What Is Post-Concussion Syndrome?
Post-Concussion Syndrome (PCS) isn’t just a lingering headache after a bump to the head. It’s when symptoms from a mild traumatic brain injury - like dizziness, brain fog, trouble sleeping, or irritability - refuse to go away long after the injury should’ve healed. Most people bounce back from a concussion in a few days or weeks. But for 15-30% of them, symptoms stick around past three months. That’s when doctors diagnose PCS.
The brain doesn’t show structural damage on an MRI or CT scan. That’s why it’s easy to dismiss. But the problem isn’t broken tissue - it’s broken function. Even after metabolic recovery (which usually finishes within 22 to 30 days), the brain keeps using inefficient pathways to do simple tasks. Think of it like a computer running old software after a system update. It still works, but slowly, glitchy, and exhausting.
How Long Does Recovery Actually Take?
There’s no one-size-fits-all timeline. For most people - about 70 to 80% - symptoms fade within four weeks, especially if they start gentle movement and activity early. About 60% feel better within just 5 to 7 days. But for others, recovery stretches into months, sometimes years.
Research shows that if symptoms haven’t improved by three months, you’re in the PCS range. Some studies even suggest that if there’s no meaningful progress after three years, symptoms may become long-term. That doesn’t mean they’re permanent for everyone - but it does mean the brain needs more targeted help.
Age matters. Kids and older adults recover slower. People who’ve had prior concussions are at higher risk for prolonged symptoms. Athletes who wait two or three weeks to see a specialist take 20 days longer to recover than those treated within the first week.
What Symptoms Should You Watch For?
PCS doesn’t come with one symptom. It’s a mix - physical, mental, emotional, and sleep-related. Common signs include:
- Headaches or pressure in the head
- Dizziness or balance issues
- Blurry vision or light sensitivity
- Trouble concentrating or remembering things
- Feeling overwhelmed, anxious, or irritable
- Insomnia or sleeping too much
- Noise sensitivity
- Fatigue that doesn’t go away with rest
These symptoms don’t always show up right away. Many people feel fine for the first few days, then crash around day 5 to 10. That’s normal. It’s not a relapse - it’s the brain revealing its true recovery status.
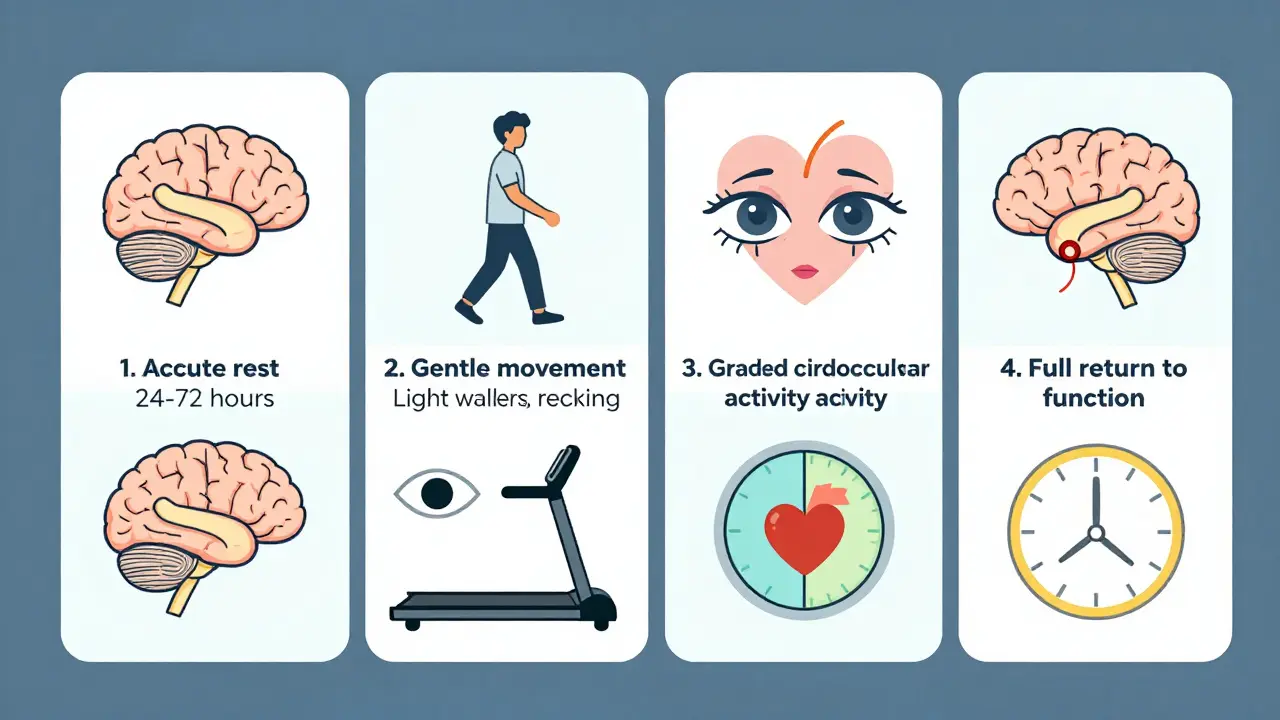
Why Rest Alone Doesn’t Work Anymore
For years, the advice was simple: lie down, avoid screens, stay quiet. But that approach often made things worse. Studies now show that strict rest beyond 24 to 72 hours delays recovery. Why? Your brain needs stimulation - the right kind.
Think of your brain like a muscle. After a sprain, you don’t keep it in a cast forever. You gently move it. The same applies here. Active rehabilitation - carefully graded physical and cognitive activity - triggers healing pathways. A 2023 study from Complete Concussions found that athletes who started light exercise within the first week recovered 20 days faster than those who waited.
Rest is still important in the first 48 hours. But after that, the goal shifts to controlled, symptom-limited activity. Sitting still too long can make your nervous system hypersensitive, worsening dizziness, headaches, and anxiety.
How Is PCS Managed Today?
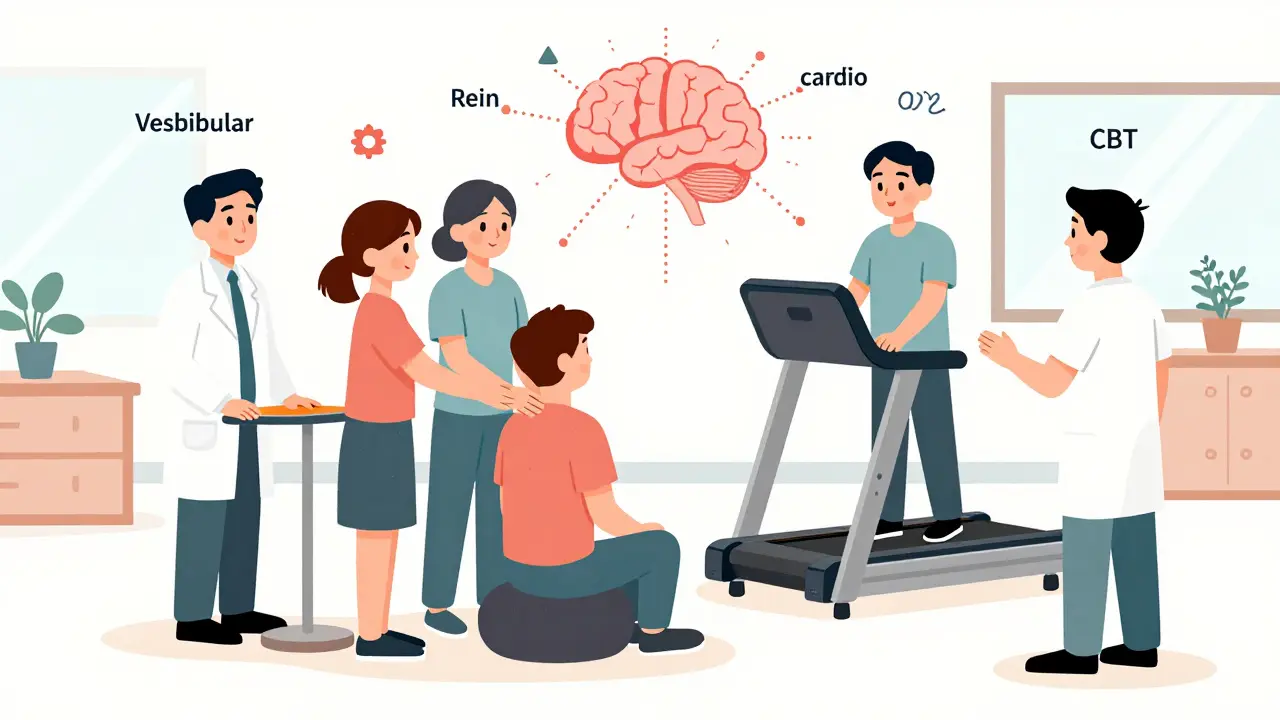
Modern PCS management is multidisciplinary. No single treatment fixes everything. Instead, experts target specific systems:
- Vestibular therapy - for dizziness and balance problems. This involves eye-head coordination exercises and controlled movement.
- Cervical therapy - neck injuries often accompany concussions. Tight muscles or misalignments can trigger headaches and dizziness.
- Vision therapy - if reading or screen use causes strain, eye-tracking and focusing drills help.
- Cardiovascular rehab - a graded treadmill program slowly rebuilds tolerance. The goal? To reach 85-90% of your max heart rate without symptoms.
- Cognitive behavioral therapy (CBT) - helps manage anxiety, sleep issues, and the emotional toll of chronic symptoms.
Some clinics use advanced tools like functional Neurocognitive Imaging (fNCI) to map blood flow in the brain. This helps pinpoint which areas are underperforming. Treatment then targets those exact regions. One study showed patients improved by 75% on symptom severity scores after just four days of this targeted therapy.
When Is It Safe to Return to Normal Life?
Recovery isn’t just about feeling better. It’s about function. Experts use clear benchmarks:
- Post-Concussion Symptom Scale (PCSS) score under 5 for men, under 6 for women
- No abnormal findings on neurological exams
- Ability to exercise at 85-90% of max heart rate without symptoms
- Returning to work, school, or daily tasks without mental fatigue or headaches
The CDC recommends returning to regular activities as soon as symptoms are mild and nearly gone. You don’t need to be 100% symptom-free to start. But you need to avoid anything that makes symptoms spike.
For athletes, the return-to-play process is staged: light aerobic exercise → sport-specific drills → non-contact training → full contact → game play. Rushing this can lead to re-injury and longer setbacks.
What Factors Make Recovery Harder?
Not everyone who gets a concussion ends up with PCS. Certain factors increase risk:
- History of prior concussions - each one raises the risk of longer recovery
- Severe symptoms in the first 24 hours - a 20-point jump on the Graded Symptom Checklist predicts longer recovery
- Loss of consciousness or memory loss around the time of injury
- On-field dizziness - one study found this increased the chance of recovery taking more than 21 days by 6.3 times
- Pre-existing mental health conditions like anxiety or depression
- Waiting too long to get evaluated - delays beyond two weeks make recovery longer
If you’re a parent, coach, or teacher, watch for changes in behavior. Kids might become more tearful, act out in school, or avoid socializing. These aren’t just mood swings - they could be signs of an unresolved brain injury.
What’s the Long-Term Outlook?
The good news? Most people with PCS do recover. Even those who struggle for months often see steady improvement with the right care. The Cleveland Clinic reports a generally positive prognosis - symptoms usually resolve, even if it takes a year.
But recovery isn’t always linear. You might have two good weeks, then a bad day. That’s normal. It doesn’t mean you’re backtracking. It means your brain is still adjusting.
Some studies suggest that if recovery hasn’t occurred by three years, symptoms may become persistent. But even then, many people learn to manage them well. The goal isn’t always to erase every symptom - it’s to rebuild function and quality of life.
What’s New in Research?
Science is catching up. The CONCERN study, launched in 2021 by the University of Pittsburgh, is tracking 1,200 concussion patients over five years to find biomarkers that predict who will develop PCS. That could lead to early interventions before symptoms become chronic.
Researchers are also exploring how inflammation, autonomic nervous system dysregulation, and blood flow changes contribute to PCS. The focus is shifting from “rest and wait” to “activate and repair.”
One key insight: PCS isn’t in your head - it’s in your brain’s wiring. And with the right tools, that wiring can be rewired.







12 Comments