Clozapine ANC Monitoring Calculator
Enter Start Date
Your Monitoring Schedule
Current Monitoring Period
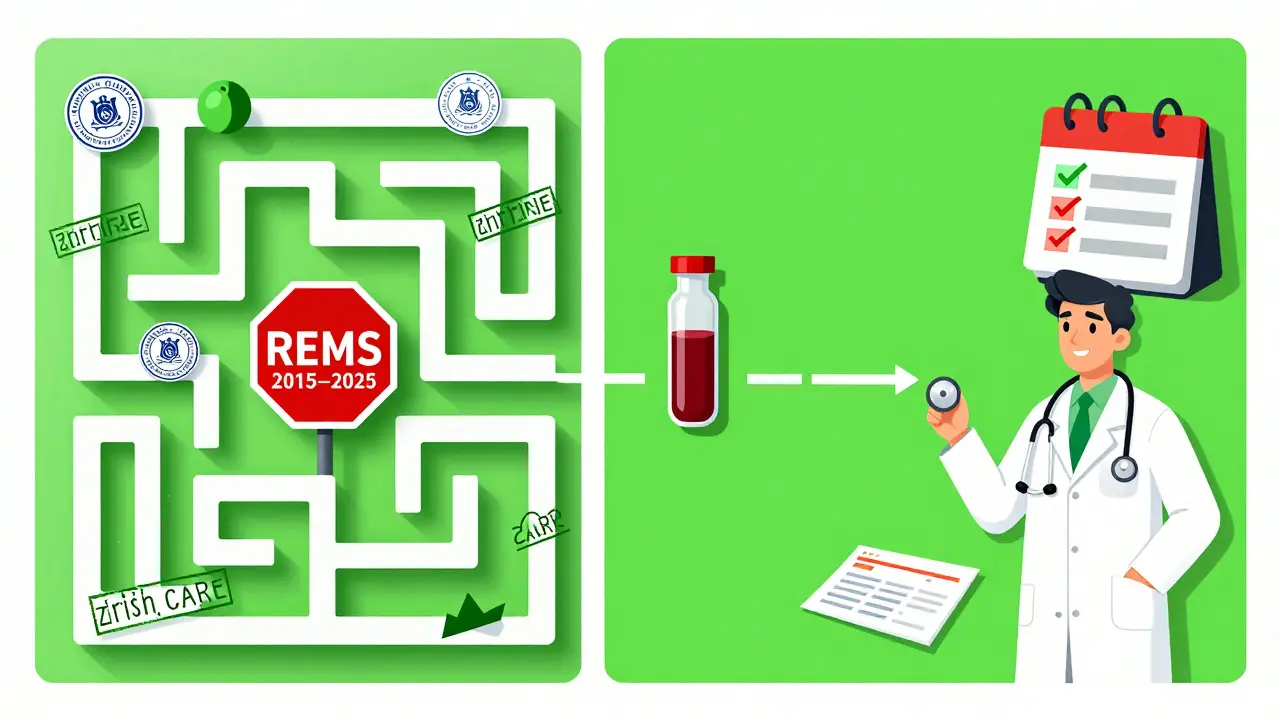
Before February 24, 2025, getting clozapine wasn’t just about a prescription. It was a paperwork marathon. Patients had to jump through hoops: weekly blood tests, monthly forms, certified doctors, certified pharmacies, and endless phone calls just to get their meds. For people with treatment-resistant schizophrenia, clozapine was often the only thing that worked-but the system made it harder to access than it needed to be.
What Was the Clozapine REMS Program?
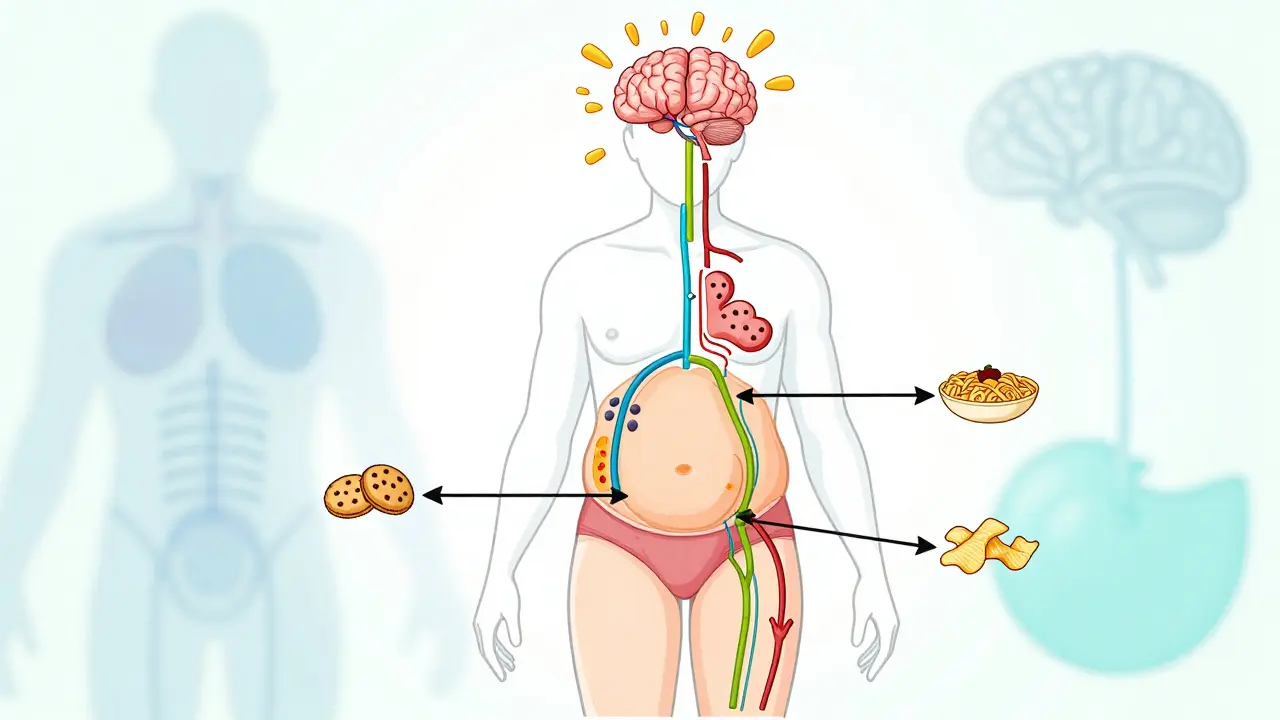
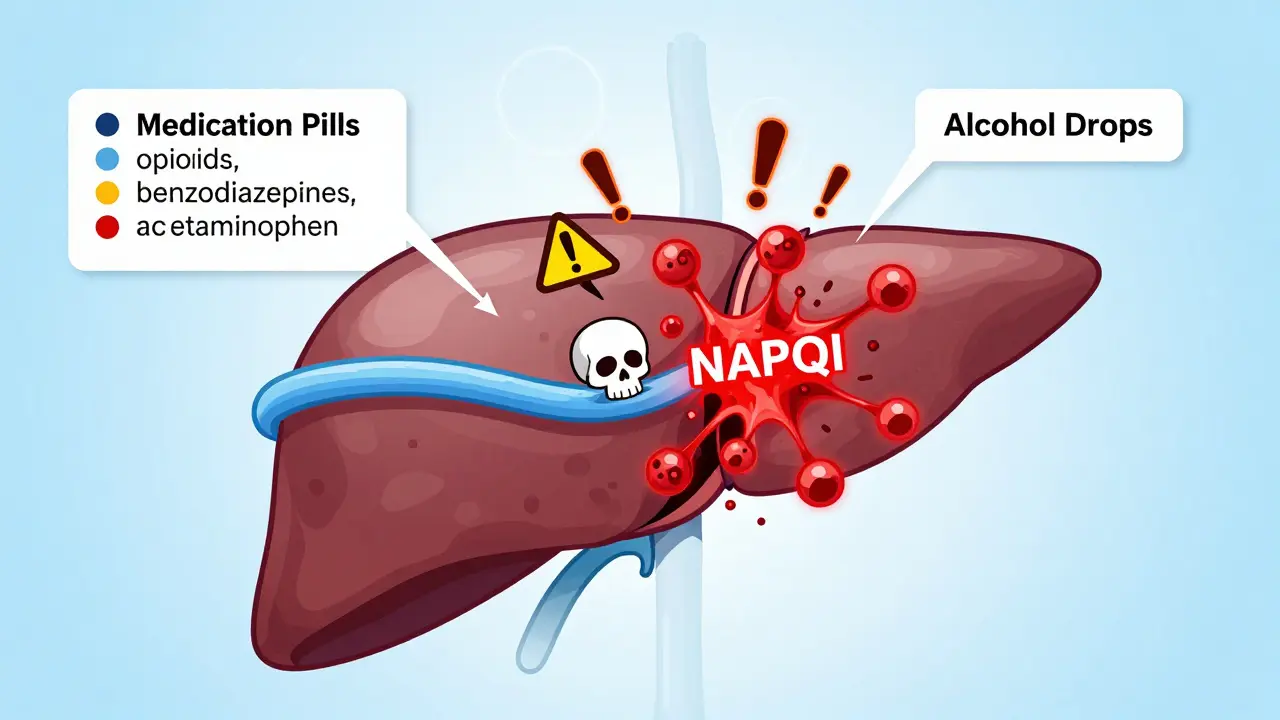
The Clozapine Risk Evaluation and Mitigation Strategy (REMS) was a federal safety program created by the FDA in 2015. Its goal? Prevent life-threatening drops in white blood cells-specifically, severe neutropenia and agranulocytosis. These conditions can leave the body defenseless against infections. Clozapine is incredibly effective for schizophrenia when other drugs fail, but it carries this serious risk, especially in the first six months.
Under the old REMS rules, every step of the process was locked down. Prescribers had to be certified. Pharmacies had to be certified. Patients had to enroll. Every time a patient needed a refill, the pharmacy had to confirm that their Absolute Neutrophil Count (ANC) was above a certain level-1,500/μL for most people, 1,000/μL for those with benign ethnic neutropenia. And they couldn’t just call in the result. They had to log into a federal portal, submit a form, and wait for approval before filling the script.
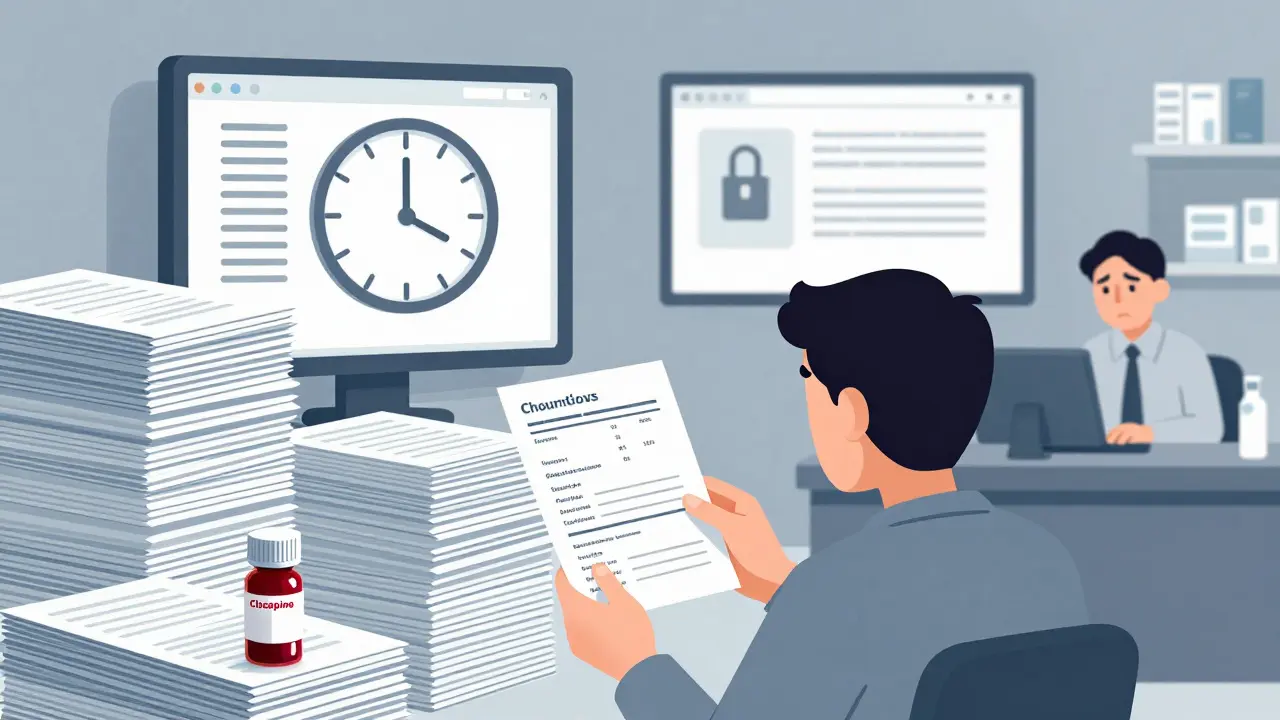
That meant delays. Some patients waited days. Others gave up. Clinics spent hours each week just managing REMS paperwork. One survey found clinics spent an average of 3.2 hours per week on REMS tasks alone. For a medication that could mean the difference between hospitalization and stability, that was unacceptable.
The Big Change: REMS Was Removed in February 2025
On February 24, 2025, the FDA officially ended the mandatory Clozapine REMS program. No more certified prescribers. No more certified pharmacies. No more monthly Patient Status Forms. No more waiting for portal approval.
This wasn’t a sign that the risk disappeared. It was a sign that the system had outlived its purpose.
The FDA spent over a year reviewing real-world data from the Sentinel System, the Department of Veterans Affairs, and Brigham and Women’s Hospital. What they found was clear: doctors and pharmacists were already monitoring ANC levels properly-even without being forced to. Studies showed that 92% of patients on clozapine were getting their blood tests on schedule. The risk of severe neutropenia hadn’t gone up. The death rate hadn’t changed. The system wasn’t saving lives-it was just slowing them down.
The FDA concluded: the medical community had learned. The guidelines were understood. The monitoring was happening. So they removed the bureaucracy.
ANC Monitoring Is Still Required-Just Not by the Government
Let’s be clear: you still need your ANC checked. The FDA didn’t say stop monitoring. They said stop forcing you to report it.
Here’s what the current guidelines say:
- Before starting clozapine: Get a baseline ANC test.
- Weeks 1-18: Weekly blood tests. This is when the risk is highest.
- Weeks 19-52: Every two weeks if ANC is normal.
- After 12 months: Monthly, unless your doctor says otherwise.
These aren’t suggestions. They’re the standard of care. The FDA still requires the Boxed Warning on every clozapine label. The prescribing information from Novartis hasn’t changed. The risk is real. But now, you don’t have to submit your results to a federal database. Your doctor keeps the records in your chart. Your pharmacy just fills the prescription.

Why This Matters for Patients
Before 2025, 30% of patients who needed clozapine couldn’t get it on time because of REMS delays. One woman in Ohio told her support group she waited 11 days for a refill because the pharmacy couldn’t verify her ANC. Her symptoms returned. She ended up in the ER.
Now, that won’t happen as often. Pharmacies no longer spend 10-15 minutes per prescription on REMS checks. Prescribers don’t have to re-certify every two years. Patients don’t have to fill out forms they don’t understand.
And it’s working. Since the change, clinics in rural areas report a 40% increase in clozapine starts. Insurance companies like Anthem project a 25-30% rise in new prescriptions over the next two years. That’s thousands of people who will finally get the drug that works for them.
What About the Risks?
Yes, clozapine can still cause agranulocytosis. About 0.8% of patients develop severe neutropenia, mostly in the first six months. But that risk hasn’t changed. The monitoring hasn’t changed. Only the red tape has.
Doctors still check ANC levels. Labs still report results. Patients still get warned. The difference? Now, the decision to monitor is based on clinical judgment-not federal compliance.
Some experts worried this might lead to gaps. But the data says otherwise. The VA, which treated over 12,000 clozapine patients before and after REMS removal, saw no increase in missed tests. In fact, adherence improved slightly-probably because patients trusted their doctors more when the system felt less robotic.
What Should You Do Now?
If you’re taking clozapine:
- Keep getting your ANC tested on schedule. Don’t skip because the form is gone.
- Ask your doctor if you’re still following the right timeline.
- Make sure your pharmacy knows the REMS is gone. Some may still be using old procedures.
If you’re starting clozapine:
- Ask your psychiatrist to explain the ANC schedule.
- Find a pharmacy that’s familiar with clozapine. Not all are.
- Don’t wait for a form. Bring your lab results to your appointment.
If you’re a provider:
- Update your protocols. Remove REMS references from your templates.
- Use the FDA-approved prescribing information (2017, still current).
- Educate your staff. Many are still trained on the old system.
What’s Next?
The American Society of Health-System Pharmacists is rolling out updated guidelines in Q3 2025 to help clinics adjust. The FDA will keep watching through the Sentinel System. If neutropenia rates start to climb, they’ll step back in.
But for now, the message is clear: trust the science, not the system.
Clozapine is still the most effective antipsychotic for treatment-resistant schizophrenia. Meta-analyses show it works for 30-50% of patients who didn’t respond to anything else. Before, only 12% of eligible patients got it. Now, that number is rising. And that’s not just policy change-it’s a lifeline restored.
Frequently Asked Questions
Is clozapine still dangerous?
Yes, clozapine can cause severe neutropenia or agranulocytosis, especially in the first six months. The risk hasn’t gone away. But the FDA’s decision to remove the REMS program was based on evidence that doctors are already monitoring patients safely without mandatory reporting. The Boxed Warning remains on all clozapine labels.
Do I still need blood tests for clozapine?
Yes. ANC monitoring is still medically required. The schedule is: weekly for the first 18 weeks, every two weeks from 6 to 12 months, and monthly after that. Your doctor will tell you the exact plan. Just because the government no longer requires you to report results doesn’t mean the medical need has changed.
Can any pharmacy fill my clozapine prescription now?
Yes. Pharmacies no longer need to be certified under the REMS program. But not all pharmacies are familiar with clozapine’s monitoring needs. If your pharmacy seems unsure, ask them to check the current prescribing information from Novartis. You can also switch to a pharmacy that regularly handles clozapine prescriptions.
What if my doctor stops checking my ANC?
If your doctor stops monitoring your ANC, speak up. The FDA removed the mandatory reporting system, not the medical standard of care. You have the right to expect regular blood tests. If your provider refuses, ask for a referral to a psychiatrist or specialist who follows current clozapine guidelines.
Why did the FDA remove REMS if the risk is still there?
Because the system wasn’t working as intended. The FDA found that doctors and pharmacists were already monitoring patients properly-without the REMS bureaucracy. The program created delays, reduced access, and added administrative burden without improving safety. Removing it was about trusting clinical judgment, not ignoring risk.
Will clozapine become easier to get now?
Yes. Since the REMS removal, clinics report faster starts and fewer abandoned prescriptions. Experts predict a 25-30% increase in clozapine use over the next two years. For patients with treatment-resistant schizophrenia, this means more people will get the most effective treatment available.


9 Comments