Antidepressant Safety Calculator for Breastfeeding Mothers
Antidepressant Safety Assessment
Select an antidepressant to see safety information for breastfeeding mothers
Safety Information
Relative Infant Dose (RID):
Safety Rating:
Key Considerations
Potential Side Effects in Infants
Understanding Postpartum Depression
1 in 8 new mothers experience postpartum depression. It's not just the 'baby blues'-it's a serious condition that can last months or longer. Symptoms include overwhelming sadness, anxiety, loss of interest in activities, and trouble bonding with your baby. Left untreated, it can affect your ability to care for yourself and your child. The CDC reports that about 1 in 8 women develop PPD within the first year after giving birth. The postpartum depression treatment process must balance maternal health and infant safety.
How Antidepressants Pass into Breast Milk
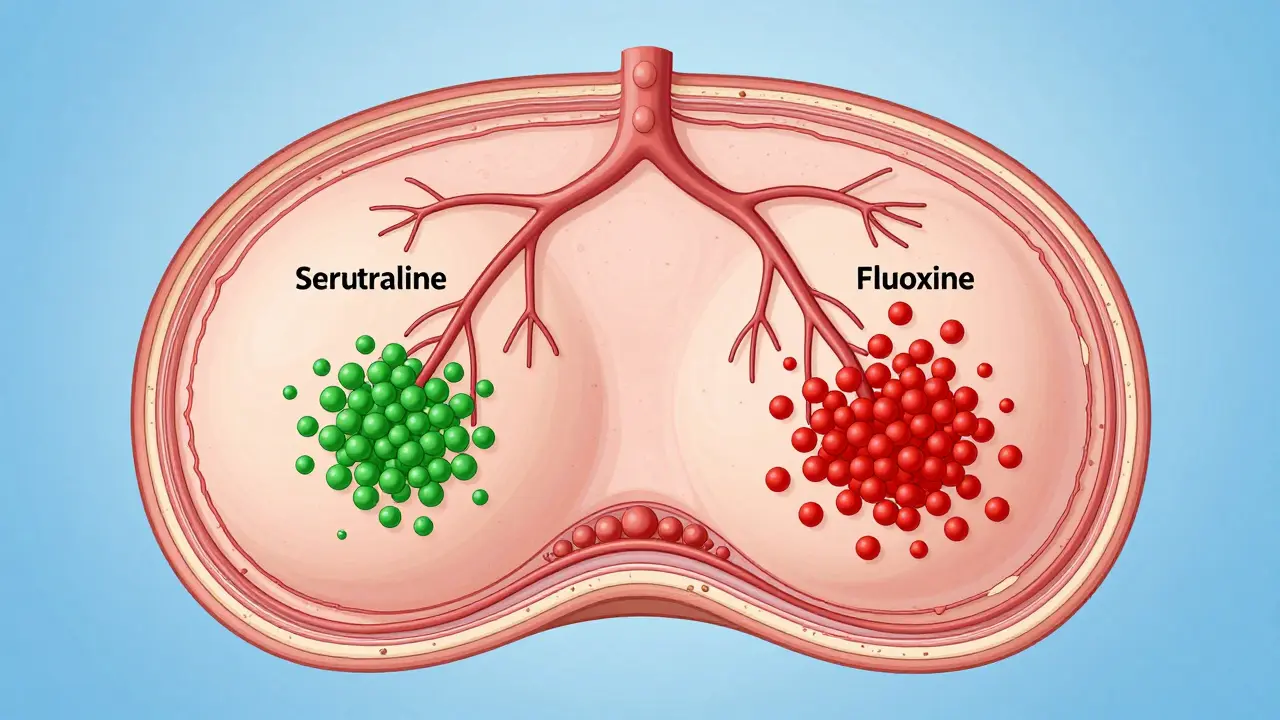
When you take antidepressants, some of the medication passes into breast milk. Scientists measure this using 'relative infant dose' (RID), which calculates how much of the mother's dose the baby receives through milk. Any RID below 10% is generally safe. For example, sertraline has an RID of just 0.5-3.2%, while fluoxetine can reach 5.9-15.2%. This difference matters because higher RID means more medication in your baby's system.
The InfantRisk Center explains that the baby's age and health also affect risk. Premature infants or those under two months may be more sensitive to medication exposure. Always discuss your specific situation with your doctor before starting treatment.
Which Antidepressants Are Safest for Breastfeeding?
| Antidepressant | Transfer Rate to Breast Milk | Safety Rating | Key Considerations |
|---|---|---|---|
| sertraline | 0.5-3.2% | First-line | Lowest transfer rate; undetectable in 92% of infant blood tests |
| paroxetine | 0.9-8.6% | First-line | Low transfer, but may cause withdrawal symptoms in newborns if used late in pregnancy |
| citalopram | 3.5-8.9% | Moderate | Potential QT interval prolongation at higher doses |
| fluoxetine | 5.9-15.2% | Higher risk | Accumulates in infant serum; may cause irritability or feeding issues |
| zuranolone | 0.5-1.5% | New treatment | First oral PPD-specific drug; current guidelines recommend pumping and discarding milk for 1 week after treatment |
A 2022 meta-analysis of 27 studies involving 1,845 mother-infant pairs found no significant adverse effects in breastfed infants with maternal sertraline use. Infant serum levels were undetectable in 92% of cases. Paroxetine follows closely with similar low transfer rates. Meanwhile, fluoxetine's long half-life causes buildup in infant blood, with some studies showing levels up to 30% of maternal concentrations after prolonged use.
Real-World Experiences from Mothers
A 2021 survey of 347 lactating women with PPD published in Archives of Women's Mental Health found 78% continued breastfeeding while taking antidepressants. Of these, 86% reported 'no noticeable effects' on their infants. However, 12% noticed side effects like increased fussiness (6.3%), sleep disturbances (4.1%), or feeding difficulties (1.6%).
On Postpartum Support International's online forum, a thread titled 'Sertraline while breastfeeding' with 1,247 comments (as of September 2023) shows 68% positive experiences, 22% reporting mild effects that resolved with dose adjustments, and 10% describing significant issues leading to medication changes. One mother shared: 'My daughter developed explosive diarrhea that stopped immediately when I switched from fluoxetine to sertraline.' Another wrote: 'Sertraline gave me my life back without harming my breastfeeding relationship.'

Practical Steps for Safe Treatment
When starting antidepressants, follow these steps:
- Start with the lowest effective dose of sertraline (25-50mg daily) or paroxetine (10-20mg daily)
- Take medication immediately after breastfeeding to maximize the time before the next feeding
- Monitor your baby for sedation, poor feeding, or irritability during the first 2-4 weeks
- Use the Edinburgh Postpartum Depression Scale (EPDS) at 1, 2, 4, and 6 months to track symptoms
The Cleveland Clinic advises waiting at least three to four weeks before assessing medication effectiveness. Abruptly stopping antidepressants increases relapse risk threefold. Resources like LactMed (updated weekly by the National Library of Medicine) provide real-time data on over 1,300 medications. The InfantRisk Center hotline (806-352-2519) fields about 3,000 lactation medication inquiries monthly.
Newer Treatments and Future Research
zuranolone (Zurzuvae), approved by the FDA in August 2023 as the first oral treatment specifically for PPD, shows promise. Clinical trials found 50% of participants achieved remission within 15 days compared to 30% on placebo. However, current guidelines from the American College of Obstetricians and Gynecologists recommend 'pumping and discarding milk for 1 week after treatment' due to limited data.
Ongoing research includes the B.R.I.D.G.E. study (NCT04907789), tracking infant neurodevelopment in 500 mothers taking SSRIs during lactation. Preliminary data is expected in late 2024. The NIH has allocated $4.7 million for 2023-2025 to study how antidepressants affect the infant gut microbiome. A 2022 JAMA Pediatrics study found infants with CYP2D6 poor metabolizer status had 3.2-fold higher serum concentrations of venlafaxine when exposed through breast milk, suggesting future personalized treatment options.
Is it safe to breastfeed while taking antidepressants?
Yes, for most antidepressants. Major health organizations like the CDC and ACOG state that the benefits of treating maternal depression usually outweigh any potential risks from medication in breast milk. Sertraline and paroxetine are considered safest, with very low transfer rates. Untreated depression poses greater risks to both mother and baby.
Which antidepressants are safest for breastfeeding mothers?
Sertraline and paroxetine are first-line options. Sertraline has the lowest transfer rate (0.5-3.2%) and undetectable levels in 92% of infant blood tests. Paroxetine follows closely with low transfer (0.9-8.6%). Avoid fluoxetine and doxepin due to higher transfer rates and documented side effects like irritability or apnea in infants.
What are the signs of antidepressant side effects in breastfed infants?
Watch for excessive sleepiness, poor feeding, irritability, or unusual crying. Some infants may develop gastrointestinal issues like gas or diarrhea. If you notice these symptoms, contact your pediatrician immediately. Most side effects resolve with dose adjustments or switching medications.
How long does it take for antidepressants to work during postpartum depression?
It usually takes 3-4 weeks to see improvement. The Cleveland Clinic emphasizes not stopping medication prematurely-abrupt discontinuation increases relapse risk threefold. Consistent use is key, even if symptoms improve before the full four weeks.
Can I stop breastfeeding if I need to take antidepressants?
Stopping breastfeeding is rarely necessary. Most antidepressants are safe to use while nursing. The American Academy of Pediatrics and CDC both state that breastfeeding is generally compatible with antidepressant treatment. If you're concerned, work with your doctor to choose the safest medication and monitor your baby closely.