When you or your child struggles with focus, impulsivity, or constant restlessness, it’s easy to feel like you’re fighting an invisible battle. ADHD isn’t just about being distracted or fidgety-it’s a neurodevelopmental condition that affects how the brain manages attention, emotion, and action. And while it can feel overwhelming, the good news is there are clear, research-backed ways to manage it. The most effective approach doesn’t rely on just one thing. It’s a mix of medication, behavior changes, and daily routines that work together. This isn’t about quick fixes. It’s about building a system that helps you or your child live better, day after day.
Stimulants: The Fast-Acting Core of ADHD Treatment
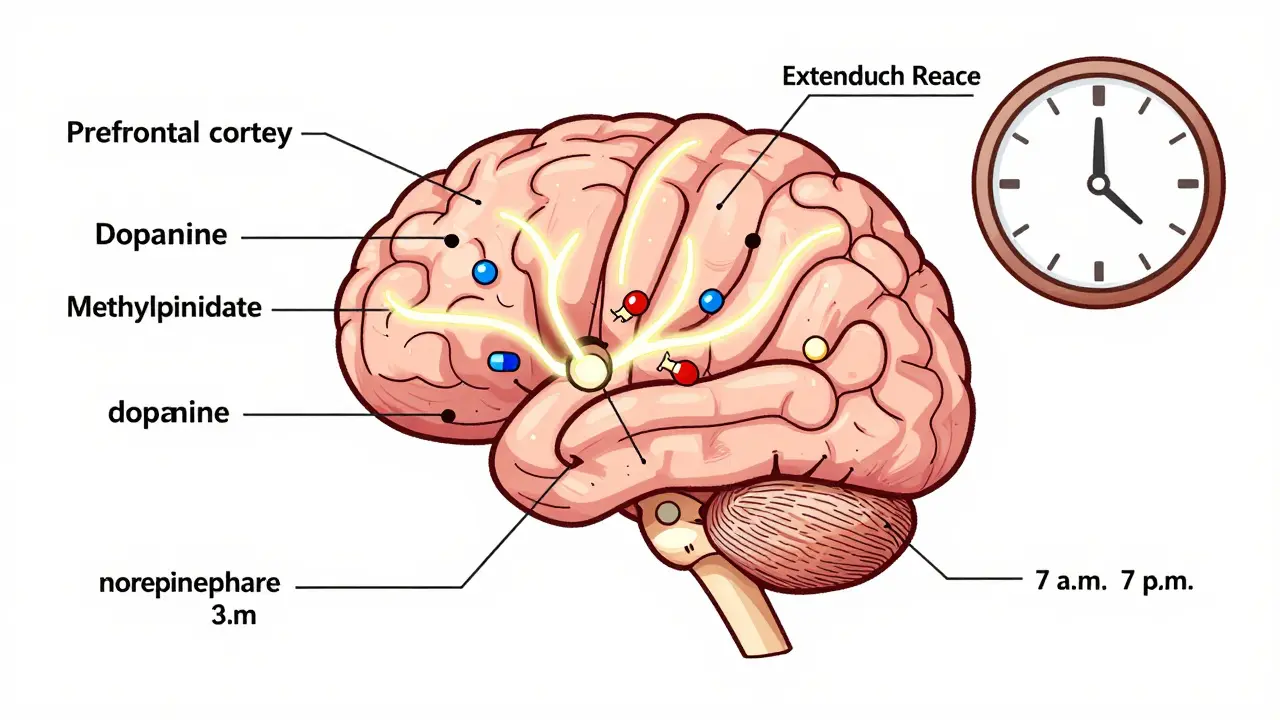
Stimulants are the most commonly prescribed medications for ADHD-and for good reason. About 70 to 80% of people who try them see real improvement in focus, impulse control, and task completion. These aren’t energy boosters like coffee. They work by increasing dopamine and norepinephrine in the prefrontal cortex, the part of the brain that helps you plan, focus, and control impulses. Think of them as a quiet reset button for the brain’s internal control system.
The two main types are methylphenidate and amphetamine-based drugs. Methylphenidate includes brands like Ritalin, Concerta, and Focalin. Amphetamines include Adderall, Vyvanse, and Dexedrine. The difference isn’t just the name-it’s how long they last and how they’re absorbed. Immediate-release versions kick in within 30 minutes but wear off in 3 to 4 hours. Extended-release versions like Concerta or Vyvanse last 10 to 12 hours, which means fewer doses, fewer disruptions, and more stable symptom control throughout the school or workday.
But they’re not without trade-offs. Appetite suppression hits 50 to 60% of kids on stimulants. Some people lose interest in food during the day and end up eating more at night. Sleep problems are common too-about 30 to 50% of users struggle to fall asleep, especially if the last dose is too late. Headaches, stomachaches, and mood swings as the medication wears off (called “rebound”) are also frequent. One parent on a popular forum described it like this: “My son’s fine at school, but by 5 p.m., he’s a volcano. He yells over spilled milk. It’s not him-it’s the medicine fading.”
Doctors usually start low: 5 mg of methylphenidate or 2.5 mg of amphetamine once a day. Then they slowly increase every week until symptoms improve or side effects become too much. For kids, height and weight are checked every six months. About 30% see a temporary dip in growth during the first year, but most catch up by year three. Blood pressure is monitored too-stimulants can raise it slightly in 2 to 5% of users. That’s why a baseline check is required before starting.
Non-Stimulants: Slower But Safer Alternatives
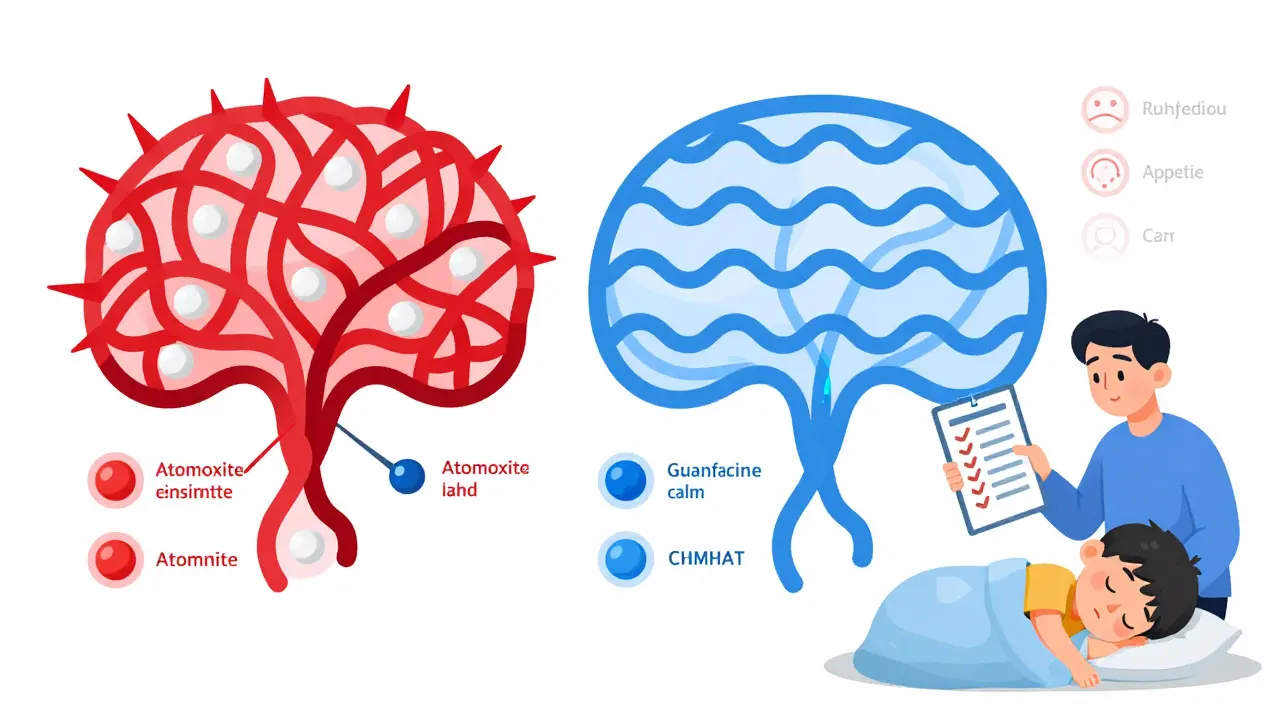
If stimulants don’t work-or cause too many side effects-there are non-stimulant options. They don’t kick in as fast. It can take 4 to 6 weeks before you notice real change. But they’re often chosen for people with anxiety, tics, a history of substance use, or heart concerns.
Atomoxetine (Strattera) is the most common. It works by increasing norepinephrine, similar to stimulants, but without the same risk of misuse. It’s not addictive. About 50 to 60% of users respond well. Side effects include nausea, tiredness, and, in rare cases, liver issues. It’s often used in teens and adults who want to avoid the “high” feeling some report with stimulants.
Guanfacine (Intuniv) and clonidine (Kapvay) are blood pressure medications repurposed for ADHD. They calm the nervous system by targeting alpha-2 receptors in the brain. They’re especially helpful for emotional outbursts, impulsivity, and sleep problems. A parent of a 9-year-old with ADHD told me: “We switched from Adderall to Intuniv because he was too emotional. Now he’s calmer at home, sleeps better, and doesn’t bounce off the walls at bedtime.”
Non-stimulants don’t suppress appetite as much. They don’t cause the same level of sleep disruption. And they’re safer for people with heart conditions. But they’re less effective for pure inattention. If your main struggle is staying on task, stimulants still win. But if your child melts down over small frustrations, or can’t fall asleep no matter what, non-stimulants might be the better fit.
Behavioral Strategies: The Long-Term Foundation
Medication helps you manage symptoms. Behavioral strategies help you build skills that last. You can’t take a pill to organize your desk, plan your homework, or pause before yelling. Those skills have to be learned-and practiced.
For kids, parent training is one of the most powerful tools. Programs like the New Forest Parenting Programme require 12 to 16 weekly sessions, each 90 minutes long. That sounds intense. But studies show 40 to 50% of kids show major improvement in behavior when parents learn to give clear, calm instructions, use consistent rewards, and avoid power struggles. It’s not about being stricter. It’s about being clearer. Instead of saying, “Clean your room,” you say, “Put your clothes in the hamper, your books on the shelf, and your toys in the bin. I’ll check in 10 minutes.” Then you follow through.
School accommodations matter too. A 504 Plan or IEP can give extra time on tests, preferential seating, checklists, and breaks. Teachers who understand ADHD don’t see a “bad kid.” They see a brain that needs structure. One teacher in Auckland told me: “I started giving my ADHD students a 5-minute heads-up before transitions. No more meltdowns. Just quiet, focused movement.”
For adults, organizational tools like digital calendars, task apps (Todoist, TickTick), and time-blocking help. Breaking big tasks into 15-minute chunks makes them feel possible. Setting alarms for “start now” instead of “do this later” reduces procrastination. And mindfulness practices-even 5 minutes a day-help with emotional regulation. One adult with ADHD shared: “I used to quit everything when I got frustrated. Now I pause, breathe, and say, ‘What’s the next tiny step?’ It changes everything.”
Putting It All Together: What Works Best
The best outcomes don’t come from medication alone. They come from combining it with behavior changes. The landmark MTA study from 1999 showed that kids who got both medication and behavioral therapy did better than those who got only one. They had fewer symptoms, better social skills, and improved family relationships.
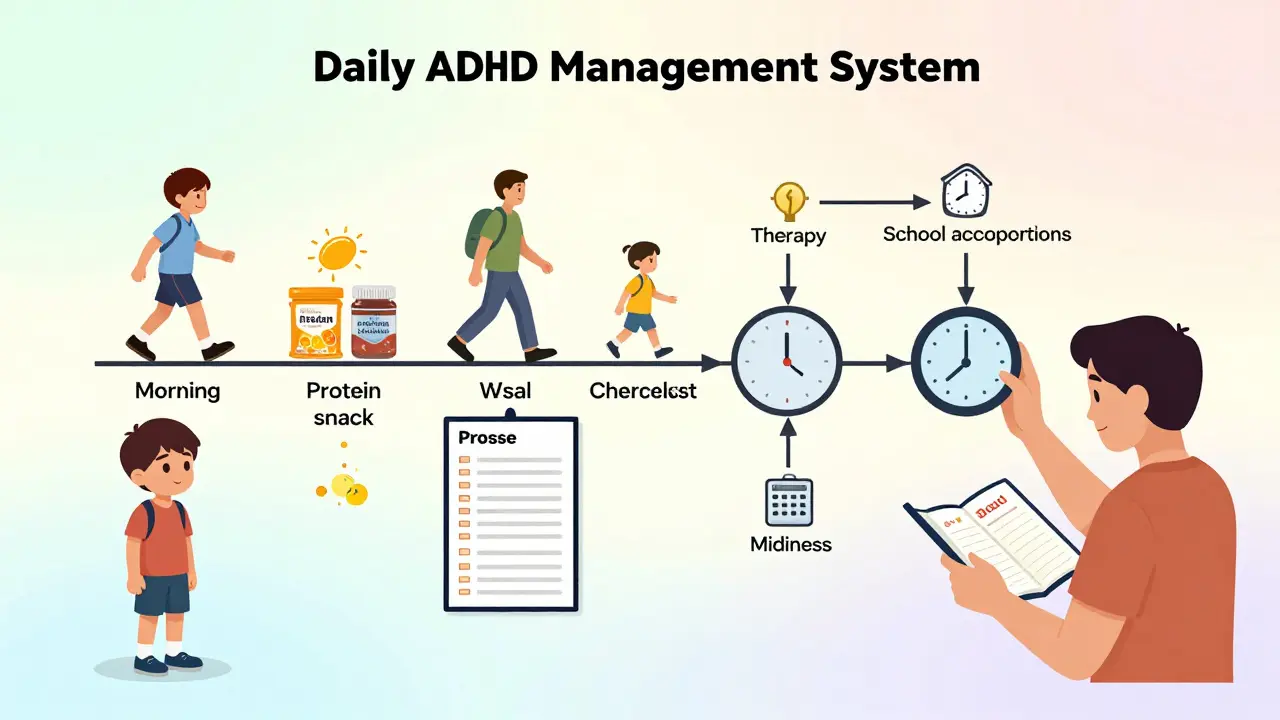
Here’s how it looks in real life:
- A 10-year-old takes Concerta in the morning. At lunch, they get a protein-rich snack to fight appetite loss. At 4 p.m., they have a 20-minute walk outside. At 7 p.m., they use a visual checklist to pack their backpack. Their parents use praise charts for chores.
- An adult takes Vyvanse for focus at work. They use a Pomodoro timer (25 minutes work, 5 minutes break). They keep a “brain dump” journal to clear mental clutter. They see a therapist monthly to work on emotional triggers.
- A teenager on Strattera practices daily journaling to track mood swings. Their school allows them to record lectures instead of taking notes. They get 10 extra minutes on tests.
The key isn’t perfection. It’s consistency. You don’t need to do everything perfectly every day. You just need to keep showing up. Some days, the medication works great. Other days, you rely on your routines. That’s normal.
What to Watch Out For
Not everyone responds the same way. And side effects aren’t always obvious at first.
Some people feel emotionally flat on stimulants-like they’re going through the motions without joy. This is called “emotional blunting.” It’s not rare. On Reddit’s r/ADHD, 31% of users reported it. If you or your child seems less expressive, less excited, or just “off,” talk to your doctor. Adjusting the dose or switching meds can help.
Girls and women often experience more side effects than boys and men. One study found females reported side effects 1.4 times more often. They’re also more likely to have anxiety or depression alongside ADHD, which can complicate treatment. If you’re a woman with ADHD and stimulants make you feel more anxious or tearful, it’s not your fault. It’s a biological difference.
Preschoolers respond differently too. Alpha-2 agonists like guanfacine cause fewer mood swings and appetite issues in young kids than stimulants. The American Academy of Pediatrics now recommends behavioral therapy as the first step for children under 6. Medication is only added if symptoms are severe and behavior therapy hasn’t helped.
And cost matters. Generic methylphenidate costs $15 to $25 a month. Brand-name extended-release versions can hit $250 to $400 without insurance. Many U.S. insurers require you to try the cheapest option first. That’s called step therapy. If your child can’t tolerate it, you can appeal. Don’t assume you can’t afford help-ask your doctor about patient assistance programs.
What’s New in 2025
ADHD treatment is evolving. In 2023, the FDA approved AZSTARYS-a new combo drug designed to reduce abuse risk while lasting 13 hours. In 2024, the American Academy of Pediatrics updated guidelines to recommend screening for eating disorders before starting stimulants, since appetite loss can trigger dangerous patterns in vulnerable people.
Genetic testing is starting to help too. Tests like Genomind’s PGx Express can tell if your body metabolizes stimulants slowly or quickly based on your CYP2D6 and CYP2C19 genes. If you’re a slow metabolizer, you might need a lower dose. If you’re a fast one, you might need more. This isn’t routine yet-but it’s coming.
Digital tools are also gaining ground. EndeavorRx, an FDA-cleared video game for kids 8 to 12, improves attention through targeted cognitive training. VR-based programs are now in late-stage trials. These aren’t replacements for medication or therapy-but they’re helpful extras.
Final Thoughts: It’s Not One Size Fits All
There’s no magic pill. No perfect plan. ADHD treatment is personal. What works for your neighbor might not work for you. Some people thrive on stimulants. Others do better with non-stimulants. Some need behavior coaching. Others need school accommodations. Many need all of it.
The goal isn’t to “fix” someone. It’s to give them the tools to manage their brain-not fight it. You don’t have to be perfect. You just have to be persistent. Track what works. Talk to your doctor. Adjust. Try again. Progress isn’t linear. But it’s real.
Do stimulants make ADHD worse over time?
No. Long-term studies, including the 20-year follow-up of the MTA study, show stimulants don’t harm brain development or worsen symptoms over time. Some people stop taking them in adolescence because they feel they no longer need them, or because of side effects-but the medication itself doesn’t cause decline. In fact, consistent use is linked to better academic and social outcomes in adulthood.
Can you outgrow ADHD?
ADHD is a lifelong condition, but how it shows up changes. Many adults learn coping strategies that make symptoms less disruptive. Hyperactivity often fades, but inattention and impulsivity may persist. About 60% of children with ADHD still have symptoms as adults, though they may manage them better with experience, structure, and sometimes continued treatment.
Are non-stimulants weaker than stimulants?
Not weaker-just different. Non-stimulants are less effective for core attention symptoms but better for emotional regulation and sleep. They’re not a backup option-they’re a different tool. Someone with severe emotional outbursts might respond better to guanfacine than to Adderall. Effectiveness depends on the person’s specific symptoms, not the drug category.
How do I know if my child’s medication isn’t working?
Look for three things: no improvement in school performance, no change in social interactions, or worsening behavior after the medication wears off (rebound). If your child’s teacher says they’re still disruptive, or if they come home exhausted and irritable every day, it’s time to revisit the plan. Don’t wait months. Ask for a medication review after 4 to 6 weeks.
Is behavioral therapy just for kids?
No. Adults benefit from cognitive behavioral therapy (CBT) for ADHD too. CBT helps with time management, emotional regulation, and reducing self-criticism. Many adults with ADHD feel ashamed or frustrated. Therapy helps them reframe their experiences-not as failures, but as challenges with solutions.
Can I stop medication if I feel better?
Don’t stop suddenly. Even if you feel fine, your brain may still need the support. Work with your doctor to slowly reduce the dose and monitor symptoms. Some people can stop successfully; others relapse. It’s not a sign of weakness to need ongoing treatment. It’s like wearing glasses-you don’t stop using them just because you feel okay.
ADHD treatment isn’t about finding the perfect drug. It’s about finding the right mix of tools that let you live your life-without constantly fighting your own brain. Start small. Track progress. Ask for help. You’re not alone.




11 Comments