When panic hits, you don’t need to wait for it to pass-you can act.
A panic attack doesn’t come with a warning. One moment you’re fine, the next your heart is pounding, your chest feels tight, and your mind screams that something’s terribly wrong. You might feel dizzy, numb, or like you’re losing control. It’s terrifying-but it’s not dangerous. And you don’t have to ride it out alone. A clear, simple action plan can help you stop the spiral before it takes over.
What works isn’t magic. It’s science. Decades of research show that combining breathing, grounding, and-when needed-medication gives you the best chance to regain control. Not everyone needs all three, but knowing how to use each one means you’re never unprepared.
Stop the hyperventilation: Breathing that actually works
When panic strikes, your breathing changes. It gets shallow, fast, and uneven. You’re not getting enough oxygen to your brain-not because you’re suffocating, but because you’re blowing off too much carbon dioxide. That drop in CO₂ triggers dizziness, tingling, chest pain, and that awful feeling you’re about to die. The fix? Slow, controlled breathing.
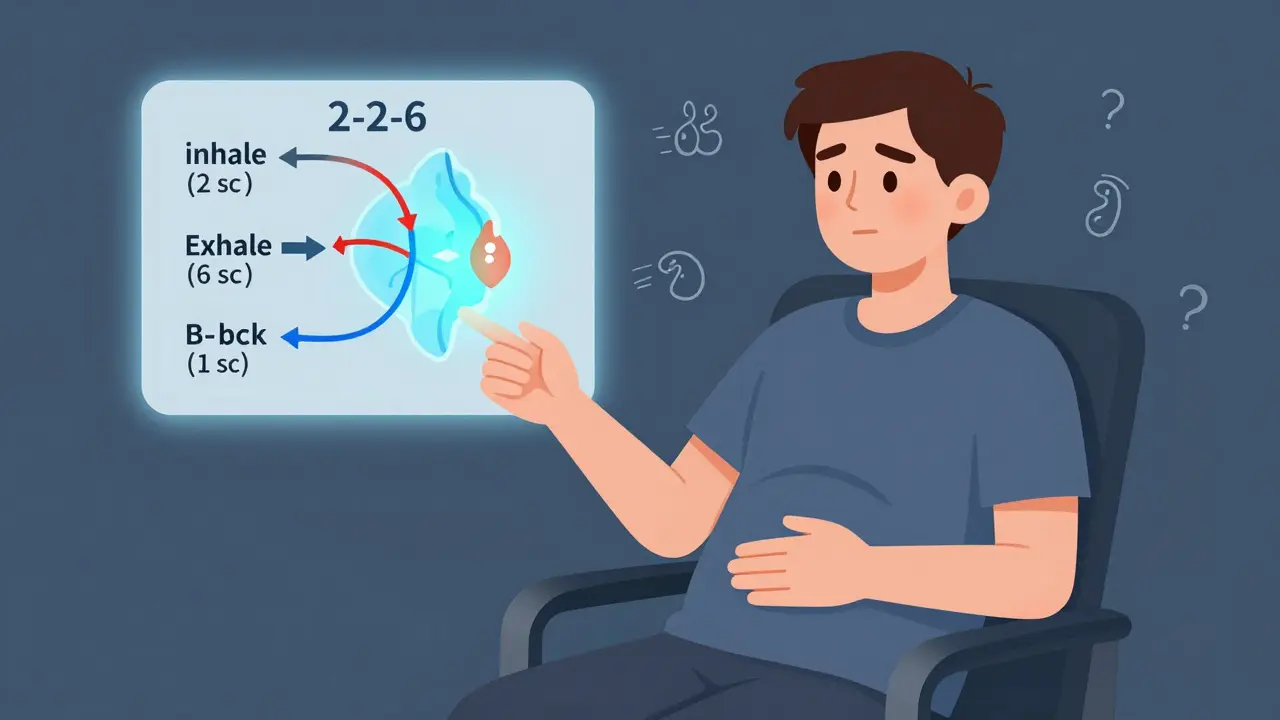
The 2-2-6 method is one of the most effective and easiest to remember. Inhale through your nose for two seconds. Hold for two seconds. Exhale slowly through your nose for six seconds. Then pause for one second before starting again. Do this for just 90 seconds. That’s all it takes to reset your nervous system.
Why this works: Long exhales activate your parasympathetic nervous system-the part that says “calm down.” Studies show people who practiced this daily for eight weeks cut their panic attacks by nearly half. You don’t wait until you’re in the middle of an attack to learn it. Practice it while brushing your teeth, sitting in traffic, or waiting in line. Make it automatic.
Another option: diaphragmatic breathing. Place one hand on your belly. Breathe in through your nose so your belly rises, not your chest. Exhale slowly through your mouth. Feel your hand sink as you breathe out. Do this for five minutes a day. It’s not just for emergencies-it rewires your body’s stress response over time.
Bring yourself back to the room: Grounding techniques that cut through the fear
Panic pulls you into your thoughts. You’re trapped in a loop: “I’m having a heart attack,” “I’m going to faint,” “I can’t handle this.” Grounding breaks that loop by forcing your brain to focus on the outside world.
The 5-4-3-2-1 method is simple and powerful. Name:
- Five things you can see (the crack in the wall, your coffee mug, the tree outside)
- Four things you can touch (your jeans, your phone, the chair beneath you, your own arm)
- Three things you can hear (the hum of the fridge, birds outside, your breath)
- Two things you can smell (soap on your hands, the rain)
- One thing you can taste (your toothpaste, a mint, the air)
This isn’t just distraction. It’s neurological redirection. A 2022 study from the Anxiety and Depression Association of America found closing your eyes during a panic attack reduced symptoms by 32% in under 90 seconds. Grounding does the opposite-it opens you back up to reality.
Another tool: personalized safety statements. Write them down. Save them in your phone. Say them out loud: “I’m safe. This is panic, not danger. It will pass. I’ve felt this before and I’m okay.” Repeat them like a mantra. People who used these daily saw their panic attacks shorten from an average of 22 minutes to 14.
Some find distraction helpful. Play a game on your phone. Solve a crossword. Talk to someone-even if it’s just saying, “I’m having a panic moment, can you sit with me?” The goal isn’t to ignore the panic. It’s to stop feeding it with your attention.

Medication: When it helps, when it doesn’t, and how to use it wisely
Medication isn’t a crutch. For many, it’s a bridge.
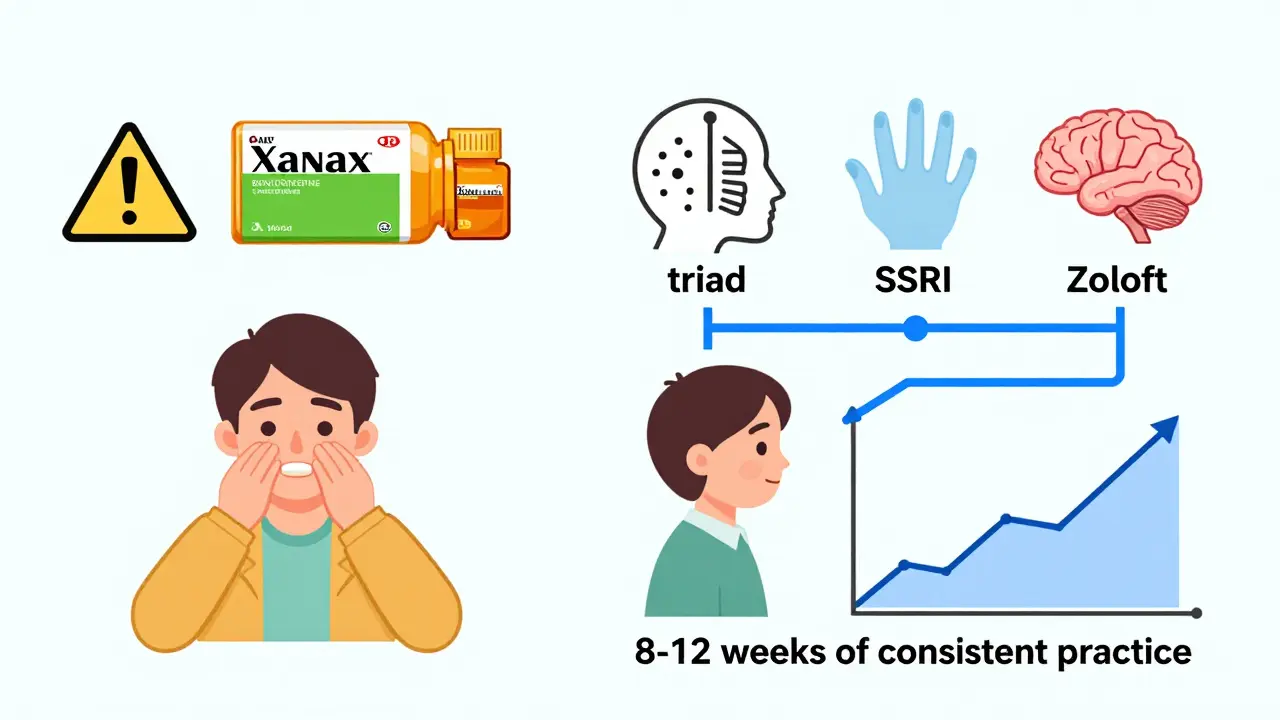
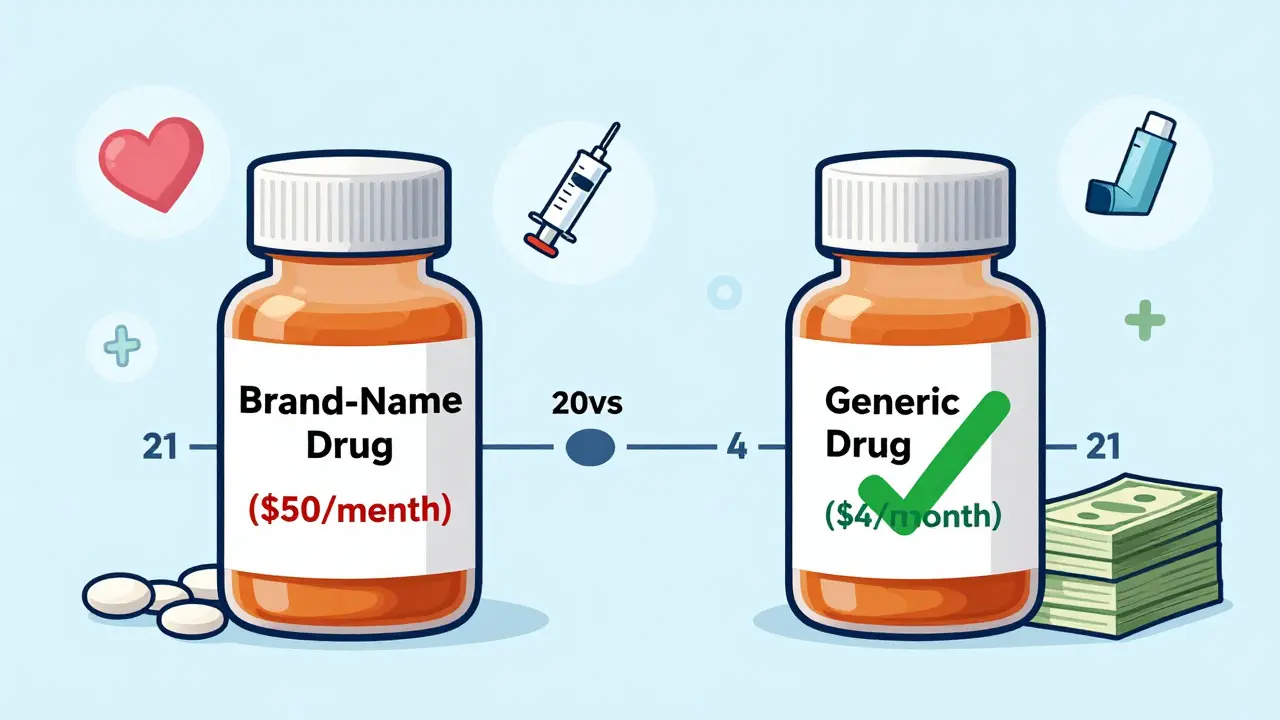
First-line options are SSRIs-medications like sertraline (Zoloft) or paroxetine (Paxil). These aren’t instant. They take 6 to 12 weeks to build up in your system. But once they do, they reduce panic attacks by 60 to 70%. They’re not addictive. They don’t make you feel “high.” They help your brain regulate fear signals over time.
Side effects? Yes. Nausea, insomnia, or feeling emotionally flat at first. But 79% of people who stuck with them for six months said the benefits outweighed the early discomfort.
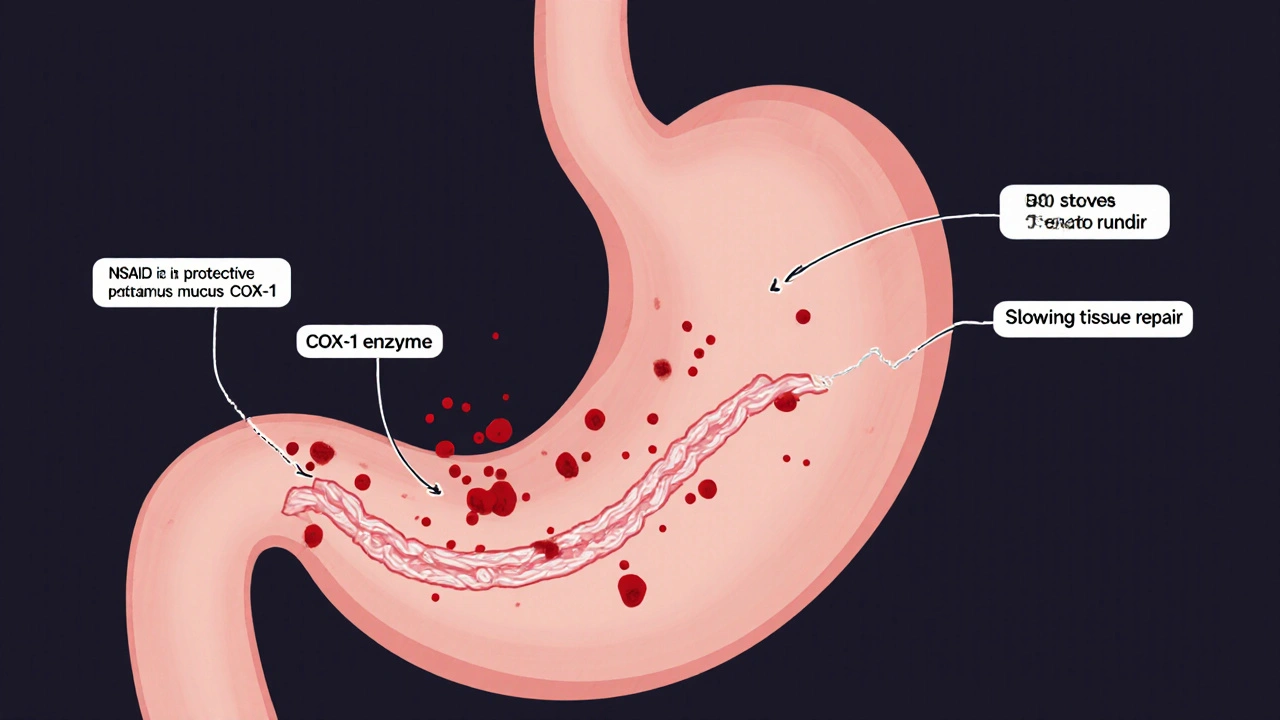
Benzodiazepines-like alprazolam (Xanax) or clonazepam (Klonopin)-work fast. They can calm you down in 15 to 30 minutes. That’s why some people keep them on hand. But they come with big risks. About 23% of daily users develop tolerance within six weeks. That means they need more to get the same effect. Stopping suddenly can cause withdrawal. That’s why experts say: use them only for emergencies, never as your daily fix.
Here’s the key: medication works best when paired with breathing and grounding. A 2022 NIMH study found that 68% of people who used both medication and CBT-based techniques went into remission. Only 42% did with medication alone. The goal isn’t to rely on pills forever. It’s to use them until your brain learns new ways to respond.
Building your plan: Start small, stay consistent
You don’t need to master everything at once.
Week 1: Pick one breathing technique. Practice it for five minutes every morning. Don’t wait for panic to try it.
Week 2: Add one grounding method. Write down three safety statements. Keep them where you’ll see them-on your mirror, in your wallet, on your phone’s lock screen.
Week 3: If you’re considering medication, talk to your doctor. Bring your symptom log. Ask: “Is this right for me? What are the risks? What’s the plan if it doesn’t work?”
Track your progress. Note when attacks happen, what you did, and how long they lasted. After 10-15 entries, patterns emerge. Maybe they happen after skipped meals. Or late nights. Or when you’re avoiding a conversation. Knowing your triggers lets you plan ahead.
Apps like Panic Relief from UCSF offer guided breathing and grounding exercises. They’re free, easy to use, and have 4.3 out of 5 stars from nearly 2,000 users. Wearables that track heart rate can also help. If your heart spikes at 110 bpm while you’re sitting still, you might catch the panic before it fully hits.
What to do when nothing seems to work
It’s okay to feel stuck. Many people struggle to remember their techniques in the middle of an attack. That’s why physical reminders matter. Wear a rubber band on your wrist. Snap it gently when you feel panic rising. Say aloud: “Stop.” It’s a cue your body learns to associate with pausing the spiral.
If breathing and grounding aren’t enough, don’t blame yourself. Talk to a therapist trained in CBT. The American Psychological Association gives CBT the highest rating for panic disorder-70-80% of people improve. Online programs like those from the Centre for Clinical Interventions offer free workbooks. You don’t need to be in a clinic to start.
And if you’re afraid of medication? That’s valid. Talk to your doctor about alternatives. Some people manage well with therapy and lifestyle changes alone. Others need help. Neither choice makes you weak.
It’s not about eliminating panic. It’s about not letting it control you.
Panic attacks don’t mean you’re broken. They mean your body’s alarm system is stuck. You’re not alone. Nearly 5% of adults in the U.S. have had a panic attack. Millions more have learned to manage them.
You don’t need to be fearless. You just need to be prepared. With breathing to calm your body, grounding to anchor your mind, and medication as a tool-not a crutch-you can face panic without fear. Not every attack will vanish. But each time you use your plan, you weaken panic’s power. And that’s progress.
Can breathing techniques stop a panic attack cold?
Yes, if practiced correctly and consistently. Breathing techniques don’t prevent panic from starting, but they stop it from escalating. The 2-2-6 method, for example, can reduce symptoms by 40-60% within 90 seconds by restoring carbon dioxide levels and calming the nervous system. The key is practicing daily-even when calm-so your body knows what to do when panic hits.
Are grounding techniques just distraction?
No. Grounding isn’t about ignoring panic-it’s about shifting your brain’s focus from internal threat signals to external reality. Techniques like 5-4-3-2-1 activate the prefrontal cortex, the part of your brain responsible for rational thought. This interrupts the fear loop in the amygdala. Studies show grounding reduces panic intensity by up to 32% in under two minutes.
Is it safe to use Xanax for panic attacks?
It can be, but only under strict medical supervision and for short-term use. Xanax (alprazolam) works quickly and can reduce panic symptoms by 75% within an hour. But it carries a high risk of dependence. About 23% of daily users develop tolerance within 4-6 weeks. Experts recommend it only as a rescue medication-not daily-and never without combining it with therapy. Long-term use can make panic worse by preventing you from learning coping skills.
Do I need medication to manage panic attacks?
Not necessarily. Many people manage panic effectively with breathing, grounding, and therapy alone. But if you’re having more than two attacks a week, or if panic is keeping you from work, socializing, or sleeping, medication can be a helpful tool. SSRIs like Zoloft are often recommended first because they’re non-addictive and build long-term resilience. Medication isn’t a failure-it’s a support system while you build your skills.
How long does it take to see results from a panic action plan?
You’ll notice small improvements in 2-3 weeks-like shorter attacks or less fear between episodes. But real change takes 8-12 weeks of consistent practice. That’s when your brain starts rewiring. Studies show people who practiced breathing daily for eight weeks cut their panic frequency by nearly half. The goal isn’t perfection. It’s progress: fewer attacks, less fear, more control.
Can I use these techniques if I’m on other medications?
Yes. Breathing and grounding techniques are safe to use with any medication. In fact, they often enhance the effects of SSRIs and reduce reliance on benzodiazepines. Always talk to your doctor before making changes, but these methods don’t interfere with prescriptions. They’re complementary. Many therapists combine them with medication as part of standard care.
Next steps: Start today, not when the next attack hits
Write down your three safety statements. Pick one breathing technique. Set a daily reminder to practice it for five minutes. Download a free app like Panic Relief. Talk to your doctor if you’re unsure about medication. Don’t wait for the next panic to begin your plan. Build it now, while you’re calm. Because when panic comes-and it might-you’ll be ready.




13 Comments