GI Bleeding Risk Calculator
Combining systemic steroids (like prednisone) with NSAIDs (ibuprofen, naproxen) increases your risk of serious gastrointestinal bleeding by up to 12x. This tool helps you assess your personal risk based on key factors.
Enter your information to see your risk level
When you’re on a short course of prednisone for a flare-up and still need pain relief for your arthritis, it’s tempting to reach for ibuprofen or naproxen. But combining these two common medications can be dangerous - and many people don’t know it. The truth is, taking systemic corticosteroids and NSAIDs together can raise your risk of a life-threatening gastrointestinal bleed by more than 12 times compared to using either drug alone. This isn’t a rare side effect. It’s a well-documented, preventable medical hazard that shows up in emergency rooms every week.
Why This Combination Is So Dangerous
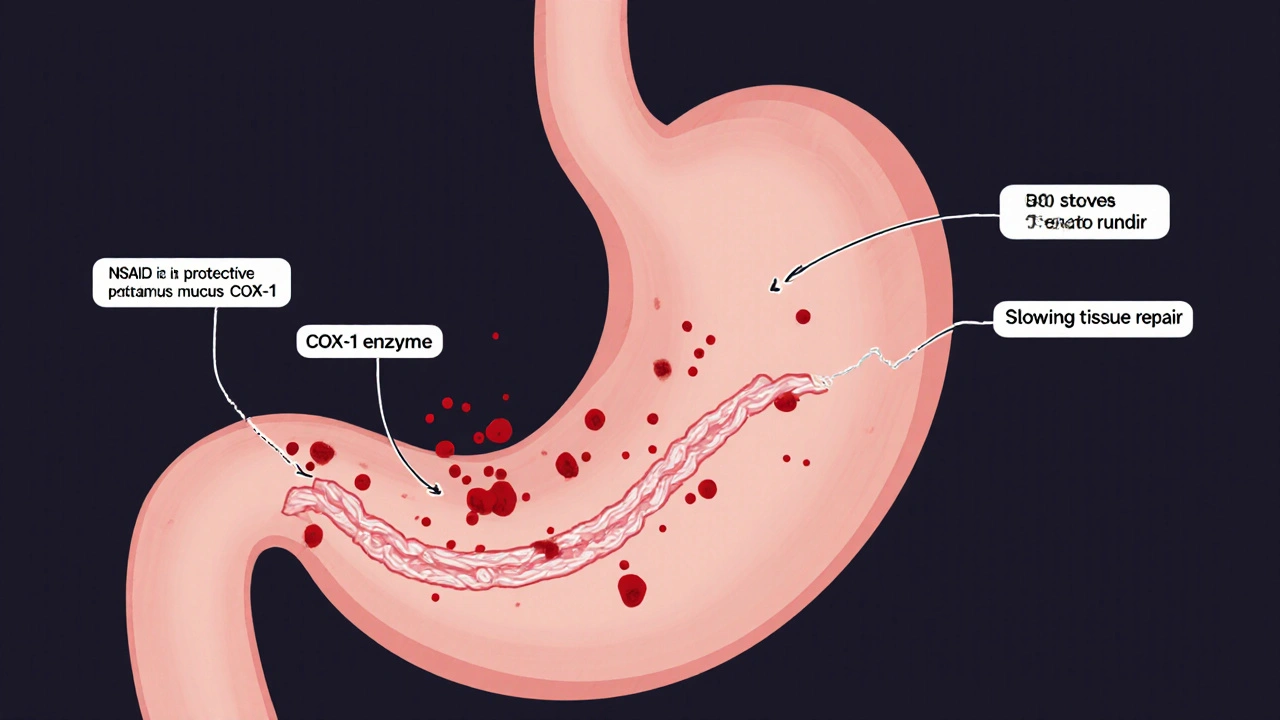
NSAIDs like ibuprofen, naproxen, and diclofenac work by blocking enzymes called COX-1 and COX-2. COX-2 helps with inflammation and pain, which is why these drugs feel effective. But COX-1 is the enzyme your stomach relies on to make protective mucus and maintain blood flow to the stomach lining. When NSAIDs shut down COX-1, your stomach loses its natural defense system. That’s why even healthy people can develop ulcers from long-term NSAID use. Corticosteroids like prednisone make things worse. They don’t directly cause ulcers. Instead, they sabotage your body’s ability to heal. Steroids slow down tissue repair, reduce mucus production, and - critically - mask the early warning signs. If you get a stomach ulcer while on steroids, you might not feel the classic burning pain. That means you won’t know something’s wrong until it’s too late: a bleed starts, and you suddenly feel dizzy, weak, or pass dark, tarry stools. Studies show the risk isn’t linear - it’s multiplicative. Taking an NSAID alone might raise your GI bleeding risk by 3 to 4 times. Add steroids, and that risk jumps to 8 to 12 times higher. For people over 65, with a past ulcer, or on blood thinners like warfarin, the numbers climb even further. One study found that patients on high-dose NSAIDs plus steroids had an odds ratio of 12.7 for bleeding - meaning they were over 12 times more likely to have a serious GI event than someone taking neither drug.It’s Not Just Your Stomach at Risk
Most people think of NSAID-related bleeding as a peptic ulcer problem - something in the upper GI tract. But research shows nearly one-third of NSAID-induced bleeds happen in the lower intestine, not the stomach. These can be harder to detect, slower to diagnose, and just as deadly. A 1999 study found that 86% of patients with lower GI bleeding had taken NSAIDs. That means even if you don’t have heartburn or indigestion, you’re still at risk. The danger isn’t limited to prescription NSAIDs. Over-the-counter ibuprofen and naproxen are just as risky when combined with steroids. Many patients assume OTC means safe - but when you’re on prednisone, even a single daily tablet of Advil can push you into danger territory.Not All NSAIDs Are Created Equal
If you need an NSAID while on steroids, not all options are the same. Traditional NSAIDs - like naproxen, diclofenac, and high-dose ibuprofen - are the worst offenders. They block both COX-1 and COX-2, wiping out your stomach’s protection. COX-2 selective inhibitors like celecoxib (Celebrex) are safer. They spare COX-1, so they cause less damage to the stomach lining. Studies show they reduce upper GI bleeding risk by 50-60% compared to traditional NSAIDs. But here’s the catch: even celecoxib isn’t risk-free when combined with steroids. The risk is lower, but it’s still there. And if you’re on aspirin for heart protection, the combination with steroids still requires extra caution. The best approach? Avoid traditional NSAIDs entirely if you’re on steroids. If you absolutely need pain relief, talk to your doctor about celecoxib - but only if you’re also getting a proton pump inhibitor (PPI).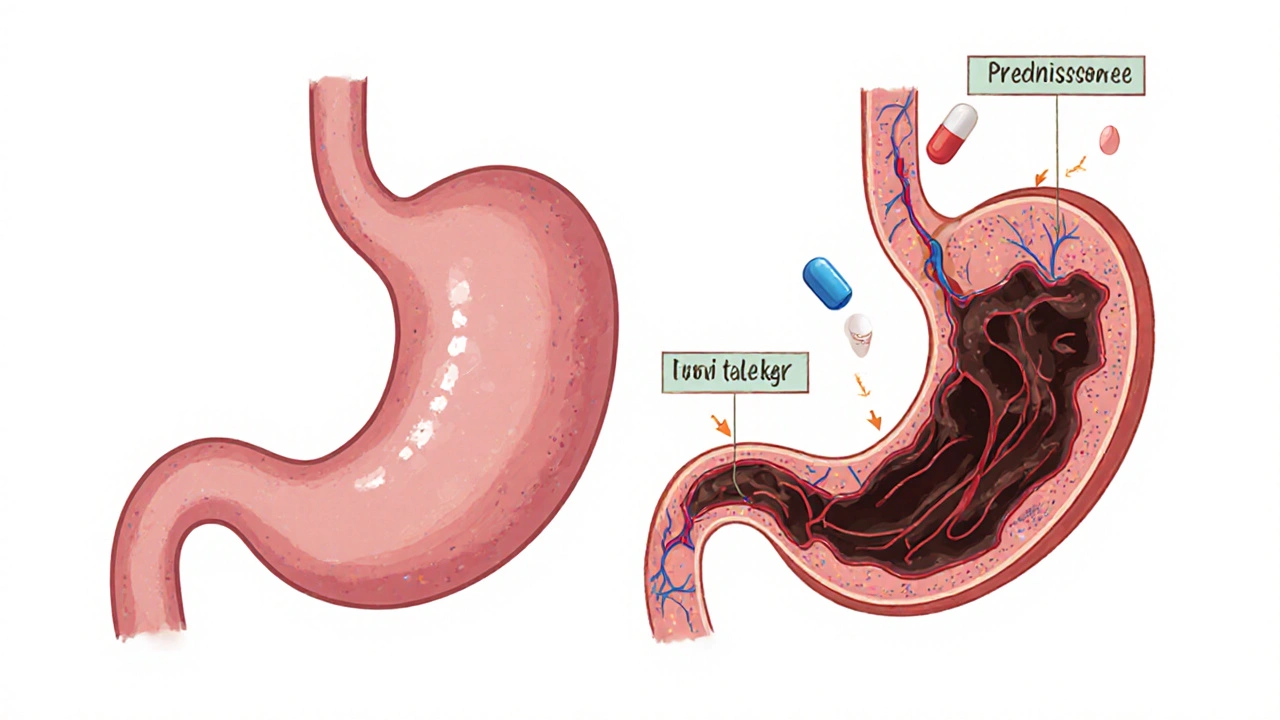
What Actually Works: The Only Proven Prevention
The American College of Gastroenterology, the European Society of Gastrointestinal Endoscopy, and the American Gastroenterological Association all agree: if you’re taking both steroids and NSAIDs, you need a PPI. That’s not a suggestion. It’s a medical standard. PPIs like omeprazole, esomeprazole, or pantoprazole work by shutting down the stomach’s acid pumps. Less acid means less irritation to damaged tissue, and it gives your stomach a chance to heal. PPIs reduce the risk of NSAID-induced ulcers by over 70%. H2 blockers like famotidine (Pepcid) are not enough - they’re only half as effective. For most people, a standard dose like omeprazole 20mg once daily is sufficient. But if you’re over 65, have a history of ulcers, or are on blood thinners, you may need double the dose - 40mg daily. Don’t assume your doctor will automatically prescribe it. Studies show only about 39% of patients on this dangerous combo actually get a PPI. In non-specialist clinics, the rate drops below 22%. A 2023 study found that hospitals using automated clinical alerts to co-prescribe PPIs with NSAID/steroid orders reduced bleeding events by nearly 70%. That’s not magic - it’s systems working the way they should.What You Should Do Right Now
If you’re currently taking steroids and NSAIDs together, here’s what to do:- Stop assuming it’s safe. Even a 5-day steroid burst raises your bleeding risk within 7 days.
- Check your meds. Are you taking ibuprofen, naproxen, or diclofenac? If yes, and you’re on prednisone or another steroid, you’re in a high-risk group.
- Ask your doctor for a PPI. Say: “I’m on steroids and NSAIDs. Do I need a proton pump inhibitor to protect my stomach?”
- Don’t switch to H2 blockers. Pepcid or Zantac won’t cut it. Only PPIs have proven effectiveness.
- Watch for warning signs. Black or tarry stools, vomiting blood, sudden dizziness, or abdominal pain that doesn’t go away - call your doctor immediately.

Why This Keeps Happening
This isn’t a failure of science - it’s a failure of practice. Doctors know the risk. But many don’t think to ask if patients are taking OTC NSAIDs. Patients don’t know to mention them. The FDA requires GI bleeding warnings on NSAID labels - but none of them specifically warn about the steroid interaction. A 2023 survey of 842 patients who had a GI bleed while on both drugs found that 63% had never been warned about this risk by their prescriber. One Reddit user, a gastroenterologist, wrote: “I see preventable bleeds weekly from primary care providers starting prednisone bursts in patients already on chronic ibuprofen without adding PPIs.” The cost of ignoring this is huge. In the U.S. alone, combination-related GI bleeds cost the healthcare system $1.87 billion a year. Most of those cases could have been prevented with a $10-a-month PPI.What’s Changing - and What’s Next
There’s hope. In 2023, the FDA approved Vimovo - a single pill combining naproxen and esomeprazole - for high-risk patients. It’s not a magic bullet, but it’s a step forward. Some health systems like Kaiser Permanente and Mayo Clinic now automatically co-prescribe PPIs with NSAID/steroid orders. Their bleeding rates have dropped dramatically. Researchers are also looking at genetics. Early data suggests some people carry gene variants that make them 2.3 times more likely to suffer GI damage from this combo. In the future, a simple blood test might tell you if you’re in the high-risk group. For now, the answer is simple: if you’re on steroids and NSAIDs, you need a PPI. No exceptions. No gray areas. It’s not optional. It’s not a suggestion. It’s the only thing standing between you and a serious, potentially fatal bleed.Can I take Tylenol instead of NSAIDs while on steroids?
Yes. Acetaminophen (Tylenol) doesn’t affect COX-1 or the stomach lining, so it’s the safest pain reliever to use with steroids. It won’t reduce inflammation like NSAIDs, but it’s effective for pain and fever without raising GI bleeding risk. Always check with your doctor if you’re unsure about dosing, especially if you have liver issues.
How long should I take a PPI if I’m on steroids and NSAIDs?
Take the PPI for the entire time you’re on both medications - and for at least 2 weeks after you stop the last one. The risk doesn’t disappear the day you quit the drugs. Healing takes time, and your stomach lining needs ongoing protection until it’s fully recovered. Stopping the PPI too early is a common mistake that leads to delayed bleeds.
Are there natural alternatives to protect my stomach?
No. While some people suggest probiotics, licorice, or aloe vera for gut health, none of these have been shown to prevent NSAID-steroid induced bleeding. Only PPIs have proven, evidence-based effectiveness. Relying on supplements instead of a PPI puts you at serious risk. Don’t gamble with your GI tract.
Is this risk the same for inhaled or topical steroids?
No. Inhaled steroids (like those in asthma inhalers) and topical steroids (creams or ointments) don’t enter your bloodstream in significant amounts, so they don’t increase GI bleeding risk when combined with NSAIDs. The danger only applies to systemic steroids - pills, injections, or IV forms like prednisone, methylprednisolone, or dexamethasone.
What if I’m on low-dose aspirin for heart health?
Low-dose aspirin (81mg) already increases GI bleeding risk on its own. Adding NSAIDs and steroids creates a triple threat. In this case, you absolutely need a PPI - and you should avoid traditional NSAIDs completely. Celecoxib with a PPI is the safest NSAID option if you must use one, but even then, the combination should be avoided if possible. Talk to your cardiologist and gastroenterologist together about your options.





8 Comments