A hard truth up front: every antidepressant, including amitriptyline, carries a boxed warning about suicidal thoughts-especially in people under 25. That doesn’t mean it causes suicide. It means a small but real risk exists during certain windows, and you deserve a clear, practical plan to monitor it. Here’s what that looks like in real life, without scare tactics or sugar-coating.
If you’re taking amitriptyline for depression, anxiety, sleep, or nerve pain, you’re likely here for straight answers: how big is the risk, when is it highest, what should you watch for, and what should you do if your thoughts shift in a bad direction? You’ll find plain guidance below, grounded in the FDA boxed warning (updated 2024), Medsafe New Zealand data sheets, NICE guidance, and large reviews of antidepressant safety. We’ll also cover what to do if you’re supporting someone else, and how to bring this up with your prescriber without derailing treatment.
One more thing: if you’ve already noticed a change in your thinking-more hopelessness, planning, or feeling like a burden-pause here and focus on safety. Remove means, get a trusted person with you, and contact your prescriber or emergency services now. Don’t wait to “see if it passes.” Early action saves lives.
We’ll keep language simple and the steps doable. Your goal is not to learn every technical detail. Your goal is to stay safe while you (and your clinician) see whether amitriptyline is helping.
Quick answer, risk windows, and what to watch for
- TL;DR: A small subset of people-mainly under 25-may experience increased suicidal thoughts when starting amitriptyline or after dose changes. The risk is highest in the first 1-4 weeks and after dose increases or abrupt stops. Most adults over 25 do not see an increased risk, and older adults may even see a reduced risk, per FDA analyses.
- Don’t stop suddenly if you notice thoughts shifting. Tell someone, remove access to means, and contact your prescriber urgently. Stopping cold turkey can worsen mood swings, anxiety, and insomnia.
- Caregivers: daily check-ins matter most during weeks 1-4, after any dose change, and during tapers. Watch for sudden energy with dark thoughts-that combo can be dangerous.
- In New Zealand, Medsafe requires the same suicidality warning as the FDA for all antidepressants, including tricyclics like amitriptyline. The guidance applies whether you’re taking it for depression or for pain/sleep.
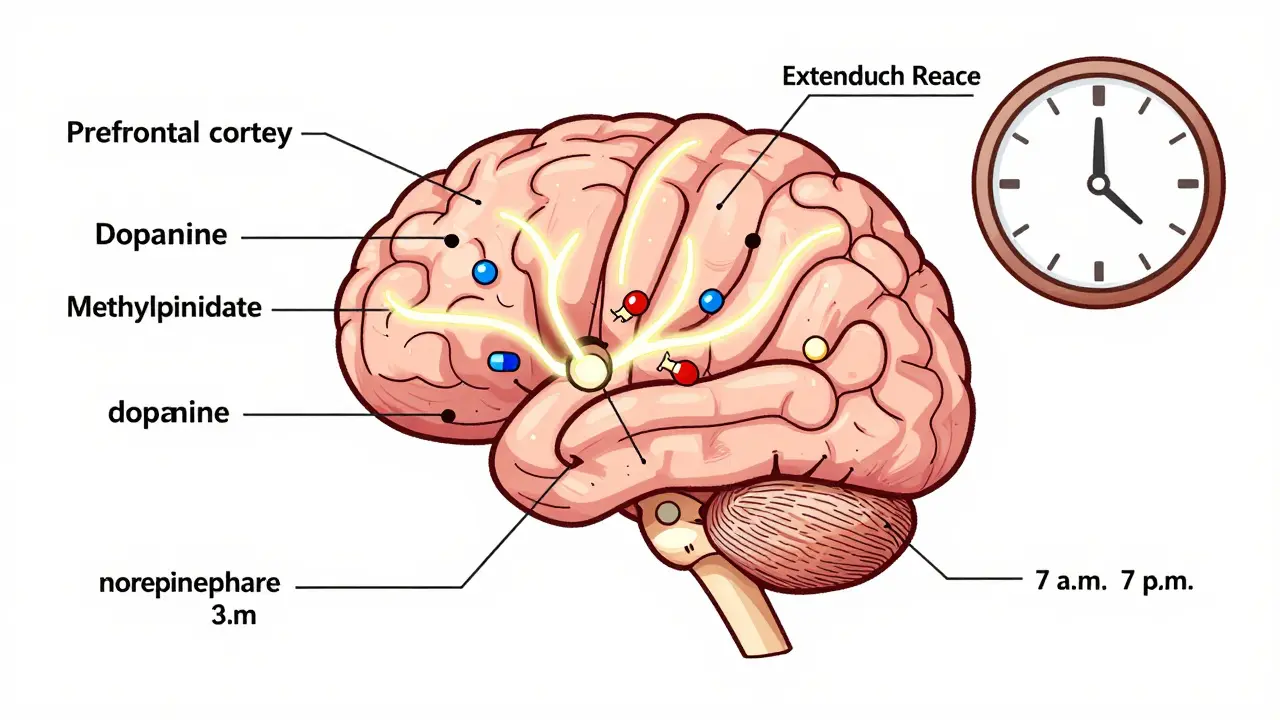
What is amitriptyline? It’s a tricyclic antidepressant (TCA) that’s been around for decades. In Aotearoa New Zealand and elsewhere, it’s used for depression, anxiety, migraine prevention, nerve pain, and insomnia (often at lower doses for the non-depression uses). Like all antidepressants, it can increase energy before mood improves, which is one reason the early window matters-it may give you enough drive to act on dark thoughts that were already present.
How common is the risk? Based on pooled data the FDA used for its boxed warning, suicidal thinking/behavior in youth roughly doubled on antidepressants versus placebo (about 4% vs 2% in the short term). For adults 25+, no overall increase was seen; for 65+, risk may be lower than with placebo. The warning covers all antidepressants, including TCAs. While most of the modern data are from SSRIs/SNRIs, regulators treat amitriptyline similarly for safety monitoring.
Who is most at risk?
- Age under 25 (strongest signal in teens and young adults)
- History of suicide attempts or self-harm
- Rapid dose changes or abrupt stopping
- Co-existing bipolar spectrum symptoms (e.g., periods of too much energy, low need for sleep, racing ideas)
- Alcohol or drug use that worsens impulsivity
- Insomnia or agitation spiking in the early weeks
Warning signs to pay attention to:
- New or worsening thoughts about death, self-harm, or “being better off gone”
- Sudden restlessness, anxiety, or agitation, especially at night
- New impulsivity, irritability, or taking unusual risks
- Talking about feeling like a burden, or saying goodbyes
- Making plans, researching methods, or acquiring means
- A sudden lift in energy while mood is still very low
What to do right now if your thoughts are shifting:
- Don’t go it alone. Move into the same room as someone you trust or invite them over.
- Lock away or remove potential means. Keep only small amounts of medicine accessible.
- Tell your prescriber the same day. Ask for a same-day call-back or urgent review.
- If you feel unsafe or have a plan, call emergency services or go to the nearest emergency department.
Important: keep expectations realistic. If amitriptyline helps you sleep and eases pain, that can support recovery. If it spikes anxiety, agitation, or dark thoughts, that’s a signal to slow down, adjust the dose, add short-term supports, or switch. You and your clinician can fine-tune this. The key is close check-ins during the first month and after any change.
For searchers wondering “is this just me?”-no, this pattern is exactly what regulators warn about. The fix is not tough-guy grit. It’s monitoring, honest reporting, and quick adjustments. That’s how you keep the benefits and cut the risk with amitriptyline suicidal thoughts.

Practical steps: monitoring, reducing risk, and what to do if thoughts appear
Here’s a simple, no-drama plan that people actually follow. Adapt it with your prescriber.
Week-by-week monitoring (first month):
- Week 1: Start low. Take it at night unless advised otherwise. Track sleep, anxiety, restlessness, and any dark thoughts in a notes app. Share daily updates with one person.
- Week 2: If dose increases, double check that support is tight for 5-7 days. Plan a check-in call with your prescriber or GP.
- Week 3-4: Watch for the “energy-before-mood” phase. If energy rises but hope doesn’t, upgrade monitoring (daily check-ins, remove means, ask for a faster follow-up).
- After any change (start, stop, increase, decrease): Treat the next 7-10 days as a higher-risk window. Adjust plans and reduce exposure to triggers (alcohol, sleep loss).
Red flags that warrant urgent contact with your clinician:
- New suicidal thoughts that are hard to shake
- Agitation, pacing, or trouble sitting still
- Severe insomnia (e.g., less than 3-4 hours sleep for 2 nights)
- Mood swings or periods of too much energy with pressured speech
- Any planning or steps taken toward self-harm
What not to do:
- Don’t stop suddenly unless told by a clinician. TCAs can cause withdrawal symptoms-rebound anxiety, insomnia, flu-like symptoms-that can worsen risk.
- Don’t combine with alcohol or sedatives just to sleep. This can cloud judgment and increase overdose danger.
- Don’t keep a large supply on hand. Ask your prescriber or pharmacist about smaller dispenses during higher-risk periods.
What often helps (and is easy to try):
- Timing: Take at night to use sedation for sleep and reduce daytime grogginess.
- Routine: Regular sleep/wake times tame mood swings. Protect the hour before bed.
- Light movement: Short daytime walks can ease tension and improve sleep quality.
- Food and fluids: Stable meals reduce nausea and jitteriness.
- Connection: Daily 5-10 minute check-in with someone who knows your plan.
Simple decision path if thoughts appear:
- If thoughts are passive (“wish I wouldn’t wake up”) and new since starting/increasing: tell someone, remove means, message your prescriber today for advice and earlier review.
- If thoughts are active (planning, urges), or you feel unsafe: have someone stay with you and contact emergency services or go to the nearest emergency department now.
- If agitation or insomnia suddenly spike: ask about dose reduction, slower titration, or adding short-term support (e.g., a brief course of a sleep aid) while staying closely monitored.
Caregiver checklist (family, flatmate, partner):
- Daily check-in during weeks 1-4 and after any change: “How are your thoughts today? Any restless or unsafe feelings?”
- Watch for mixed states: more energy + unchanged hopelessness.
- Help reduce access to means. Keep medicines locked and limit quantities out.
- Ensure they eat, hydrate, and keep a bedtime routine.
- If they mention a plan or feel unsafe, stay with them and contact emergency services.
Questions to ask your prescriber (bring this to your next visit):
- “What dose are we starting at, and how fast do you plan to increase?”
- “When should I check in with you in the first month?”
- “Which side effects are okay to ride out, and which are red flags?”
- “How will we taper if we switch or stop?”
- “Given my history (age, past attempts, bipolar in family), how do we minimize risk?”
Why dose and speed matter: Going slow trims the chance of agitation and insomnia. TCAs are potent; a low-and-slow titration may lower the risk of early mood instability. If your prescriber suggests a pause or micro-adjustments, that’s not “failure”-it’s standard risk management.
Important nuance for amitriptyline: Compared to SSRIs, TCAs can be more dangerous in overdose. That’s one reason prescribers may limit the quantity on hand early on, especially if your risk is higher or you live alone. It’s not punitive; it’s preventive.

Evidence, FAQs, and NZ-specific notes
Below is a compact evidence snapshot with plain-language takeaways. Sources include: FDA boxed warning (updated 2024); Medsafe New Zealand antidepressant safety communications and data sheets (2023-2025); NICE guideline NG222 (Depression in adults, 2022); and large meta-analyses summarised in Cochrane Reviews (latest updates through 2023).
| Topic | What the evidence says | Practical takeaway |
|---|---|---|
| Early risk window | Highest in first 1-4 weeks and after dose changes; energy can rise before mood improves (FDA/NICE). | Plan daily check-ins during these periods; don’t make big life decisions then. |
| Age effect | In under-25s, suicidal thoughts/behaviors ~4% on antidepressants vs ~2% on placebo in short-term trials (FDA). | Extra monitoring for under-25s; consider slower titration and smaller dispenses. |
| Adults 25-64 | No overall increase in suicidality signal across antidepressants (FDA meta-analyses). | Still monitor; risk is not zero, especially with insomnia, agitation, or substance use. |
| Older adults (65+) | Signal may be reduced vs placebo (FDA). TCAs can cause falls, anticholinergic effects. | Weigh fall/cardiac risks; tighten sleep and hydration routines. |
| TCAs vs SSRIs | Regulators apply suicidality warnings to all classes. TCAs carry higher overdose toxicity. | Keep small quantities; lock up meds; discuss safest options if risk is high. |
| Stopping abruptly | Withdrawal can cause anxiety, insomnia, irritability (Cochrane; NICE). | Taper with a plan; report mood shifts during tapers within 48 hours. |
| Comorbid bipolar risk | Antidepressants can flip mood or unmask hypomania in vulnerable people (NICE). | Screen for past “highs”; if present, mood stabilizer strategies may be needed. |
| Alcohol/cannabis | Can worsen impulsivity and sedation; may blunt treatment response (Medsafe advisories). | Avoid or limit, especially early on and during dose changes. |
Frequently asked questions
- Does amitriptyline cause suicidal thoughts in adults over 30?
There’s no consistent increase in risk for adults over 25 in the FDA’s pooled analyses. Still, if insomnia, agitation, or dark thoughts show up after starting or changing dose, treat that as a signal and talk to your clinician quickly. - What if I’m taking amitriptyline for pain or sleep, not depression?
The same warning applies. Lower doses can still shift sleep and anxiety in ways that affect mood. Monitor the same way, especially if the dose increases. - How long until side effects settle?
Sedation, dry mouth, and grogginess often ease over 1-2 weeks. If agitation, restlessness, or suicidal thoughts appear or worsen, don’t wait-update your prescriber now. - Is it safe to mix with alcohol?
Not advised. Alcohol can increase sedation and lower inhibitions, which increases risk. If you’ve been drinking and feel unsafe, get support and avoid being alone. - Can I just reduce the dose myself if I feel off?
Don’t change dose without telling your prescriber. Even small, sudden reductions can trigger withdrawal-like symptoms that complicate mood. - Could amitriptyline make me feel wired instead of sleepy?
Yes, in a small subset. If you feel revved-up, restless, or can’t sleep, report it-dose timing or the dose itself may need adjustment. - What about teens and young adults in New Zealand?
Medsafe follows the same boxed-warning approach as the FDA. For under-25s, prescribers usually pair medication with tight monitoring and therapy, and may limit quantities on hand. - Is it dangerous to keep a big supply at home?
For TCAs, yes-overdose risk is higher than with many modern antidepressants. Ask for smaller dispenses during higher-risk windows. - How do I taper safely if we decide to stop?
Work with your prescriber on a gradual taper (often weekly or biweekly steps). Track sleep, anxiety, and mood during the taper and 1-2 weeks afterward.
Conversation script you can use with your clinician
- “I’m noticing more restless nights and darker thoughts since starting. Can we slow the titration or reassess the dose?”
- “Given my age and history, could we set weekly check-ins for the first month?”
- “If I ever feel unsafe, what’s my exact plan for same-day help?”
New Zealand-specific notes
- Medsafe data sheets for amitriptyline carry the suicidality warning for children, adolescents, and young adults. The advice applies regardless of indication (depression, pain, sleep).
- In Aotearoa, prescribers may prefer lower starting doses for sleep/pain (e.g., 5-25 mg at night) and adjust slowly to limit grogginess and agitation.
- Pharmacists can help with smaller dispenses and blister packs. Ask them to flag interactions (e.g., other sedatives, alcohol).
Pro tips from clinic floors
- Track one or two signals only-sleep hours and daily mood score (0-10). Simple beats perfect.
- Bundle the habit: take your dose with brushing teeth at night, then jot your two numbers.
- Share a screenshot of your week with your prescriber. It speeds up good decisions.
Next steps and troubleshooting by scenario
- Just started (days 1-7): Keep evenings quiet. Avoid alcohol. Tell one person you’re starting. Book a check-in within 7-10 days.
- Dose just increased: Treat the next week as higher risk. Daily check-ins. If sleep tanks or agitation rises, ask about stepping back.
- Thoughts getting darker but no plan: Remove means, ask someone to stay over, message your prescriber for a same-day or next-day review.
- Active plan or urge: Stay with someone now and contact emergency services or go to the nearest emergency department. Safety first; meds discussions can wait a day.
- Considering a switch: Don’t stop abruptly. Ask for a cross-taper plan and tighter follow-up in the first two weeks of the new med.
- Tapering off: Reduce slowly. Keep the same monitoring plan you used at the start, for at least 2 weeks after the last dose.
Credible sources you can mention to your clinician
- US FDA boxed warning on antidepressants and suicidality (updated 2024)
- Medsafe New Zealand antidepressant safety communications and amitriptyline data sheets (2023-2025)
- NICE Guideline NG222: Depression in adults (2022, updates ongoing)
- Cochrane Reviews on antidepressants and withdrawal effects (latest updates through 2023)
You don’t need to “power through” scary thoughts to prove resilience. You need a plan, a person, and a prompt check-in with your prescriber. That’s how you use amitriptyline safely-and how you protect the progress you’re about to make.






17 Comments