PAD Medication Selector
Personal Health Profile
Recommended Medication:
When you’re dealing with Peripheral artery disease (PAD), the first question is often, “Which drug actually helps my legs move without pain?” Pletal (cilostazol) pops up in many prescriptions, but it’s not the only player on the field. This guide walks you through the most common alternatives, weighs the pros and cons, and gives you a clear table to see which option fits your lifestyle and health profile.
Quick Takeaways
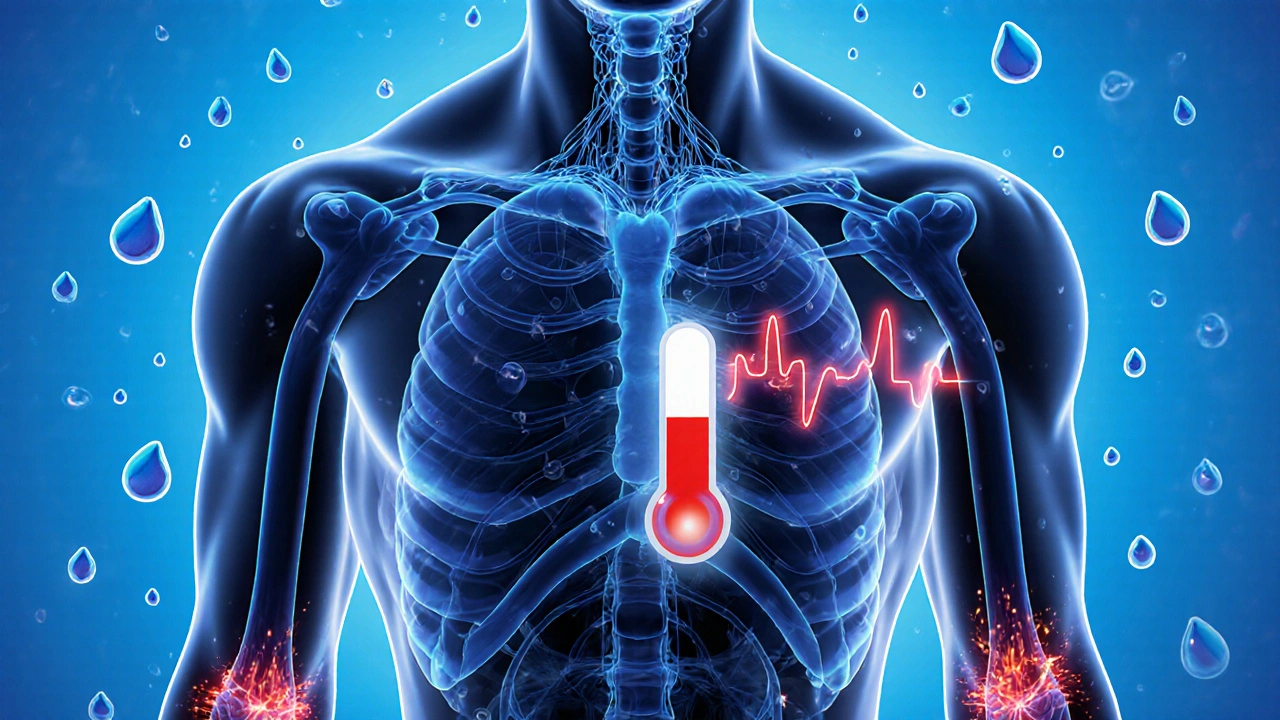
- Pletal improves walking distance by 30‑50% in most trials, but can cause headaches and palpitations.
- Pentoxifylline is milder on the heart but works slower; best for patients on anticoagulants.
- Naftidrofuryl targets blood‑vessel spasm and is useful when claudication worsens after meals.
- Alprostadil (prostacyclin) is a potent vasodilator for severe PAD, usually given by injection.
- Non‑drug options-exercise therapy, smoking cessation, and statins-are essential backbones for any regimen.
What Is Pletal (Cilostazol)?
Cilostazol is a phosphodiesterase‑3 inhibitor that increases cyclic AMP in blood‑vessel walls, leading to vasodilation and reduced platelet aggregation. Approved by the FDA in 1999, it’s marketed under the brand name Pletal for intermittent claudication, the cramping pain that forces many PAD patients to stop walking.
Typical dosing is 100mg twice daily, taken with food. The drug’s half‑life is about 11hours, so steady blood levels are maintained with the BID regimen.
Key Benefits and Risks of Pletal
- Benefit: Clinical trials (e.g., EUCLAIM, 2004) showed a 33% increase in maximum walking distance compared with placebo.
- Benefit: It also mildly improves lipid profiles, lowering LDL by ~5%.
- Risk: Headaches occur in up to 30% of users; these are usually transient.
- Risk: Palpitations, tachycardia, and rare cases of atrial fibrillation have been reported, so it’s contraindicated in patients with recent cardiac events.
- Risk: Not suitable for smokers who haven’t quit-studies show smoking negates 70% of the drug’s benefits.
Top Alternative Medications
Below are the most frequently prescribed alternatives, each with a short definition and the key attributes that matter when you compare them.
Pentoxifylline
Pentoxifylline is a xanthine‑derivative that improves red‑blood‑cell flexibility and reduces blood viscosity. It’s taken as 400mg twice daily.
- Walking distance gains: 15‑20% (modest).
- Side‑effects: nausea, dizziness, mild headaches.
- Best for: patients on blood‑thinners or with mild heart disease.
Naftidrofuryl
Naftidrofuryl is a peripheral vasodilator that relieves micro‑vascular spasm in the limbs. Dosed at 200mg three times daily.
- Walking distance gains: 20‑30% in post‑prandial claudication.
- Side‑effects: rare gastrointestinal upset.
- Best for: patients whose pain worsens after meals or who cannot tolerate cilostazol’s cardiac effects.
Alprostadil (Prostacyclin)
Alprostadil is a synthetic prostaglandinI₂ that causes strong vasodilation and inhibits platelet aggregation. Administered by subcutaneous injection, usually 20‑40µg daily.
- Walking distance gains: 40‑60% in severe PAD.
- Side‑effects: injection site pain, hypotension.
- Best for: patients with advanced disease who have failed oral therapy.
Non‑Drug Cornerstones
Even the best medication can’t replace lifestyle changes. The three pillars that work side‑by‑side with any drug are:
- Exercise therapy - supervised walking programs improve walking distance by 50‑80% on their own.
- Smoking cessation - eliminates the major risk factor; quitters see a 30% reduction in disease progression.
- Statins - lower LDL and stabilize plaques, indirectly supporting any PAD medication.
Side‑by‑Side Comparison Table
| Medication | Mechanism | Typical Dose | Walking‑Distance ↑ | Major Contra‑indications | Common Side‑effects |
|---|---|---|---|---|---|
| Pletal (Cilostazol) | Phosphodiesterase‑3 inhibition → vasodilation & anti‑platelet | 100mg BID | 30‑50% | Recent MI, unstable angina, uncontrolled arrhythmia | Headache, palpitations, diarrhea |
| Pentoxifylline | Decreases blood viscosity, improves RBC flexibility | 400mg BID | 15‑20% | Severe renal impairment | Nausea, dizziness |
| Naftidrofuryl | Peripheral vasodilator targeting micro‑spasm | 200mg TID | 20‑30% (post‑meal) | Severe liver disease | GI upset |
| Alprostadil | Prostacyclin analog → strong vasodilation | 20‑40µg SC daily | 40‑60% (severe PAD) | Bleeding disorders, hypotension | Injection pain, flushing |
How to Choose the Right Option for You
- Assess cardiovascular safety. If you’ve had a heart attack in the past year, avoid Pletal and consider Pentoxifylline or Naftidrofuryl.
- Consider disease severity. Mild to moderate claudication often responds to Pletal or Pentoxifylline; advanced cases may need Alprostadil.
- Check for drug interactions. Cilostazol is metabolized by CYP3A4; avoid strong inhibitors like ketoconazole. Pentoxifylline has fewer interactions.
- Evaluate tolerance. If headaches are a deal‑breaker, start with Naftidrofuryl.
- Don’t forget lifestyle. Pair any medication with at least 30‑minutes of walking, 5days a week, and quit smoking.
Talk with your vascular specialist about your exact risk profile. Many clinicians start with Pletal because of its strong evidence base, then switch or add another agent if side‑effects arise.
Frequently Asked Questions
Can I take Pletal and a statin together?
Yes. Statins work on cholesterol pathways, while cilostazol targets blood‑vessel tone. The combo is common and safe for most patients.
What if I’m a smoker? Should I still start Pletal?
Smoking cuts the effectiveness of Pletal by up to 70%. It’s better to quit first; many doctors will hold off on prescribing until you’ve been smoke‑free for at least a month.
Is there a generic version of cilostazol?
Yes, several manufacturers sell generic cilostazol, which usually costs 30‑40% less than the branded Pletal.
Can I switch from Pletal to Pentoxifylline without a wash‑out period?
Because cilostazol has a short half‑life, most clinicians advise a 24‑hour gap before starting Pentoxifylline, just to avoid overlapping side‑effects.
Which option is safest for someone on blood thinners?
Pentoxifylline is generally considered the safest, as it has minimal anti‑platelet activity compared with cilostazol or Alprostadil.

Next Steps
1. Review your cardiovascular history and current meds.
2. Schedule a brief appointment with your vascular doctor to discuss the comparison table.
3. If you start a medication, set a 4‑week checkpoint to evaluate walking distance and side‑effects.
4. Add a structured walking program and quit smoking if needed - the gains from lifestyle can double the drug’s effect.
With the right mix of medicine and habit, many PAD patients reclaim a pain‑free stroll around the park. Use this guide as your roadmap, and let your clinician fine‑tune the plan for your unique case.





12 Comments