Every year, millions of people in the U.S. get the wrong medication, the wrong dose, or wrong instructions - and many of these mistakes happen right where you expect the safest care: at the hospital or your local pharmacy. The truth is, medication errors are more common than most people realize, and they look very different depending on where they happen.
Hospitals: More Errors, But More Checks
In hospitals, medication errors are everywhere. One study found that nearly 1 in 5 doses given to patients contained some kind of mistake - whether it was the wrong drug, wrong time, or wrong amount. Nurses, doctors, and pharmacists are juggling dozens of patients at once, often under pressure. A patient on a ventilator might get morphine instead of saline. Someone with kidney disease might get a standard dose of a drug that should be cut in half. Timing gets messed up. Labels get misread. It’s not always negligence - it’s the system working under strain. But here’s the thing: hospitals have layers of protection. Before a drug reaches a patient, it usually passes through multiple hands. The pharmacist checks the order. The nurse scans the barcode on the pill and the patient’s wristband. If something’s off, someone usually catches it. That’s why, even though hospitals have a 20% error rate during the dispensing and administration phases, far fewer of those errors actually hurt patients. A 2006 study in JAMA Internal Medicine looked at 36 hospitals and nursing homes and found that while errors were common, many were caught before they caused harm. That’s because hospitals have built-in safety nets. Barcode scanning, electronic health records, double-check protocols - they all add up. In large academic hospitals, staff report about 100 medication errors every month. That sounds scary, but it’s actually a sign the system is working - because they’re reporting them, not hiding them.Retail Pharmacies: Fewer Errors, But Fewer Safeguards
At your local pharmacy, the numbers look better on paper. Studies show only about 1.5% of prescriptions filled in community pharmacies contain a dispensing error. That’s roughly 1 error per 10,000 prescriptions. Sounds low, right? But here’s the catch: in retail pharmacies, the patient is often the last line of defense. There’s no nurse scanning your wristband. No doctor double-checking your chart. You walk up, hand over your prescription, and get a bottle with a label. If the label says “take one tablet twice a day” but the doctor wrote “once a week,” you might not notice. And if you don’t notice, you take it - and that’s when things go wrong. One well-documented case involved a woman who was prescribed estradiol once a week for hormone therapy. The pharmacy transcribed it as “twice daily.” She took it every day for weeks. She ended up with severe side effects and had to visit her doctor for follow-up care. That’s not rare. AHRQ reports that transcription errors - where the pharmacist misreads or miskeys the doctor’s instructions - are the most common type of error in retail settings. And while hospitals have error-reporting systems built into their software, most community pharmacies didn’t have formal reporting until recently. Even now, many pharmacists fear punishment if they admit a mistake. So errors go unreported. The FDA gets over 100,000 reports a year - but experts say that’s less than 10% of what actually happens.What Kind of Mistakes Happen Where?
The types of errors differ because the systems are different. In retail pharmacies, the top three errors are:- Wrong medication (giving lisinopril instead of losartan)
- Wrong dose (giving 10 mg instead of 5 mg)
- Wrong directions (saying “take with food” when it should be “take on empty stomach”)
- Prescribing: A doctor orders the wrong drug because they’re tired or distracted.
- Transcribing: A nurse types the order into the system wrong.
- Dispensing: A pharmacist pulls the wrong bottle from the automated system.
- Administration: A nurse gives the drug at the wrong time or to the wrong patient.

Why Do These Errors Happen?
The reasons behind errors are different in each setting. In retail pharmacies, 80% of errors come from cognitive mistakes - the kind that happen when you’re tired, stressed, or distracted. A pharmacist might be juggling 10 phone calls, a drive-thru window, and a line of customers. The software might suggest a drug that looks similar to the one prescribed. The label printer might smudge the dosage. It’s not that pharmacists are careless - it’s that the system is designed for speed, not safety. In hospitals, the biggest problems are communication breakdowns. A doctor writes a prescription in shorthand. A nurse misreads it. A pharmacist doesn’t have time to call back. Staffing shortages make it worse. A nurse might be responsible for 8 patients in a single shift - and one of them is having a heart attack. Mistakes happen when people are stretched too thin. Both settings suffer from underreporting. Pharmacists fear being blamed. Nurses worry about losing their jobs. Patients don’t know what to look for. That means the real numbers are probably much higher than what’s officially recorded.Who Gets Hurt the Most?
The consequences of medication errors aren’t the same in both places. In hospitals, patients are often sicker. A wrong dose of insulin can send someone into a coma. A wrong antibiotic can trigger sepsis. When errors happen here, the results can be deadly - but because patients are monitored closely, many are caught in time. In retail pharmacies, patients are usually healthier. They’re picking up blood pressure pills, antidepressants, or painkillers for chronic conditions. But that doesn’t mean the risk is low. A patient taking warfarin who gets the wrong dose could bleed internally. Someone on thyroid medication might develop heart problems. A 2007 NIH study found that even though only 1 in 10,000 prescriptions had a dispensing error, three of those led to hospitalization. And here’s the scary part: in retail pharmacies, you might not even know you were given the wrong medicine. You take it. You feel fine. You keep taking it. Months later, you develop a side effect - and your doctor has no idea it’s because of a pharmacy mistake.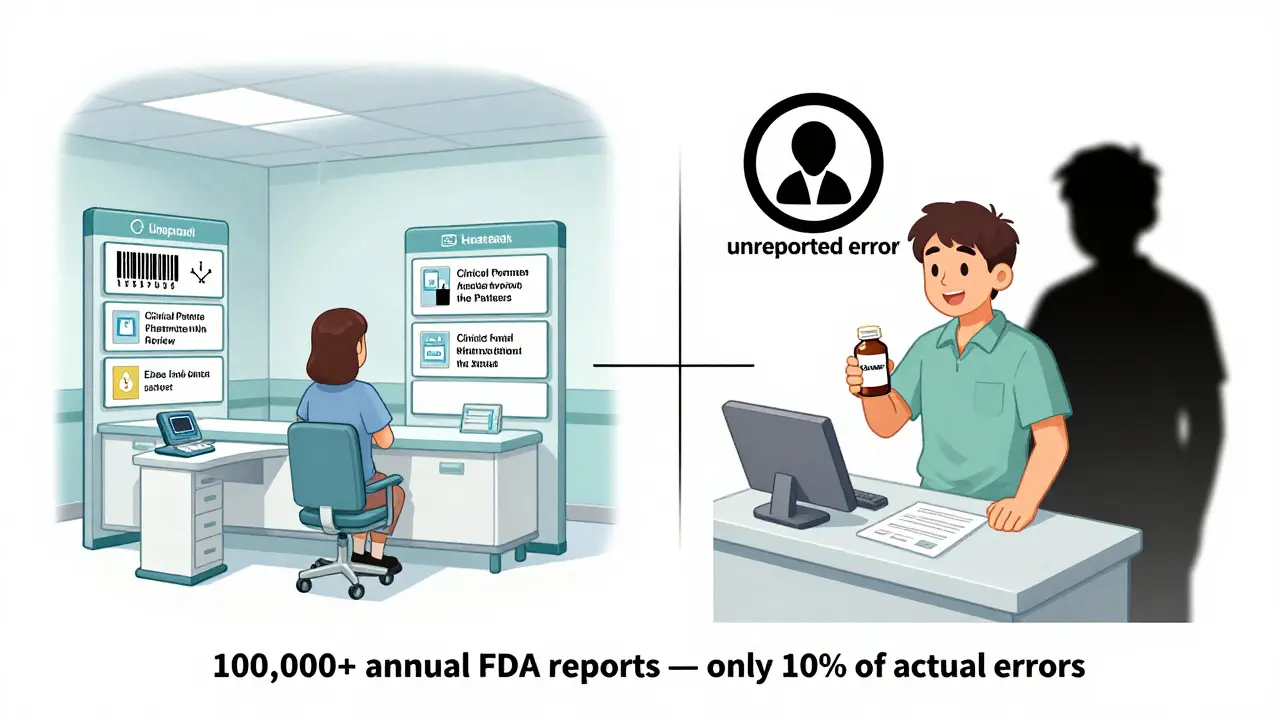
How Are We Fixing This?
The good news? Both settings are getting better. In hospitals, barcode scanning has cut errors by up to 86%. Electronic prescribing has reduced handwriting mistakes. Clinical pharmacists now sit on rounds with doctors to catch problems before they happen. Mayo Clinic’s system reduced errors by 52% after integrating their EHR and pharmacy software. In retail pharmacies, things are changing too. CVS Health rolled out AI-powered verification systems in 2022 that cut dispensing errors by 37%. California now requires pharmacies to log all errors for state review. The FDA is pushing for nationwide reporting standards. And new tools like Clinical Decision Support Systems (CDSS) now pop up warnings if a pharmacist tries to dispense 100 mg of a drug that should be 10 mg. But the biggest fix isn’t technology - it’s culture. Both hospitals and pharmacies need to stop punishing people for mistakes and start learning from them. When a pharmacist admits a near-miss, they should be thanked, not scolded. When a nurse catches a wrong dose, they should be celebrated, not ignored.What You Can Do
You’re not powerless. Here’s how to protect yourself:- Always ask: “Is this the right medicine for me?”
- Compare the pill in the bottle to the description on the label.
- Check the dosage. If it says “take one tablet twice a day,” but your doctor said “once a week,” ask why.
- Keep a list of all your meds - including doses and why you take them - and bring it to every appointment.
- If something feels off after taking a new drug, call your doctor or pharmacist. Don’t wait.
What’s Next?
The future of medication safety lies in integration. The FDA’s Digital Health Center of Excellence is testing AI tools that monitor prescriptions in real time - whether they’re written in a hospital or filled at a drugstore. By 2025, these systems could flag a dangerous interaction before a pharmacist even opens the bottle. But until then, the system still depends on people - doctors, pharmacists, nurses, and you. Mistakes will happen. But with better tools, better reporting, and better awareness, fewer of them will hurt someone.Are medication errors more common in hospitals or pharmacies?
Hospitals have higher error rates - about 20% of doses contain some kind of mistake - but retail pharmacies have fewer errors, around 1.5% of prescriptions. The difference is in detection: hospitals have multiple safety checks, while pharmacies rely mostly on the patient to catch mistakes.
What’s the most common type of pharmacy error?
The most common error in retail pharmacies is a transcription mistake - when the pharmacist misreads or miskeys the doctor’s instructions. For example, writing “twice daily” instead of “twice weekly.” This often happens with similar-looking drug names or rushed workflows.
Can medication errors be prevented?
Yes - but it takes both technology and culture change. Hospitals use barcode scanning and clinical pharmacists to catch errors. Pharmacies are adopting AI verification and mandatory error reporting. But the biggest improvement comes when staff feel safe reporting mistakes without fear of punishment.
Why do pharmacy errors go unnoticed?
In retail pharmacies, there’s no one checking the medication after it’s dispensed. Patients often don’t know what the right dose is, or they assume the pharmacist got it right. Without a second check, even serious mistakes can slip through - especially with chronic medications taken daily.
What should I do if I think I got the wrong medication?
Don’t take it. Call your pharmacy right away and ask them to verify the prescription with your doctor. Keep the pill bottle and the original prescription. If you’ve already taken it and feel unwell, contact your doctor or go to urgent care. Never ignore a feeling that something’s wrong - it could save your life.
Medication safety isn’t just a hospital problem or a pharmacy problem - it’s a shared responsibility. The system isn’t perfect, but you’re not powerless. Stay informed. Stay alert. And never assume someone else has already checked.






12 Comments