For many women, menopause isn’t just about hot flashes and sleepless nights-it’s a turning point that brings real questions about health, safety, and quality of life. If you’re wondering whether hormone therapy is right for you, you’re not alone. Millions of women are weighing the same choices today, and the answers aren’t as simple as they were 20 years ago.
What Hormone Therapy Actually Does
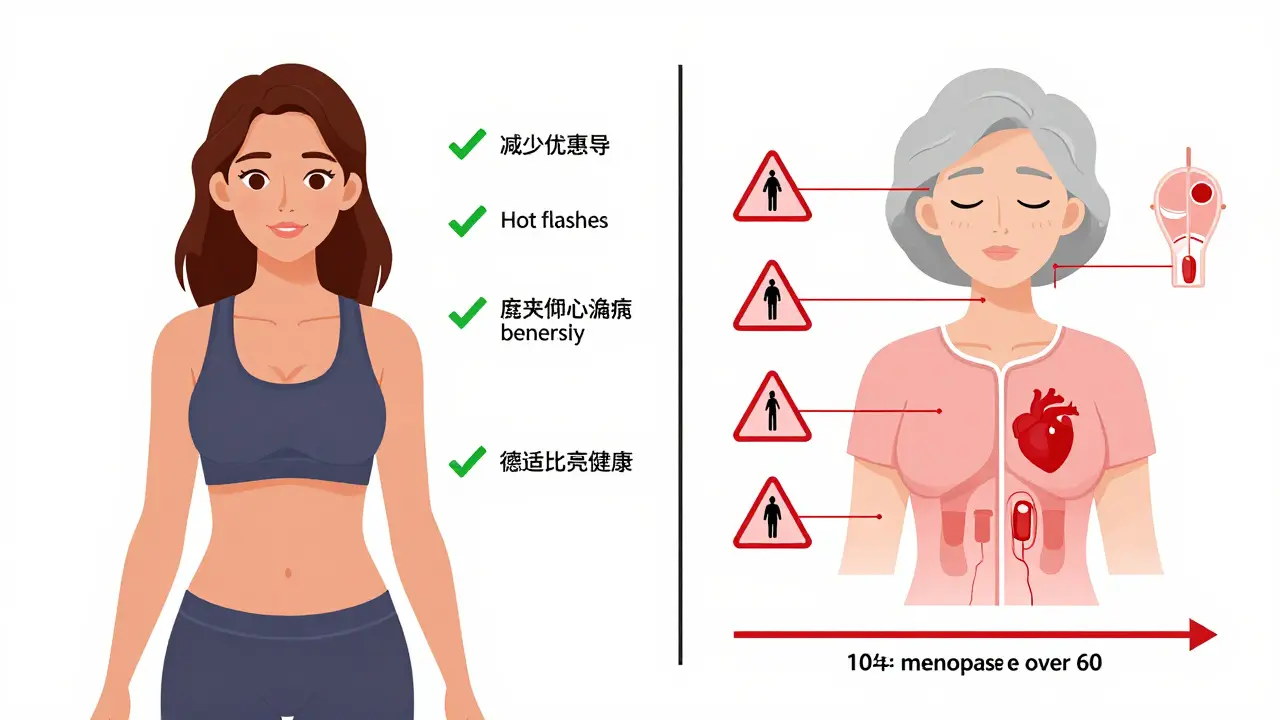
Menopause hormone therapy (MHT), often called hormone replacement therapy or HRT, isn’t a one-size-fits-all treatment. It’s designed to replace the estrogen (and sometimes progesterone) your body stops making after menopause. The goal? To ease the most disruptive symptoms: hot flashes, night sweats, vaginal dryness, and sleep disruption.Here’s the truth: hormone therapy is still the most effective treatment we have for these symptoms. Studies show it reduces hot flashes by 75% or more compared to placebo. For women who are having 15 or more hot flashes a day, the difference between taking HRT and not taking it can mean the difference between functioning normally and being trapped in discomfort.
It’s not just about comfort. Estrogen helps protect bone density. Women who skip hormone therapy after menopause lose bone at a rate of 2-3% per year in the first five years. That’s why many doctors recommend MHT for women at risk of osteoporosis-especially if they’re under 60 or within 10 years of their last period.
The Risks: What the Data Really Shows
The fear around hormone therapy started in 2002, after the Women’s Health Initiative study linked HRT to increased risks of breast cancer, heart disease, stroke, and blood clots. That study changed everything. Millions of women stopped taking it overnight.But here’s what didn’t make the headlines: those risks weren’t the same for everyone. The biggest dangers showed up in women who started hormone therapy *after* age 60-or more than 10 years after menopause began. For healthy women who start therapy closer to menopause, the risks drop significantly.
Let’s break it down:
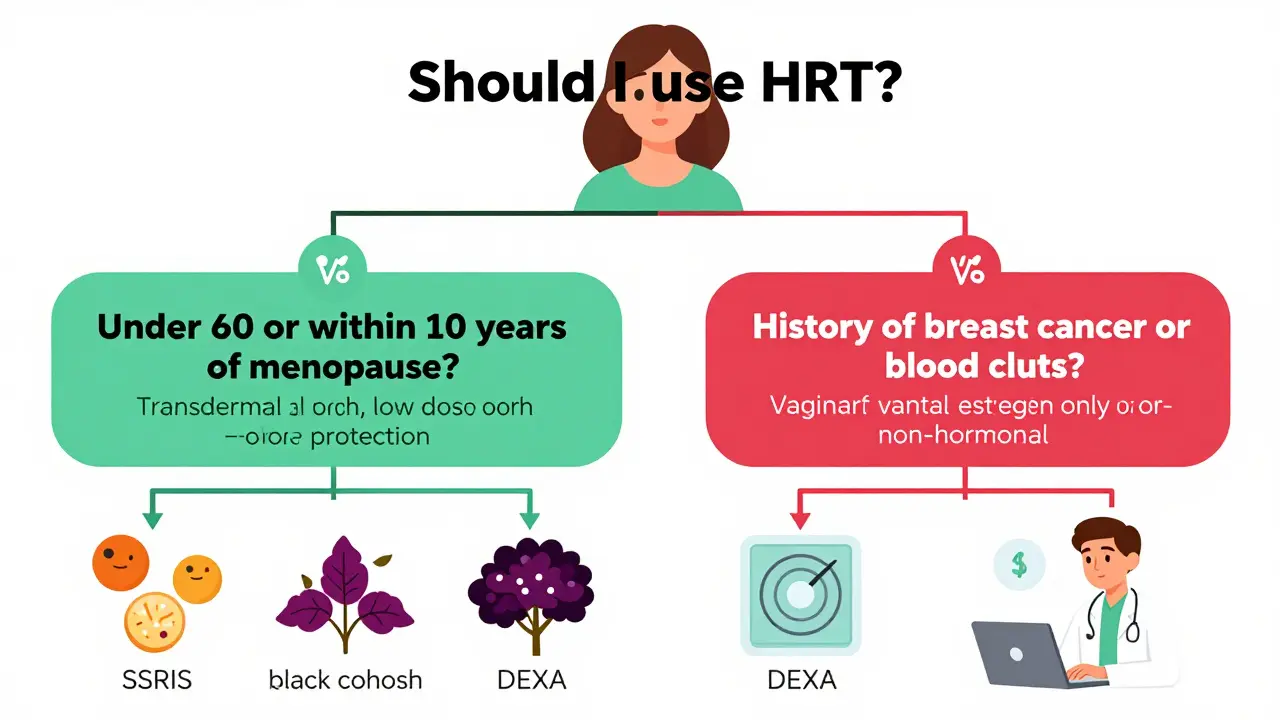
- Breast cancer: Estrogen-plus-progestogen therapy increases risk by about 29 extra cases per 10,000 women per year. Estrogen-only therapy (for women who’ve had a hysterectomy) shows almost no increase-just 9 extra cases per 10,000 women per year.
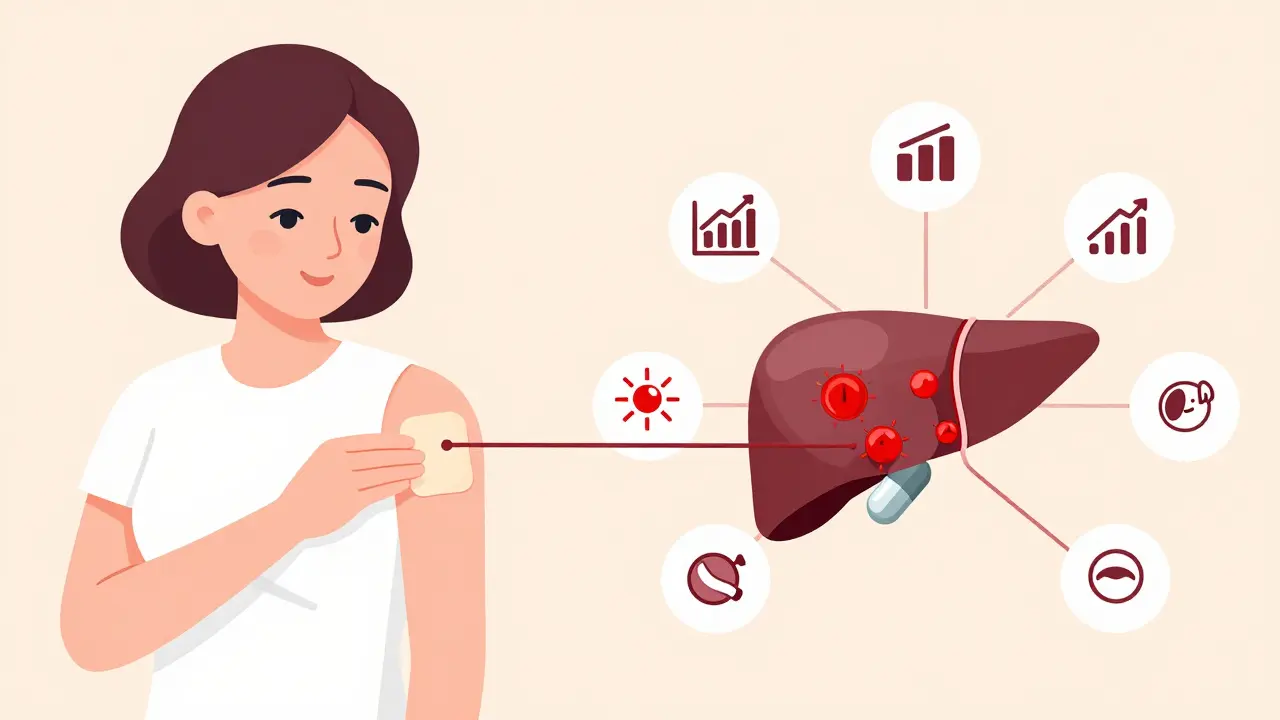
- Stroke: Oral estrogen raises stroke risk by about 30%. Transdermal estrogen (patches or gels) doesn’t carry that same risk. In fact, studies show transdermal estrogen may reduce stroke risk by 30% compared to pills.
- Blood clots: Oral estrogen increases the chance of dangerous clots by 2-3 times. Transdermal estrogen doesn’t. That’s because pills go through the liver first, triggering clotting factors. Patches skip that step.
- Heart disease: Starting HRT after age 60 or more than 10 years after menopause may slightly raise heart disease risk. Starting before then? No increased risk-and possibly some protection.
That’s why experts now talk about the “timing hypothesis”: starting hormone therapy early, when your body still responds well to estrogen, makes all the difference.
Forms of Therapy: Pills, Patches, Gels, and More
Not all hormone therapies are created equal. The delivery method matters as much as the dose.Oral estrogen (pills like Premarin or generic estradiol) is the most common-but also the riskiest for blood clots and stroke. It’s often prescribed at 0.3-0.625 mg of conjugated equine estrogens or 0.5-2 mg of 17-beta estradiol daily.
Transdermal estrogen (patches, gels, sprays) is now the preferred choice for most women. Doses range from 0.025-0.1 mg per day. These deliver estrogen directly into the bloodstream, avoiding the liver. That means lower risk of clots, stroke, and liver stress. Many women report fewer side effects, too.
Progestogen is added if you still have a uterus. Without it, estrogen can cause endometrial cancer. Micronized progesterone (like Prometrium) is safer than older synthetic versions like medroxyprogesterone acetate. It’s less likely to cause mood swings or bloating.
Vaginal estrogen (creams, rings, tablets) is a low-dose option for dryness and discomfort during sex. It doesn’t affect the rest of your body much, so it’s safe even for women with a history of breast cancer.
What About Non-Hormonal Options?
Some women want to avoid hormones entirely. That’s okay-but know what you’re giving up.Antidepressants like SSRIs (e.g., paroxetine) can reduce hot flashes by about half. Gabapentin helps too, but causes dizziness in 1 out of 4 users. Herbal remedies like black cohosh or soy isoflavones? A Cochrane Review found they reduce hot flashes by less than one per day compared to placebo. That’s barely better than nothing.
These alternatives are useful for mild symptoms or women who can’t take hormones. But if your symptoms are severe-waking you up multiple times a night, ruining your focus at work, making you feel like you’re melting-nothing else comes close to hormone therapy.
Who Should Avoid Hormone Therapy?
HRT isn’t for everyone. You should avoid it if you have:- A personal history of breast cancer
- Active blood clots or a history of deep vein thrombosis or pulmonary embolism
- Uncontrolled high blood pressure
- Undiagnosed abnormal vaginal bleeding
- History of stroke or heart attack
- Liver disease
Family history of breast cancer? That’s not a hard stop. But it does mean you need to be extra careful about dose, duration, and formulation. Talk to a specialist.
How to Get Started (And When to Stop)
There’s no rush. You don’t need to decide today. But if you’re considering it, here’s how to begin:- Track your symptoms for a month. Use a journal or app. How often do hot flashes happen? How bad is the sleep disruption?
- See a provider who understands menopause-not just your OB-GYN, but ideally someone certified in menopause care. The North American Menopause Society has a directory of certified practitioners.
- Get a basic checkup: blood pressure, cholesterol, and maybe a bone density scan if you’re over 55.
- Start low. Most women begin with 0.5 mg of oral estradiol or a 0.025 mg transdermal patch.
- Reassess in 3 months. Are symptoms better? Any side effects? Adjust as needed.
How long should you stay on it? There’s no fixed expiration date. Many women take it for 3-5 years. Some stay on longer if symptoms return after stopping. The key is using the lowest dose that works and reviewing your plan every year.
Real Stories: What Women Are Saying
On forums and patient groups, the stories are powerful:- “I went from 20 hot flashes a day to 2-3 within 10 days on a patch. I slept through the night for the first time in years.” - Reddit, March 2024
- “I quit after 3 months because of bloating and mood swings. Switched to transdermal and now I’m on it 7 years later with no issues.” - HealthUnlocked, August 2024
- “My DEXA scan showed I kept my bone density after 8 years. My sister, who refused HRT, broke her hip at 62.” - Menopause Society Forum, January 2025
But the fear is real too. A 2023 survey found 72% of women stopped HRT because they were scared of breast cancer-even when their doctor said the risk was low.
The Big Picture: Is It Worth It?
The data doesn’t lie: for healthy women under 60 or within 10 years of menopause, the benefits of hormone therapy outweigh the risks. It’s not a magic bullet. It’s not for lifelong use. But for those struggling with debilitating symptoms or at risk for bone loss, it’s one of the most effective tools we have.The old fear-“HRT is dangerous”-has been replaced by a smarter, more nuanced understanding. It’s not about whether you take it. It’s about when, how, and for how long.
Doctors are now more confident than ever in prescribing it the right way: low dose, transdermal when possible, short term for symptoms, and never for preventing heart disease or dementia. That’s the new standard.
If you’re unsure, get a second opinion. Talk to a menopause specialist. Don’t let outdated warnings stop you from feeling like yourself again.
Is hormone therapy safe for women over 60?
For women over 60, or more than 10 years past menopause, hormone therapy is generally not recommended for symptom relief unless other options have failed. The risks of stroke, blood clots, and heart disease rise with age, and the benefits for symptoms are less clear. If symptoms are severe, transdermal estrogen at the lowest dose may still be considered-but only after careful discussion with a specialist.
Does hormone therapy cause weight gain?
No, hormone therapy itself doesn’t cause weight gain. The weight gain many women experience around menopause is due to aging, changing metabolism, and declining muscle mass-not estrogen or progesterone. Some women report water retention or bloating early on, especially with oral pills, but this usually improves with dose adjustment or switching to a patch.
Can I use hormone therapy if I’ve had breast cancer?
Systemic hormone therapy (pills, patches, gels) is generally avoided in women with a history of estrogen-receptor-positive breast cancer. However, low-dose vaginal estrogen is considered safe and effective for treating vaginal dryness and discomfort. Always consult your oncologist before starting any hormone treatment.
How long should I take hormone therapy?
There’s no set time limit. Most women take it for 3-5 years to manage symptoms. If symptoms return after stopping, it’s okay to restart. The goal is to use the lowest effective dose for the shortest time needed. Annual check-ins with your doctor help determine if you still need it.
Are natural or herbal options safer than HRT?
Natural doesn’t mean safer or more effective. Herbal supplements like black cohosh, red clover, or soy isoflavones have inconsistent results and aren’t regulated like prescription medications. A Cochrane Review found they reduce hot flashes by less than one per day compared to placebo. They may help mild symptoms, but they don’t match the reliability of hormone therapy for moderate to severe symptoms.
What’s Next for Menopause Care?
The field is changing fast. In 2025, new guidelines are expected to formalize the “window of opportunity” concept-starting therapy before age 60 or within 10 years of menopause gives the best safety profile. Researchers are also exploring genetic testing to predict how your body metabolizes estrogen, which could one day guide personalized dosing.Meanwhile, more employers are offering menopause support programs. Companies like Google, Salesforce, and Unilever now provide education, counseling, and even access to specialists-because menopause affects productivity, focus, and well-being.
What hasn’t changed is this: you deserve to feel good. Menopause isn’t a disease. But the symptoms can be debilitating. Hormone therapy, when used correctly, isn’t a risk-it’s a recovery tool.





15 Comments