Heart disease kills women more than all cancers combined. Yet most women still don’t realize it’s their biggest health threat. In the U.S. alone, about 307,000 women die from heart disease every year - that’s 1 in every 5 female deaths. Globally, it’s 8.9 million women annually. And here’s the problem: the symptoms aren’t what you see in movies. No clutching the chest, no dramatic collapse. For women, it’s often fatigue so deep you can’t make your bed. Or jaw pain that feels like a toothache. Or nausea that comes out of nowhere during a normal day.
Why Women’s Heart Disease Looks Different
For decades, heart research was done mostly on men. The famous Framingham Heart Study, which shaped how we understand heart disease, included only men. That meant the medical world learned what a heart attack looks like in men - and assumed women were the same. They’re not. Women’s hearts are smaller. Their arteries are narrower. Hormones change how blood flows and how pain signals travel. That’s why women get types of heart disease that men rarely do: microvascular disease (damage to tiny heart arteries), spontaneous coronary artery dissection (SCAD - a tear in the artery wall), and Takotsubo syndrome (stress-induced heart failure). These don’t show up on standard tests designed for men. And they don’t cause the same crushing chest pain. A 2023 study from Yale Medicine found that 43% of women who had heart attacks didn’t have chest pain at all. Instead, they had fatigue, shortness of breath, nausea, or back pain. These symptoms are often dismissed as stress, anxiety, or aging. But they’re not. They’re warning signs.What Symptoms Women Actually Experience
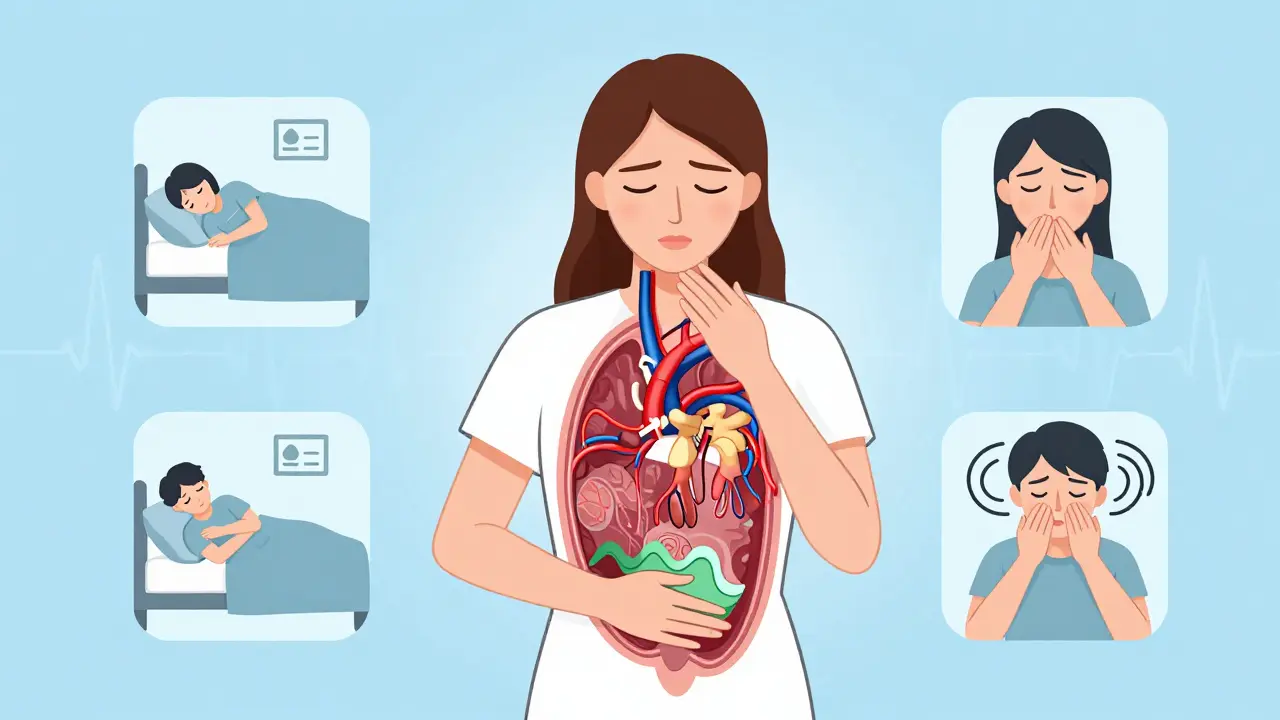
Here’s what real heart attacks look like in women, based on data from the American Heart Association and the National Heart, Lung, and Blood Institute:- Unexplained fatigue - Not just tired. So tired you can’t do normal things. This happens in 71% of women before or during a heart attack.
- Shortness of breath - Even when sitting still or doing light chores. It’s not from being out of shape. It’s your heart struggling.
- Pain in the jaw, neck, back, or arms - Often on the left side, but not always. It can feel like a dull ache or pressure. Many women think it’s arthritis or a pulled muscle.
- Nausea, vomiting, or indigestion - Especially if it comes with sweating or dizziness. Women are 59% more likely than men to mistake this for a stomach bug.
- Dizziness or lightheadedness - Not from standing up too fast. This can be your heart not pumping enough blood.
- Chest discomfort - When women do feel it, it’s rarely sharp pain. It’s more like pressure, tightness, or a heavy weight. Some say it feels like “a bra that’s too tight.”
One of the most dangerous myths is that heart attacks only happen during physical exertion. For women, they often strike during rest - even while sleeping. A 2023 Cleveland Clinic study found that women who wake up with unexplained chest pressure, nausea, or sweating are at high risk.
Why Women Are More Likely to Be Misdiagnosed
Women under 55 are seven times more likely than men to be sent home from the ER with a misdiagnosis. Why? Because their symptoms don’t match the old male-centered model. Doctors - even well-meaning ones - often assume it’s anxiety, acid reflux, or menopause. A 2022 JAMA Internal Medicine study found that in 68% of emergency cases where women had cardiac symptoms, providers labeled them as “emotional” or “anxious.” That bias is real. And deadly. Women also wait longer to seek help. On average, they delay treatment by 2.3 hours longer than men. Why? Because they don’t recognize the signs. Or they think they’re being dramatic. Or they’re caring for others and put themselves last. The result? A 50% higher chance of dying within a year after a misdiagnosed heart attack. That’s not just a statistic. That’s a mother, a sister, a friend - someone who could have been saved.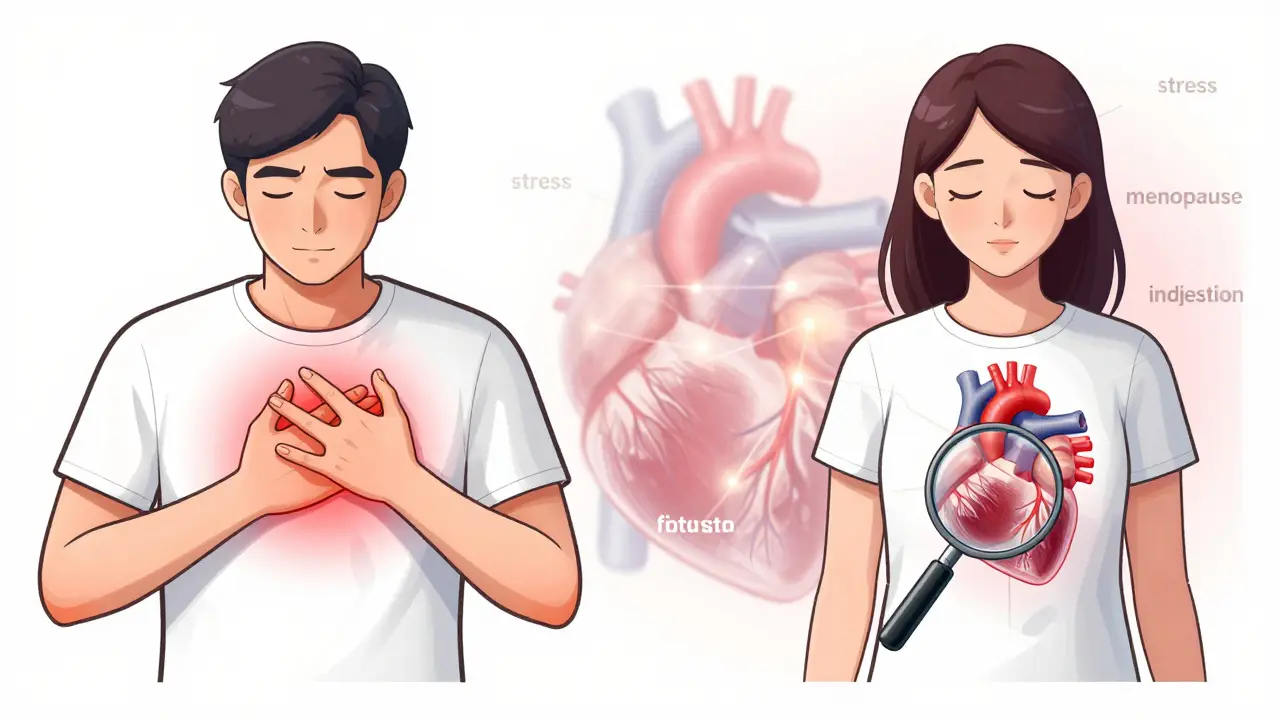
Hidden Risk Factors Only Women Have
Some risks for heart disease are unique to women. These aren’t just “lifestyle” issues - they’re biological.- Pregnancy complications - Preeclampsia (high blood pressure during pregnancy) increases future heart disease risk by 80%. Gestational diabetes doubles it. These aren’t just “pregnancy problems.” They’re early warning signs.
- Early menopause - If you went through menopause before 45, your risk jumps. Estrogen protects blood vessels. When it drops, so does that protection.
- Polycystic ovary syndrome (PCOS) - This hormonal disorder is linked to insulin resistance, high blood pressure, and higher cholesterol - all heart disease risks.
- Autoimmune diseases - Lupus, rheumatoid arthritis, and other conditions that mostly affect women also damage blood vessels and raise heart risk.
- Stress and depression - Mental stress triggers angina 37% more often in women than men. Chronic stress raises cortisol, which increases inflammation and blood pressure.
These aren’t “side notes.” They’re critical parts of your heart health profile. If you’ve had preeclampsia or early menopause, you need to talk to your doctor - not just about birth control or hot flashes, but about your heart.
What You Can Do to Protect Yourself
Knowing the symptoms is only half the battle. The other half is acting on them - and managing your risks before it’s too late.- Track your symptoms - Keep a simple log: “Day 1: Felt too tired to walk to mailbox. Day 3: Jaw ached for 20 minutes after cooking.” Write it down. Show it to your doctor. Don’t downplay it.
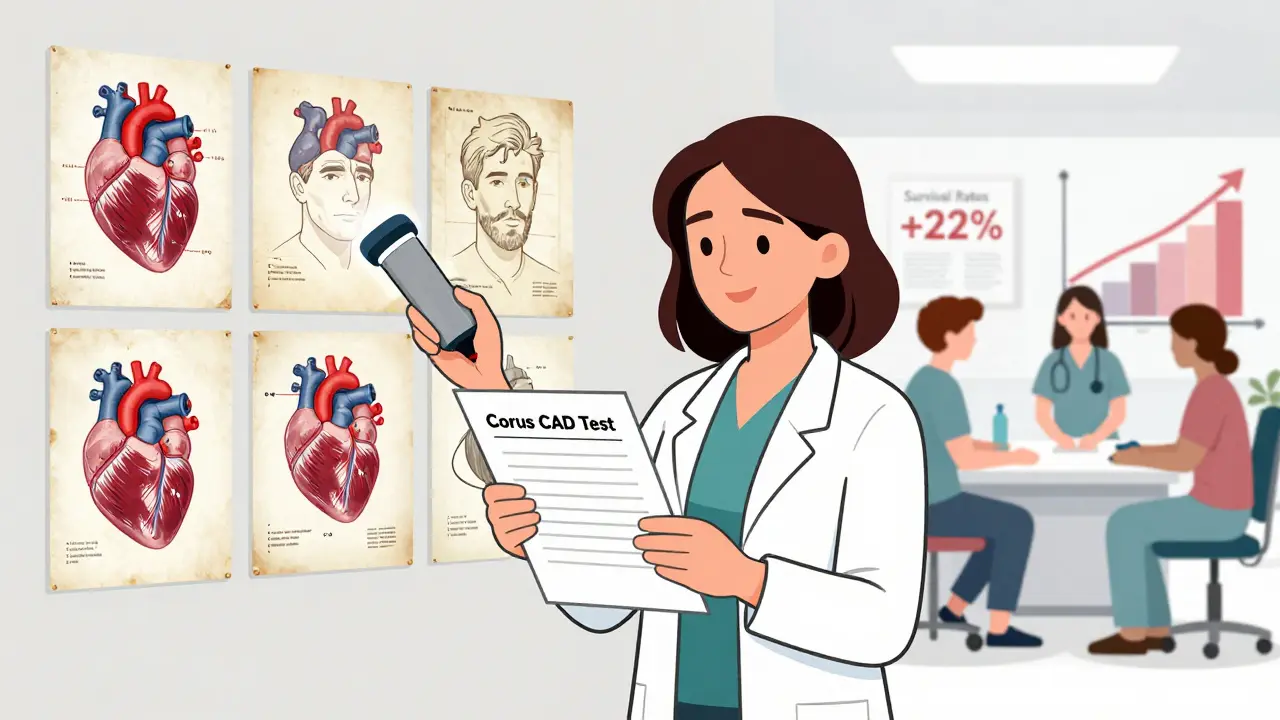
- Get tested differently - Standard stress tests and angiograms miss microvascular disease. Ask about the Corus CAD test - a blood test that analyzes gene patterns to detect blockages in women with 88% accuracy. It’s FDA-approved and covered by many insurers.
- Find a women’s heart specialist - Hospitals with Women’s Cardiovascular Centers of Excellence (147 in the U.S. as of 2023) have protocols designed for female patients. They reduce diagnostic delays by 25% or more. If you’re in a major city, look for one.
- Manage stress like your life depends on it - Because it does. Try daily walks, yoga, or talking to a therapist. Even 15 minutes of deep breathing lowers blood pressure and reduces inflammation.
- Don’t ignore your menstrual and reproductive history - Your gynecologist should know your heart risks. Your cardiologist should know your pregnancy history. Make sure those conversations happen.
There’s no magic pill. But there are proven steps. And they work. The American Heart Association’s “Go Red for Women” campaign increased symptom recognition by 27% between 2004 and 2020. That’s 10 million women learning to speak up - and saving lives.
When to Go to the ER - No Excuses
If you have three or more of these symptoms - even if they’re mild - go to the ER immediately:- Unexplained fatigue lasting more than two weeks
- Shortness of breath during light activity
- Jaw, neck, or back pain
- Nausea or vomiting with sweating
- Dizziness or fainting
Don’t wait to see if it goes away. Don’t call your doctor tomorrow. Go now. Every minute counts. Heart muscle dies quickly when it’s starved of oxygen. And women’s symptoms are often subtle - but the damage is just as real.
There’s no shame in being wrong. There’s only shame in staying silent.
What’s Changing - And What You Should Know
Good news: things are shifting. In January 2023, the National Heart, Lung, and Blood Institute launched RENEW - a $150 million initiative to study sex-specific heart disease. The FDA approved the first diagnostic tool designed for women in 2020. AI tools are being trained to spot female-specific patterns in symptoms and test results. But progress won’t save you unless you know what to look for. And you won’t know unless you’re told - clearly, directly, without medical jargon. So here’s your takeaway: Heart disease isn’t a man’s disease. It’s a woman’s disease - and it’s killing you quietly. Your symptoms matter. Your body knows. Trust it. Speak up. Get tested. Don’t wait for the pain to be “bad enough.”Do women have heart attacks without chest pain?
Yes. About 43% of women who have heart attacks don’t feel chest pain at all. Instead, they experience fatigue, shortness of breath, nausea, jaw or back pain, or dizziness. These symptoms are often mistaken for other conditions, which is why women are more likely to be misdiagnosed.
Is heart disease really the #1 killer of women?
Yes. Heart disease kills more women than all forms of cancer combined. In the U.S., it causes 1 in every 5 female deaths. Globally, it claims 8.9 million women’s lives each year - more than the next seven leading causes of death for women combined.
Can stress cause a heart attack in women?
Absolutely. Mental stress triggers angina (chest pain from reduced blood flow) 37% more often in women than in men. Severe emotional stress can also cause Takotsubo syndrome - a temporary heart failure that mimics a heart attack. Chronic stress raises blood pressure and inflammation, both major risk factors.
What’s the best test for heart disease in women?
Traditional stress tests and angiograms often miss microvascular disease, which is common in women. The Corus CAD test - a blood test that analyzes gene expression - is validated for women and detects coronary artery disease with 88% accuracy. Ask your doctor if it’s right for you, especially if you have symptoms but normal test results.
Does menopause increase heart disease risk?
Yes. After menopause, estrogen levels drop, and that protective effect on blood vessels disappears. Women who go through menopause before age 45 have a significantly higher risk. Hormone replacement therapy doesn’t lower heart risk - but managing blood pressure, cholesterol, and weight after menopause does.
Can pregnancy complications predict future heart disease?
Yes. Preeclampsia increases future heart disease risk by 80%. Gestational diabetes doubles it. These aren’t just pregnancy problems - they’re early red flags. If you had either, you should get regular heart screenings starting at age 40 - or sooner if other risk factors are present.
Why are women more likely to die after a heart attack?
Women are more likely to be misdiagnosed, delay treatment, and have heart attacks caused by conditions like microvascular disease that aren’t treated the same way. They’re also more likely to have other health issues like diabetes or kidney disease that complicate recovery. But when treated at specialized women’s heart centers, survival rates improve by 22%.
Next Steps: What to Do Today
1. Write down your symptoms - Even if they seem small. Fatigue? Jaw ache? Nausea after walking? Write it down. 2. Call your doctor - Say: “I’m concerned about my heart. I’ve had [list symptoms]. I’d like to be screened for microvascular disease or get a Corus CAD test.” 3. Find a women’s heart center - Search online for “Women’s Cardiovascular Center of Excellence” near you. These clinics know how to test and treat women correctly. 4. Talk to your mom, sister, daughter - Share this. Most women still don’t know the signs. You could save their life.Heart disease doesn’t announce itself with a siren. It whispers. Listen. Act. Don’t wait for the pain to be worse. Because by then, it might be too late.






14 Comments