When you take a pill once a day instead of three times, it’s not magic-it’s science. Modified-release (MR) formulations are designed to release medication slowly over time, keeping drug levels steady in your bloodstream. This reduces side effects, improves compliance, and makes chronic disease management easier. But here’s the catch: just because two pills look the same doesn’t mean they work the same. For generic versions of these complex drugs, proving they’re equivalent to the brand-name product isn’t as simple as comparing active ingredients. It requires a deep dive into how the drug behaves in your body-and that’s where bioequivalence gets complicated.
Why Modified-Release Formulations Are Different
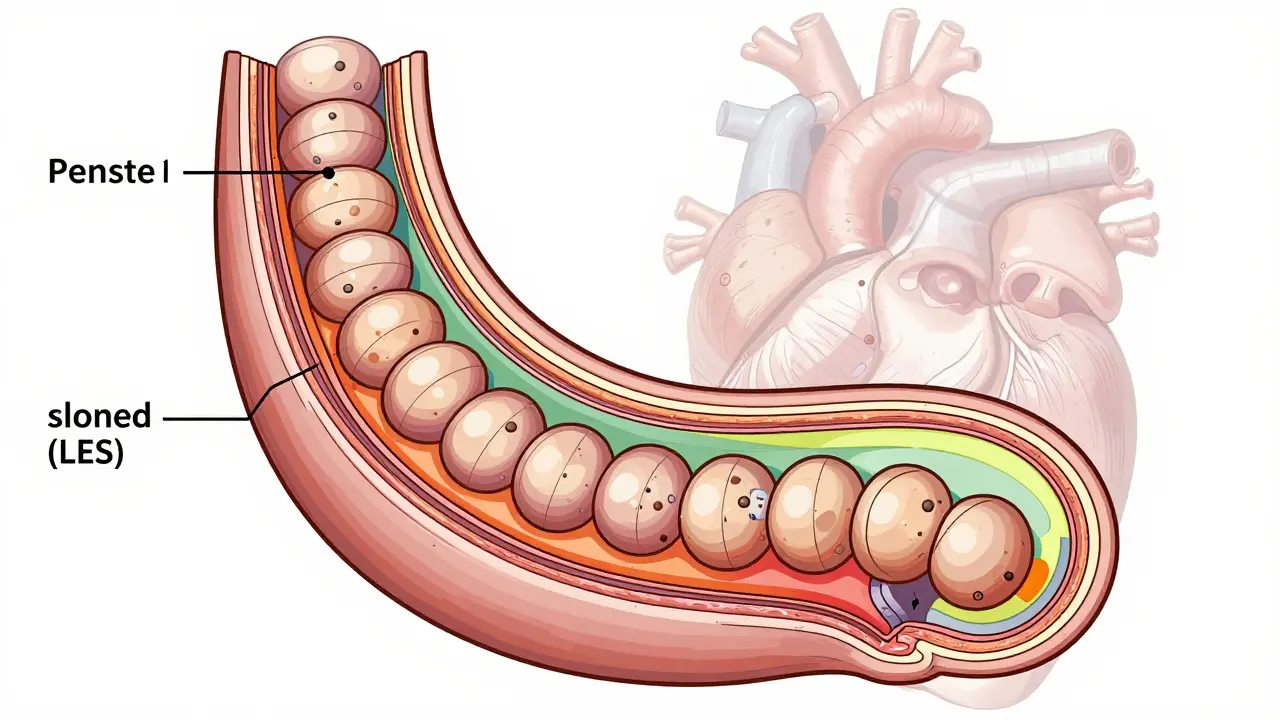
Most pills you’ve taken release their drug quickly-within an hour or two. That’s immediate-release (IR). Modified-release formulations, on the other hand, are engineered to control when and how fast the drug enters your system. Some release in two phases: an initial burst for fast relief, followed by a slow trickle to last all day. Others use coatings or tiny beads to delay absorption until the drug reaches the lower intestine. Still others are built to resist breakdown in stomach acid. These designs aren’t just for convenience. For drugs like warfarin, lithium, or methylphenidate, even small swings in blood concentration can mean the difference between effective treatment and dangerous toxicity. MR formulations reduce peak-to-trough fluctuations by 30-50% compared to IR versions. That’s why 35% of all generic drugs approved in the U.S. since 2015 are modified-release, worth $65 billion in annual sales. But here’s the problem: if a generic version releases its drug too fast, too slow, or unevenly, it won’t behave the same way in your body-even if it contains the exact same amount of active ingredient. That’s why regulators don’t just check the drug’s chemical identity. They need to see how it performs in real time inside the human body.How Bioequivalence Is Measured for MR Drugs
For regular pills, bioequivalence is judged using two main numbers: AUC (area under the curve) and Cmax (maximum concentration). These tell you how much drug got into your blood and how fast. For MR drugs, that’s not enough. Take zolpidem extended-release (Ambien CR). It has two parts: one that kicks in fast to help you fall asleep, and another that lasts longer to keep you asleep. Regulators don’t just look at the total AUC. They split it into two pieces-partial AUCs (pAUC). One measures drug exposure from time zero to 1.5 hours. The other covers 1.5 hours to infinity. Both must fall within 80-125% of the brand-name drug. If one part doesn’t match, the generic fails-even if the total AUC looks perfect. The same applies to drugs like Concerta (methylphenidate ER). In 2012, a generic version was rejected because it didn’t release enough drug in the first two hours. That tiny window was critical for effectiveness. The FDA’s Complete Response Letter pointed out that the generic’s release profile didn’t mirror the original’s early-phase behavior. For highly variable drugs-like those with a within-subject coefficient of variation above 30%-regulators use a special method called Reference-Scaled Average Bioequivalence (RSABE). This adjusts the acceptance range based on how much the reference product itself varies between doses. The FDA caps scaling at 57.38% to prevent overly wide limits. Implementing RSABE adds 6-8 months to development time and requires advanced statistical modeling.
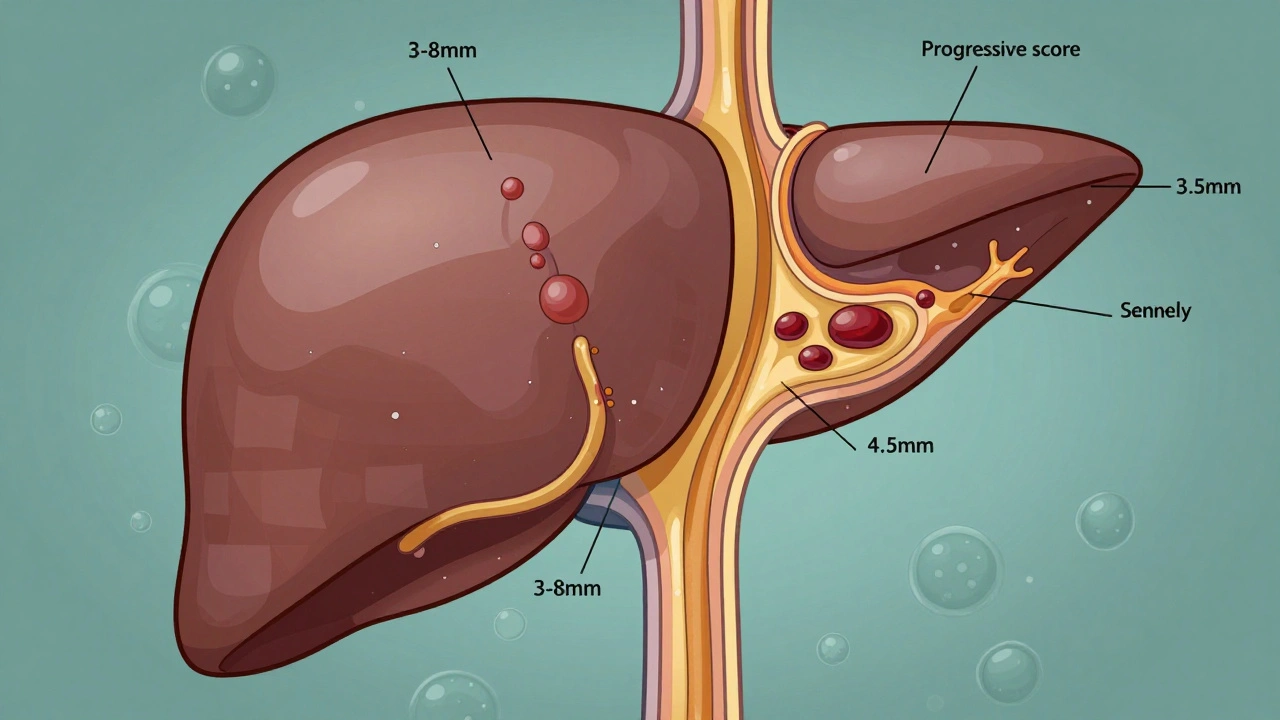
Testing Requirements: Dissolution, pH, and Alcohol
Bioequivalence isn’t just about what happens in your blood. It starts in the lab-with dissolution testing. This simulates how the drug breaks down in your digestive system. The FDA requires ER tablets to be tested at three pH levels: 1.2 (stomach acid), 4.5 (upper intestine), and 6.8 (lower intestine). The dissolution profiles of the generic and brand-name products must be similar, measured by a similarity factor called f2. If f2 is below 50, the products are considered dissimilar. For beaded capsules, only one pH condition is needed. That’s a big difference in complexity. Then there’s alcohol. Many ER pills can release their entire dose at once if taken with alcohol-a phenomenon called “dose dumping.” It’s dangerous. If you take an extended-release oxycodone tablet with a beer, you could overdose. The FDA requires alcohol testing for any ER product containing 250 mg or more of active ingredient. Studies use 40% ethanol solutions to mimic the effect. Between 2005 and 2015, seven ER products were pulled from the market due to this risk. Manufacturers often fail these tests early on. One formulation scientist at Teva reported 35-40% failure rates in early development for ER oxycodone generics. It’s not just about getting the right ingredients. It’s about engineering the right release mechanism.Regulatory Differences Between Agencies
Not all regulators think the same way. The FDA, EMA, and WHO have different rules for MR bioequivalence-and they’re not always aligned. The FDA mostly uses single-dose, fasting studies. They argue these are more sensitive at catching differences in release profiles. The EMA, however, still requires steady-state studies for some MR drugs-especially when the drug builds up in the body over time. Steady-state means taking the drug daily until concentrations stabilize. This takes weeks. It’s expensive and hard on volunteers. The WHO says MR bioequivalence criteria are “essentially the same” as for regular drugs. That’s not true in practice. Both the FDA and EMA demand extra steps: partial AUCs, alcohol testing, multi-pH dissolution. The WHO’s position is seen by many experts as outdated. For narrow therapeutic index (NTI) drugs like warfarin, the FDA tightens the acceptance range to 90-111.11%. That’s stricter than the standard 80-125%. Why? Because even a 10% difference can lead to bleeding or clotting. In 2016, a study in Neurology found that 18% of generic MR antiepileptic drugs had higher seizure breakthrough rates than the brand, even though they passed standard bioequivalence tests. That’s a red flag.
Cost, Time, and the Real-World Impact
Developing a generic MR drug costs $5-7 million more than a regular one. Why? Because the studies are longer, more complex, and require specialized equipment. A single-dose MR bioequivalence study runs $1.2-1.8 million. An IR study? $0.8-1.2 million. The extra cost comes from needing more volunteers, longer monitoring periods, advanced pharmacokinetic modeling software (like Phoenix WinNonlin or NONMEM), and specialized dissolution apparatuses (USP Apparatus 3 or 4 instead of the standard Apparatus 2). And the timeline? Most applicants don’t get it right the first time. Between 2018 and 2021, 22% of MR generic applications were rejected because of inadequate pAUC data. A successful case from Sandoz shows it’s possible: they got approval for an ER tacrolimus generic using a dissolution-based biowaiver (f2=68 at pH 6.8), saving $1.5 million and 10 months. For small biotechs, this is nearly impossible. Only 3% of MR BE studies are done by small companies. The rest? Big pharma and contract research organizations (CROs) like Covance, ICON, and Syneos Health. They have the labs, the staff, and the experience.What’s Next for Modified-Release Bioequivalence
The field is evolving fast. The FDA is working on a new 2024 guidance for complex MR products-things like gastroretentive systems and multiparticulate beads. These are harder to test because they don’t dissolve uniformly. In vitro-in vivo correlation (IVIVC) models are gaining traction. If a lab test can reliably predict how a drug will behave in the body, regulators may allow biowaivers without human studies. The FDA has accepted Level A IVIVC for 12 MR products since 2019, including extended-release paliperidone. Pharmaceutical companies are also using PBPK (physiologically based pharmacokinetic) modeling to simulate drug behavior before ever testing in humans. A 2022 DIA survey found 68% of major pharma firms now use this approach for MR development. The bottom line? The global MR drug market is growing. By 2028, it’s expected to hit $480 billion. And 42% of all prescription sales will be MR formulations. But for these drugs to be safe and effective, the bioequivalence standards must keep pace. It’s not just about matching a label. It’s about matching a pattern of release. And that pattern? It’s everything.Why can’t generic modified-release drugs just match the active ingredient like regular generics?
Because the way the drug is released matters just as much as how much is in the pill. A generic might have the same amount of active ingredient, but if it releases too fast, too slow, or unevenly, it won’t work the same in your body. For example, a drug meant to last 12 hours might dump all its content in the first hour if the coating is wrong. That can cause side effects or make the drug ineffective later. Bioequivalence testing looks at the entire release profile, not just the total dose.
What is partial AUC and why is it important for modified-release drugs?
Partial AUC (pAUC) measures drug exposure over a specific time window, not the entire curve. For drugs like Ambien CR, which have two phases of release, regulators need to know if the early burst and the slow release each match the brand. The pAUC from 0-1.5 hours shows if the fast-acting part works right. The pAUC from 1.5 hours to infinity checks the extended part. If either part is off, the drug won’t perform the same way-even if the total AUC looks fine. This is critical for drugs where timing affects safety or effectiveness.
Why do some extended-release drugs need alcohol testing?
Some ER formulations can release their entire dose all at once if taken with alcohol. This is called dose dumping. For drugs like oxycodone or methylphenidate, that can lead to overdose, hospitalization, or even death. The FDA requires alcohol testing for any ER product with 250 mg or more of active ingredient. The test uses a 40% ethanol solution to simulate what happens when someone drinks alcohol with the pill. Between 2005 and 2015, seven ER drugs were pulled from the market because they failed this test.
What’s the difference between FDA and EMA requirements for MR bioequivalence?
The FDA mostly uses single-dose fasting studies to test MR drugs, believing they’re more sensitive to differences in release. The EMA sometimes requires steady-state studies-where patients take the drug daily for weeks until levels stabilize. The EMA also focuses more on parameters like half-value duration and midpoint duration time, while the FDA uses partial AUCs. The FDA requires dissolution testing at three pH levels for tablets; the EMA does too, but with less specific guidance. These differences mean a generic approved in the U.S. might not get approved in Europe without additional testing.
Are generic modified-release drugs as safe as brand-name ones?
Most are. But not all. Studies have shown that some generic MR antiepileptic drugs had higher seizure breakthrough rates than the brand, even though they passed standard bioequivalence tests. This suggests that current testing might miss subtle differences in release patterns. For drugs with a narrow therapeutic index-like warfarin or lithium-the stakes are higher. The FDA has tightened acceptance criteria for these, but challenges remain. Always talk to your doctor if you notice changes in how a generic MR drug works for you.
How long does it take to develop a generic modified-release drug?
It typically takes 5-7 years from start to approval-about 2-3 years longer than a regular generic. That’s because of the complexity of formulation development, the need for multiple dissolution tests, and the longer bioequivalence studies. If the drug is highly variable, adding Reference-Scaled Average Bioequivalence (RSABE) can add another 6-8 months. Many applications get rejected the first time due to inadequate pAUC data or failed alcohol testing. Success requires deep expertise in pharmacokinetics and dissolution science.





8 Comments