to its immediate-release version. Effexor XR cuts dizziness by 22% and nausea by 18%. Why? Because your body isn’t flooded with the drug all at once. Peak-to-trough fluctuations drop from 4-6:1 in immediate-release to just 1.5-2.5:1 in extended-release. That’s why doctors often switch patients from immediate-release to extended-release when side effects become unbearable. A 2022 study found that 4 out of 7 comparisons showed significantly better tolerability with ER versions of epilepsy and psychiatric drugs.When Extended-Release Goes Wrong
Extended-release sounds ideal - until it doesn’t work. These formulations are designed to work in a healthy digestive system. If you have gastroparesis, Crohn’s disease, or have had gastric surgery, the pill might not move through your gut properly. That can lead to incomplete release - meaning you get less medicine than you need. Even worse: dose dumping. If the coating cracks or the tablet is crushed, chewed, or dissolved, the entire dose can flood your system at once. That’s dangerous. People have ended up in the ER after crushing extended-release oxycodone or methylphenidate. The FDA has issued multiple warnings about this. Another problem? Food. About 15% of extended-release drugs are affected by high-fat meals. A fatty breakfast can speed up or slow down absorption by 20-35%. That’s why some ER pills say “take on an empty stomach” - and why skipping meals can throw off your whole dosing schedule.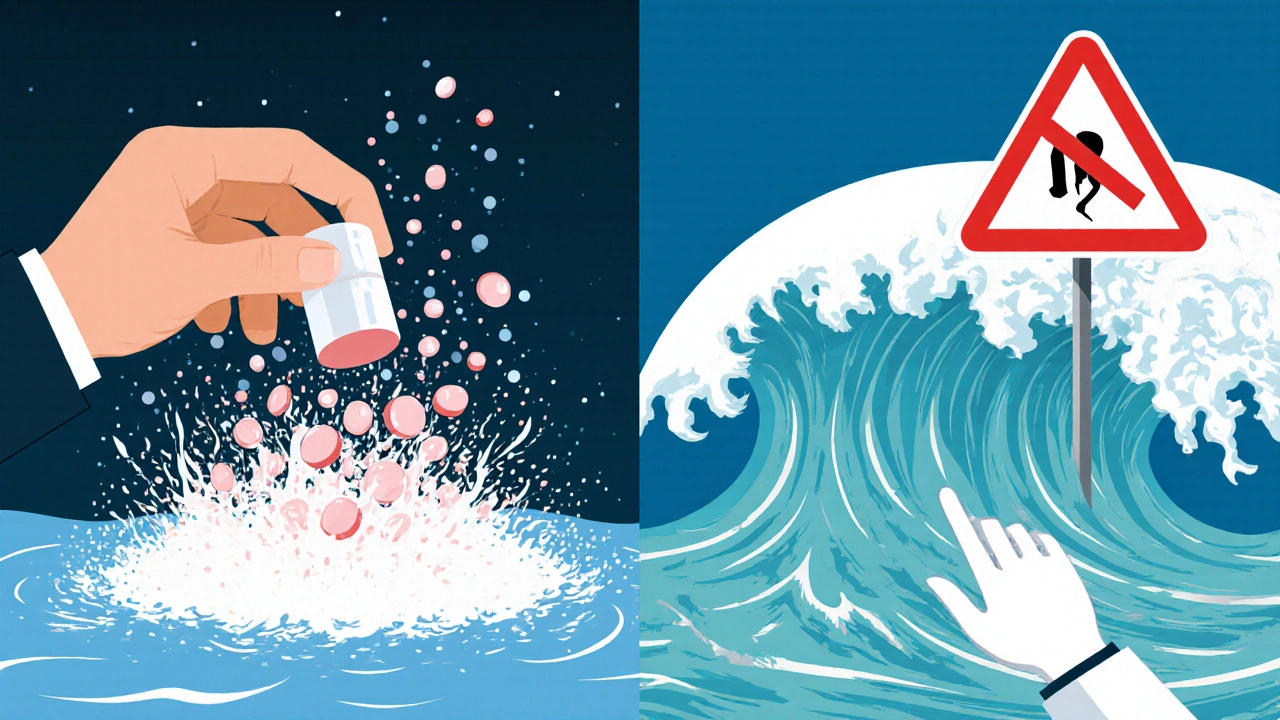
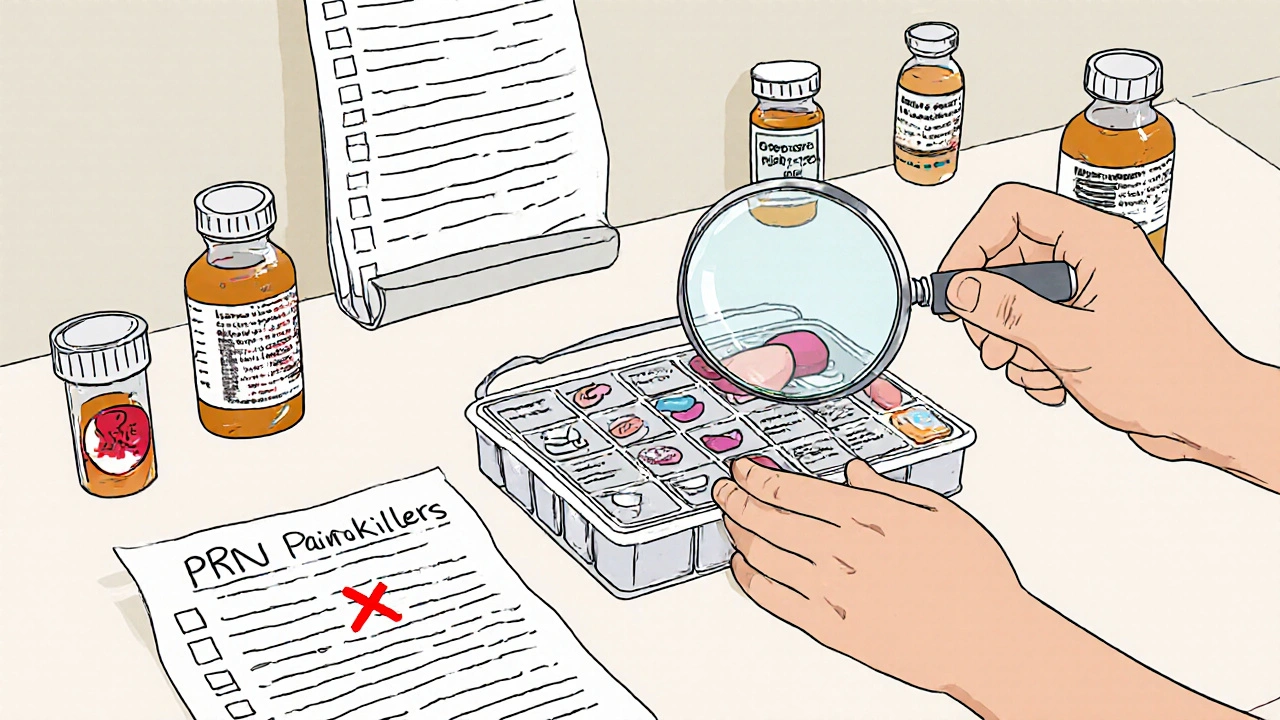
Can You Split or Crush Them?
Never. Ever. Unless the label says it’s safe. Many extended-release tablets have a special coating or core that controls the release. Breaking them destroys that mechanism. Even if it looks like a regular tablet, it might not be. Some ER pills are made of tiny pellets inside a capsule - crushing them releases all the drug at once. Patients with swallowing difficulties face a real challenge. Extended-release tablets are often larger and harder than regular ones. A 2022 Mayo Clinic survey found that 27% of elderly patients struggled with swallowing ER pills. Some manufacturers now make smaller ER tablets or offer liquid versions, but they’re not always available.Cost and Convenience: The Trade-Off
Extended-release versions cost more. On average, they’re 2.3 times the price of immediate-release equivalents. For example, Wellbutrin XL can run $185 a month, while generic bupropion costs $15. That’s a huge barrier for people without good insurance. But the cost isn’t just in dollars. It’s in adherence. One case study tracked a bipolar patient who took three daily doses of immediate-release quetiapine. Adherence was only 65%. After switching to once-daily ER, adherence jumped to 92%. Mood episodes dropped by 47% in 12 months. Patients on Drugs.com rate extended-release medications 4.2 out of 5 stars - higher than immediate-release’s 3.8. Why? Because 68% of positive reviews mention fewer pills to take, and 52% say side effects are lighter.What the Labels Really Mean
Not all “slow-release” labels are the same. Here’s what to look for:- ER, XR, XL = Extended-release. Slow, steady release over 12-24 hours.
- SR = Sustained-release. Often similar to ER, but not always identical.
- DR = Delayed-release. Designed to pass through the stomach and release in the intestines (like enteric-coated aspirin or valproate).
What Doctors Want You to Know
Prescribers are more likely to recommend extended-release for chronic conditions: depression, epilepsy, high blood pressure, ADHD, and Parkinson’s. The American College of Clinical Pharmacy says ER formulations are ideal when peak-related side effects limit dosing with immediate-release versions. But they also warn: don’t use ER if you have delayed stomach emptying, recent GI surgery, or severe constipation. The drug might not move through your system at all. And titrating doses is harder. ER pills come in fixed strengths. If you need a 75mg dose but only have 50mg and 100mg, you can’t split it. That forces some patients to take a higher dose than needed - or switch to immediate-release.The Future: Smarter Pills
Newer ER technologies are getting smarter. Rytary, for Parkinson’s, releases medication in three pulses throughout the day - reducing “off” time by over two hours. Other systems in development can stay in the stomach for 24 hours or release drugs only in specific parts of the intestine. But challenges remain. Polymer coatings from these pills are showing up in wastewater - a hidden environmental cost. And regulatory agencies are tightening requirements. The FDA now demands stricter testing to prove these pills work the same in all patients, not just healthy volunteers.What Should You Do?
If you’re on a medication that causes side effects, ask your doctor: “Is there an extended-release version?” It might reduce nausea, dizziness, or sleep problems. If you’re switching from immediate-release to extended-release, give it a few weeks. Your body needs time to adjust to the new rhythm. Never crush, split, or chew pills unless your pharmacist or doctor says it’s safe. And if you have trouble swallowing pills - tell your provider. There might be liquid, sprinkle, or smaller tablet options you didn’t know about. Extended-release isn’t magic. But when it works, it makes life easier. Fewer pills. Fewer side effects. Better control. And that’s worth knowing about.Can I crush an extended-release tablet if I have trouble swallowing?
No. Crushing an extended-release tablet can cause the entire dose to be released at once, which may lead to dangerous side effects or overdose. These pills are designed to release medication slowly. Breaking them destroys that mechanism. If swallowing is a problem, talk to your doctor or pharmacist - there may be liquid, sprinkle, or smaller-dose alternatives available.
Why do extended-release medications cost more?
Extended-release formulations require more complex manufacturing, specialized materials like polymers, and longer development times - often 36 to 48 months compared to 18-24 for regular pills. They also undergo stricter testing to ensure consistent release. These factors drive up costs. On average, ER versions cost 2.3 times more than their immediate-release equivalents.
Do food and meals affect extended-release drugs?
Yes. About 15% of extended-release medications are affected by food - especially high-fat meals. A fatty meal can speed up or slow down how the drug is released, changing its effectiveness. Some ER pills must be taken on an empty stomach. Always check the label or ask your pharmacist about food interactions.
Are extended-release pills better for side effects?
Often, yes. Because they release medication slowly, they avoid the high peak concentrations that cause side effects like nausea, dizziness, and jitteriness. Studies show extended-release versions of antidepressants, ADHD meds, and seizure drugs reduce side effects by 18-30% compared to immediate-release versions.
What’s the difference between SR, ER, and XR?
SR (sustained-release) and ER/XR (extended-release) are often used interchangeably, but they’re not always the same. ER/XR typically means release over 12-24 hours. SR may mean slower release but not necessarily full-day coverage. DR (delayed-release) means the drug doesn’t release until it reaches the intestines. Never assume they’re interchangeable - always check the specific drug’s prescribing information.
Can I take an extended-release pill twice a day if I miss a dose?
No. Extended-release pills are designed for once-daily dosing. Taking two at once can cause a dangerous overdose. If you miss a dose, take it as soon as you remember - but only if it’s within 12-24 hours, depending on the drug. Never double up. Always check with your pharmacist or doctor for specific instructions.
Why do some extended-release pills have different names?
Brand-name extended-release versions often have suffixes like XL (extended-release), XR (extended-release), or ER (extended-release). Generic versions may not include these, so you need to check the active ingredient and formulation. For example, Wellbutrin XL is the brand name for bupropion XL. The generic is just “bupropion XL.” Always confirm the release type - not just the drug name - when switching brands or generics.




8 Comments