If you’ve been told you need a polysomnography test, you’re probably wondering what it’s really like. Is it scary? Do you have to sleep with wires all over you? Will you even be able to fall asleep? The truth is, most people are surprised by how manageable it is-and how much it can reveal about their sleep.
What Exactly Is Polysomnography?
Polysomnography, often called a sleep study, is the most detailed way doctors check what’s happening in your body while you sleep. It’s not just about breathing-it tracks your brain waves, eye movements, heart rate, muscle activity, oxygen levels, and even how you move during the night. The word itself breaks down to "many" (poly), "sleep" (somno), and "recording" (graphy). That’s because it records at least seven different signals at once.
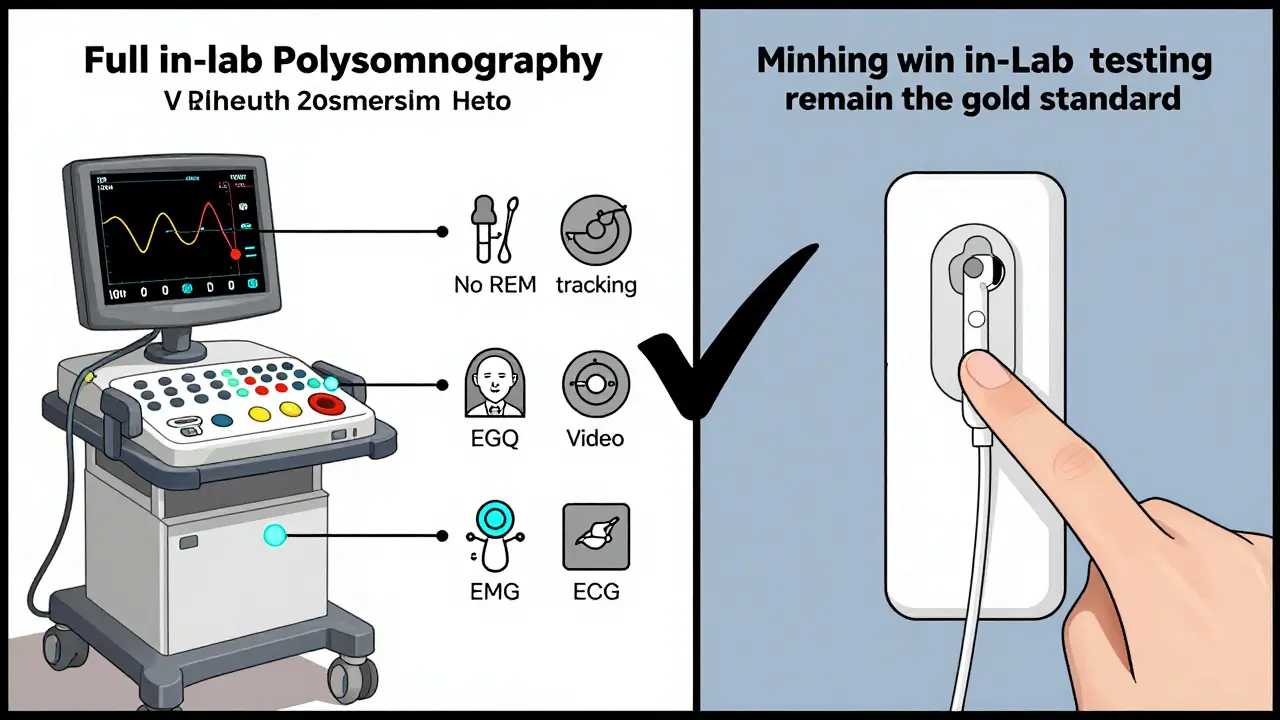
This isn’t a simple home test. Unlike those portable devices you can rent, which only measure airflow and oxygen, polysomnography gives a full picture of your sleep architecture. That means it can tell if you’re getting deep sleep, REM sleep, and whether your body is cycling through stages the way it should. It’s the only test that can diagnose conditions like narcolepsy, sleepwalking, night terrors, and different types of sleep apnea-not just snoring.
What Gets Monitored During the Study?
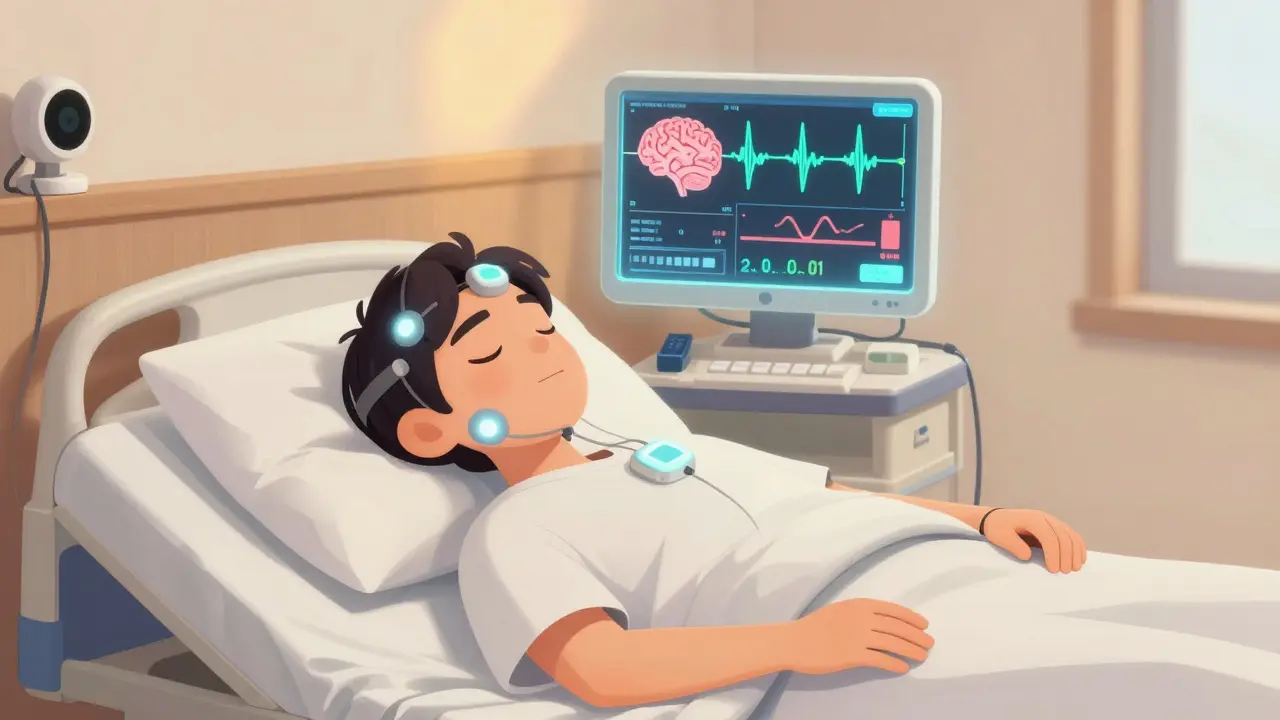
You’ll be connected to about 20 sensors, but don’t panic-they’re not needles or invasive. Most are sticky patches or soft belts. Here’s what each one does:
- EEG (electroencephalogram): Electrodes on your scalp track brain activity to determine sleep stages-light sleep, deep sleep, and REM.
- EOG (electrooculogram): Sensors near your eyes detect rapid eye movements, which signal when you’re dreaming (REM sleep).
- EMG (electromyogram): Small sensors on your chin and legs measure muscle tone. This helps spot leg jerks or unusual movements like sleepwalking.
- ECG (electrocardiogram): A few leads on your chest monitor your heart rhythm. Irregular beats during sleep can point to underlying issues.
- Respiratory belts: Two elastic bands around your chest and abdomen track how hard you’re trying to breathe.
- Nasal airflow sensor: A thin tube under your nose detects whether air is moving in and out.
- Pulse oximeter: A clip on your finger measures how much oxygen is in your blood. Drops below 90% are a red flag.
- Body position sensor: Tells technicians if you’re sleeping on your back, side, or stomach-important because sleep apnea often worsens on your back.
- Audio and video: A camera and microphone record snoring, gasping, or strange behaviors like sitting up or talking in your sleep.
All of this data is sent to a computer in another room, where a sleep technologist watches it in real time. They can talk to you through an intercom if you need to use the bathroom or if a sensor falls off. You’re never alone.
How Is the Test Done? Step by Step
Here’s what actually happens on the night of your test:
- You arrive at the sleep center 1-2 hours before your usual bedtime. Most centers are set up like hotel rooms-quiet, private, with a comfortable bed.
- A registered sleep technologist spends 30-45 minutes applying all the sensors. They’ll explain each one and make sure you’re comfortable.
- You’re encouraged to follow your normal routine: no caffeine after noon, no naps, no alcohol. This helps the results reflect your real sleep habits.
- You get into bed and turn off the lights. The technologist will monitor you from another room and may check in briefly to make sure everything’s working.
- You sleep normally. Most people do get enough sleep-even if it’s not perfect. The goal isn’t to sleep like you do at home; it’s to capture your natural sleep patterns under observation.
- The test runs for 6-8 hours, usually ending around 6 a.m. The sensors are removed quickly, and you’re free to go.
Some people worry they won’t sleep at all. It happens sometimes-but even if you only get 4 hours, it’s often enough for diagnosis. The technologist can tell if you had deep sleep, REM, or frequent awakenings, even if you don’t remember them.
What Do the Results Show?
After the test, a board-certified sleep doctor spends 2-3 hours analyzing the data. You’ll get a report with numbers like:
- Apnea-Hypopnea Index (AHI): How many times per hour your breathing stops (apnea) or gets shallow (hypopnea). Under 5 is normal. 5-15 is mild, 15-30 is moderate, over 30 is severe.
- Oxygen desaturation: How low your blood oxygen drops during breathing pauses. Drops below 88% are considered significant.
- Sleep efficiency: Percentage of time you were actually asleep vs. lying in bed. Below 85% may mean you’re struggling to stay asleep.
- REM latency: How long it takes to enter REM sleep. If you enter REM too quickly (under 15 minutes), it could point to narcolepsy.
- Leg movements: How often your legs jerk during sleep. More than 15 per hour may indicate restless legs syndrome.
These numbers don’t just say "you have sleep apnea." They help doctors tell the difference between obstructive sleep apnea (your airway collapses) and central sleep apnea (your brain stops telling your body to breathe). That’s critical because treatments are different.

Split-Night Studies: One Night, Two Purposes
If your first few hours show severe sleep apnea (AHI over 30), the study may switch to a "split-night" setup. That means the second half of the night is used to test CPAP therapy.
The technologist will fit you with a mask and slowly increase air pressure until your breathing stops are controlled. This saves you from coming back for a second test. About 35% of polysomnography studies today are split-night.
But if your apnea is mild or unclear, you’ll need a separate CPAP titration study later. The goal is always to find the lowest pressure that keeps your airway open without making you uncomfortable.
How Does It Compare to Home Sleep Tests?
Home sleep tests are cheaper and more convenient-but they’re not the same thing. They usually only measure:
- Heart rate
- Respiratory effort
- Airflow
- Oxygen levels
That’s it. No brain waves. No eye movements. No leg jerks. So if you have symptoms like daytime fatigue, sudden sleep attacks, or sleepwalking, a home test won’t catch it. Studies show home tests fail to produce usable data in 15-20% of cases. In-lab polysomnography fails less than 5% of the time.
Insurance companies often require an in-lab study if you have other health conditions like heart disease, COPD, or neurological issues. Home tests are usually only approved for otherwise healthy adults with clear signs of obstructive sleep apnea.
What Happens After the Results?
Your doctor will schedule a follow-up to explain the findings. If you have sleep apnea, treatment usually starts with CPAP. But not everyone needs it. Some people benefit from weight loss, positional therapy (sleeping on your side), or oral appliances. If you have narcolepsy, you might need medication. If you’re sleepwalking or having night terrors, behavioral strategies or safety changes in your bedroom may be recommended.
It’s not a one-size-fits-all. That’s why the full picture from polysomnography matters. A simple breathing test won’t tell you if your fatigue is from poor sleep quality, a neurological condition, or something else entirely.
Common Concerns-And the Truth
Here’s what patients often worry about-and what really happens:
- "Will I be able to sleep?" Most people do. Even if you’re awake more than usual, the data still works. Sleep techs are trained to help you relax.
- "Is it painful?" No. The sensors don’t poke or shock you. The only discomfort might be the mask if you’re not used to it.
- "What if I snore or talk in my sleep?" That’s normal. The video and audio help the doctor understand your symptoms.
- "What if I need to use the bathroom?" You can. The wires are designed to disconnect quickly. Just press a button, and the tech will help you.
Studies show over 90% of patients are satisfied with the experience-especially when they’re prepared. Most say knowing what to expect made all the difference.
Insurance and Cost
Medicare and most private insurers cover polysomnography if your doctor documents symptoms like loud snoring, witnessed breathing pauses, or excessive daytime sleepiness. You’ll likely need a referral from your primary care doctor or a sleep specialist.
Costs vary, but in-lab studies typically range from $1,500 to $3,000. Home tests cost $300-$800. Insurance usually pays 80% of the in-lab test if it’s deemed medically necessary. Always check with your provider before scheduling.
What’s Next for Sleep Studies?
Technology is improving. New wireless systems cut down the number of wires from 20 to just a few. Some labs now use AI to help analyze data faster and more accurately. But the core method hasn’t changed-and for good reason. Nothing else gives you the full story.
Researchers are working on at-home polysomnography with more sensors, but so far, nothing matches the reliability of an in-lab study for complex cases. For now, if you’re dealing with unexplained fatigue, loud snoring, or strange nighttime behaviors, a polysomnography study is still the gold standard.
Is polysomnography the same as a home sleep test?
No. A home sleep test only measures breathing, oxygen levels, and heart rate. Polysomnography records brain waves, eye movements, muscle activity, and more. It’s the only test that can diagnose narcolepsy, sleepwalking, or distinguish between types of sleep apnea.
Can I sleep normally with all those sensors?
Most people do. The sensors are soft and non-invasive. Even if you don’t sleep as well as you do at home, the data is still useful. Sleep technologists are trained to help you adjust, and many patients report they slept better than expected.
How long does it take to get results?
It usually takes 1-2 weeks. The raw data is over 1,000 pages, and a sleep specialist spends 2-3 hours analyzing it. You’ll have a follow-up appointment to discuss the findings and next steps.
What if I have sleep apnea-do I need to use CPAP forever?
Not always. Many people improve with weight loss, positional changes, or oral devices. CPAP is the most effective treatment, but it’s not the only option. Your doctor will help you find the right approach based on your results and lifestyle.
Can polysomnography detect other sleep disorders besides apnea?
Yes. It’s the only test that can diagnose narcolepsy, REM sleep behavior disorder, periodic limb movement disorder, night terrors, and sleepwalking. If your symptoms go beyond snoring or tiredness, a full sleep study is essential.
Is polysomnography covered by insurance?
Most insurers cover it if your doctor documents symptoms like witnessed breathing pauses, excessive daytime sleepiness, or loud snoring. Medicare typically pays 80% with a referral. Always check your plan’s requirements for prior authorization.
What to Do Next
If you’re still unsure whether you need a sleep study, start with your doctor. Write down your symptoms: Do you wake up gasping? Do you feel exhausted even after 8 hours? Does your partner say you stop breathing? These details matter.
Don’t ignore persistent fatigue. Sleep disorders don’t just make you tired-they raise your risk of high blood pressure, heart disease, and diabetes. A polysomnography study isn’t just about sleep. It’s about protecting your long-term health.





11 Comments