Polypharmacy Risk Assessment Tool
Assess Your Medication Risk
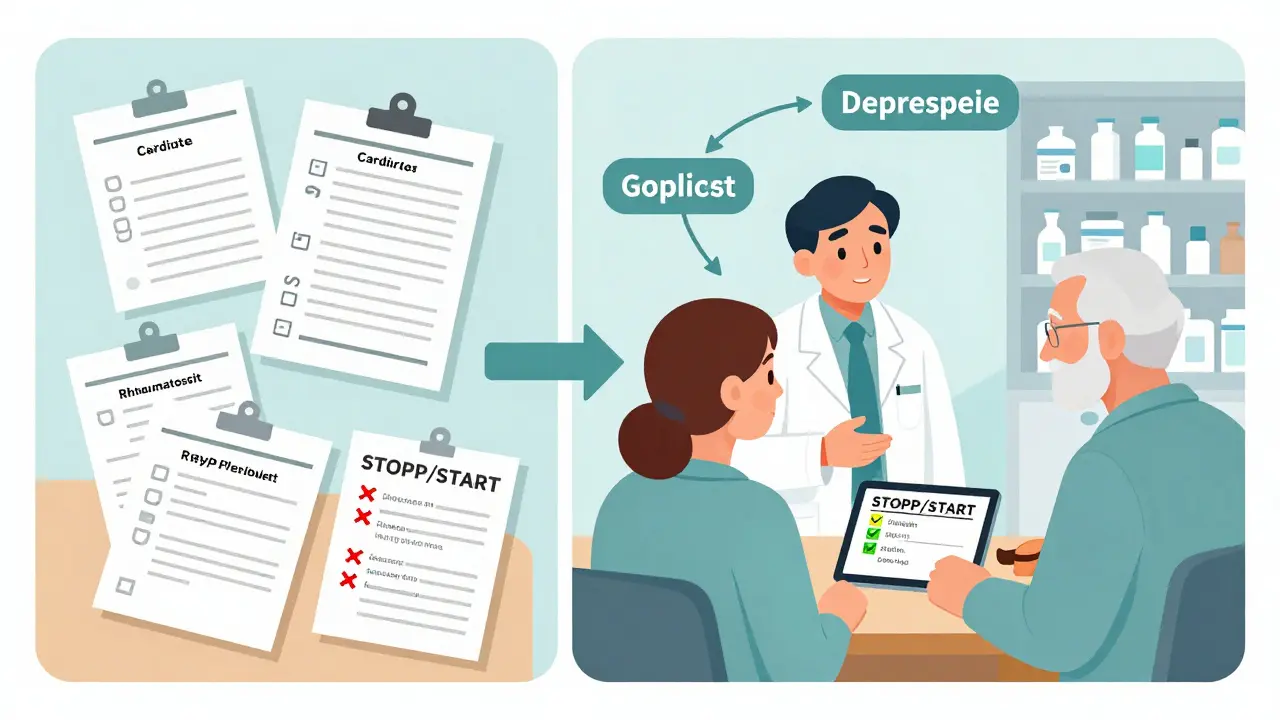
This tool identifies potentially inappropriate medications for older adults based on Beers Criteria and STOPP/START guidelines. Remember: This is for educational purposes only. Always consult a healthcare provider before making medication changes.
Results
Estimated risk of adverse drug events (ADEs) based on current medications and age.
Potentially Inappropriate Medications
Next Steps
Consider pharmacist-led medication review and deprescribing plan. Contact your healthcare provider for personalized guidance.
Why Polypharmacy Is a Silent Crisis in Older Adults
Imagine an 82-year-old woman taking 12 medications daily: one for blood pressure, two for arthritis, three for cholesterol, a sleep aid, an antidepressant, a proton pump inhibitor, a blood thinner, a diuretic, a vitamin D pill, and two supplements. She doesn’t feel worse - but she’s more likely to fall, get confused, or end up in the hospital. This isn’t rare. In the U.S., nearly 41% of adults over 65 take five or more medications. For nearly one in five, that number jumps to ten or more. These aren’t prescriptions for life - they’re a ticking time bomb.
Polypharmacy - the routine use of five or more drugs - doesn’t happen by accident. It builds up over years: a cardiologist adds a pill, a rheumatologist prescribes another, a primary care doctor keeps renewing them all. No one steps back to ask: Is this still helping? The result? Adverse drug events (ADEs) cause nearly 28% of all hospital admissions in older adults. Many of these are preventable.
What Makes a Medication Inappropriate in Older Adults?
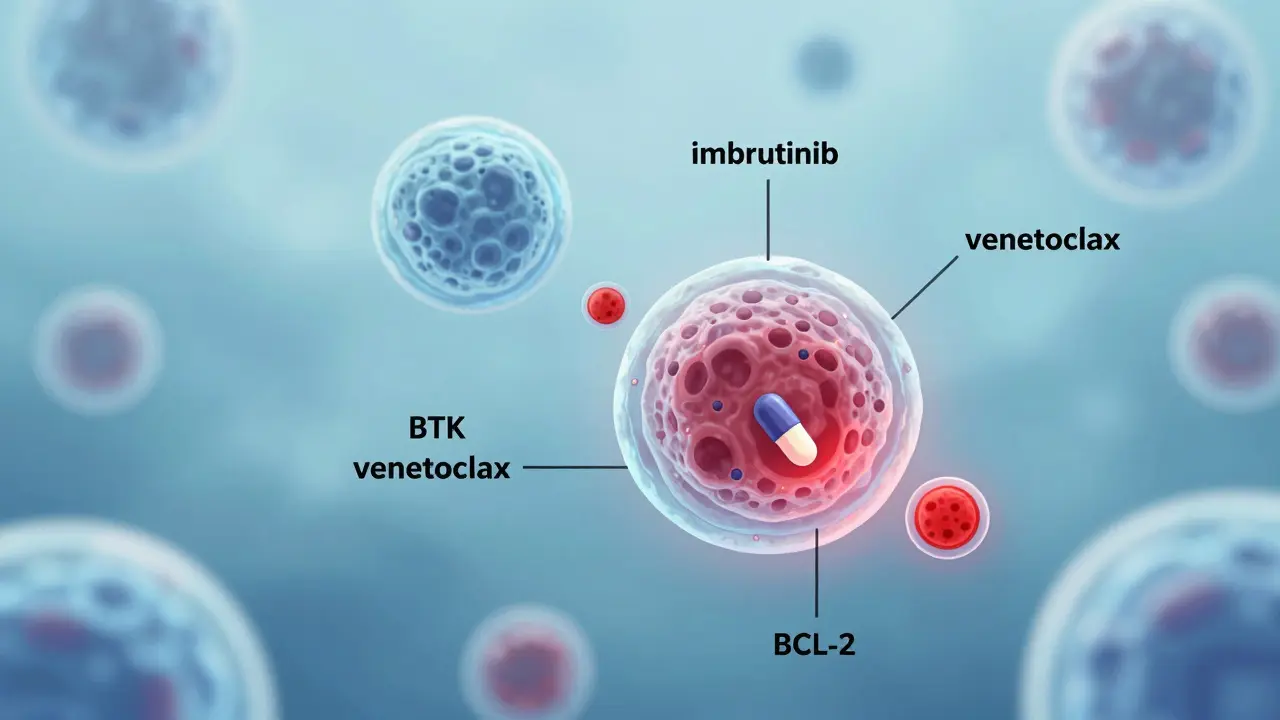
Not all multiple medications are bad. Some are life-saving. The problem is when drugs are prescribed without matching the patient’s goals, life expectancy, or actual needs. The American Geriatrics Society’s Beers Criteria (2023 update) lists 60+ medications that should be avoided or used with extreme caution in older adults. Examples include long-acting benzodiazepines like diazepam, which increase fall risk by 50%, or nonsteroidal anti-inflammatories like ibuprofen, which can cause kidney failure or stomach bleeds in seniors.
But the Beers Criteria alone aren’t enough. That’s why tools like STOPP/START (v3, 2021) and FORTA are now standard. STOPP identifies potentially inappropriate prescriptions - like giving an anticholinergic for overactive bladder when it causes confusion. START finds missed opportunities - like not prescribing a statin for someone with diabetes and heart disease. One study found that using STOPP/START reduced inappropriate prescribing by 31% in just six months.
Here’s the catch: a drug that’s inappropriate for one person might be essential for another. A blood thinner might be risky for someone with a history of falls - but deadly to stop if they have atrial fibrillation. That’s why blanket rules fail. Personalization is the only path forward.
The Only Intervention That Actually Works
Not all medication reviews are created equal. Researchers classify them into three types:
- Type I: Just looking at the medication list.
- Type II: Adding a check for whether the patient is taking them.
- Type III: Face-to-face (or video) visits with a clinician who reviews medications and the patient’s health status, goals, and symptoms.
Only Type III works. A 2023 JAMA Network Open study found Type III interventions reduced hospital readmissions by 18.3%. Types I and II? No measurable difference. Why? Because you can’t deprescribe safely without understanding the person behind the pills.
Pharmacists leading these reviews are the key. In clinics where pharmacists work under Collaborative Practice Agreements (CPAs), deprescribing rates are 37.6% higher than when doctors work alone. But only 22 U.S. states allow these agreements. In places without them, progress stalls.
And it’s not just about cutting pills. It’s about replacing them. One patient on five sleeping pills was switched to cognitive behavioral therapy for insomnia - and stopped needing any medication. Another had his antipsychotic for dementia-related agitation stopped after a behavioral plan was put in place. Both saw improved alertness and fewer falls.
Who Benefits Most - And Who Doesn’t
Not every older adult responds the same way to deprescribing. Research shows the biggest wins are in patients aged 65-79. For them, mortality dropped by nearly 15% after careful medication reviews. For those over 80? The benefit shrinks to 5.2% - and sometimes disappears. Why? Frailty, multiple organ decline, and less time to see benefit from preventive meds.
Patients with dementia see 19.3% less benefit than those without. Why? Because their ability to communicate symptoms is limited. Stopping a medication might cause agitation or withdrawal - but they can’t say, “I feel worse.” That’s why these cases need even more caution, family input, and close monitoring.
And here’s a hidden truth: 38.7% of older adults are undertreated. They’re on too many drugs - but missing essential ones. A diabetic on seven medications might not be on aspirin or a statin. A person with osteoporosis might not be on a bone-strengthening drug. Good deprescribing doesn’t mean fewer pills - it means the right pills.
How Clinicians Are Doing It Right
At Duke University Health System, they use a simple five-step approach:
- Get the real medication list - not the one on paper. Call pharmacies. Ask family.
- Use STOPP/START or FORTA to flag risky or missing meds.
- Review each drug: Why was it started? Is it still needed? What’s the risk of stopping?
- Involve the patient. Ask: “What do you hope to get from these pills?”
- Plan the taper. Don’t stop cold. Cut one at a time. Monitor for 4-6 weeks.
The Veterans Health Administration (VHA) took this further. They embedded clinical pharmacists in every geriatric clinic. Within two years, they cut potentially inappropriate medications by 26.8%. They didn’t just remove drugs - they replaced them with non-drug options: exercise for back pain, light therapy for sleep, social engagement for depression.
Community clinics struggle. Most primary care doctors have less than five minutes per patient to review meds. Medicare doesn’t pay for comprehensive reviews - only 15% of Medicare Advantage plans reimburse for them. That’s why many just keep renewing prescriptions. It’s easier.

The Hidden Barriers - And How to Overcome Them
Even when clinicians know what to do, they hit walls:
- Fragmented care: 78% of older adults see five or more providers a year. No one has the full picture.
- Poor documentation: Only 33% of electronic health records track medication adherence.
- Patient fear: 68% of seniors are terrified of stopping a pill - even if it’s harmful. “My doctor gave me this - it must be important.”
- Time and pay: A full medication review takes 45-60 minutes. Few clinics have the staff or funding.
Solutions exist. Telehealth is helping. In 2025, 75% of pharmacist-led reviews happened via video. That’s faster, more convenient, and just as effective. AI tools are emerging too. Epic’s new “Polypharmacy Risk Score” predicts ADEs with 87% accuracy by analyzing EHR data - dosage, age, kidney function, drug interactions.
But tech alone won’t fix this. It needs people. Teams. A pharmacist, a nurse, a social worker, and a doctor - all talking to each other and to the patient. The American Society of Consultant Pharmacists recommends one clinical pharmacist for every 1,200-1,500 older patients. Most clinics have zero.
What’s Coming Next
The future of geriatric polypharmacy is here - and it’s changing fast. In 2024, Medicare started penalizing doctors if more than 30% of their patients are on ten or more medications. That’s a financial nudge - and it’s working. Hospitals are finally paying attention.
The American Geriatrics Society is releasing Beers Criteria v2026 in late 2025, with new deprescribing algorithms built in. Researchers are testing personalized risk calculators that use genetic data to predict who’s most likely to have bad reactions. And the National Institute on Aging is prioritizing studies on how long it takes to safely stop psychotropic drugs - because sudden withdrawal causes 23.7% of adverse events in this group.
By 2030, experts predict comprehensive medication reviews will be standard care for every older adult. Why? Because value-based payment models now reward lower hospitalization rates - and polypharmacy is the #1 driver of preventable admissions.
What You Can Do Today
If you’re caring for an older adult:
- Ask for a full medication list - from every provider. Write it down. Update it every six months.
- Ask: “Which of these medicines are still necessary? Which ones might be doing more harm than good?”
- Request a pharmacist-led review. Most hospitals and clinics can refer you.
- Don’t stop anything cold. Work with a provider to taper safely.
- Track changes: Did they sleep better? Fall less? Feel clearer? That’s the real measure of success.
Medications aren’t magic. They’re tools. And like any tool, they can be useful - or dangerous - depending on how they’re used. For older adults, the goal isn’t to take fewer pills. It’s to take the right ones - and only the ones that truly matter.







13 Comments