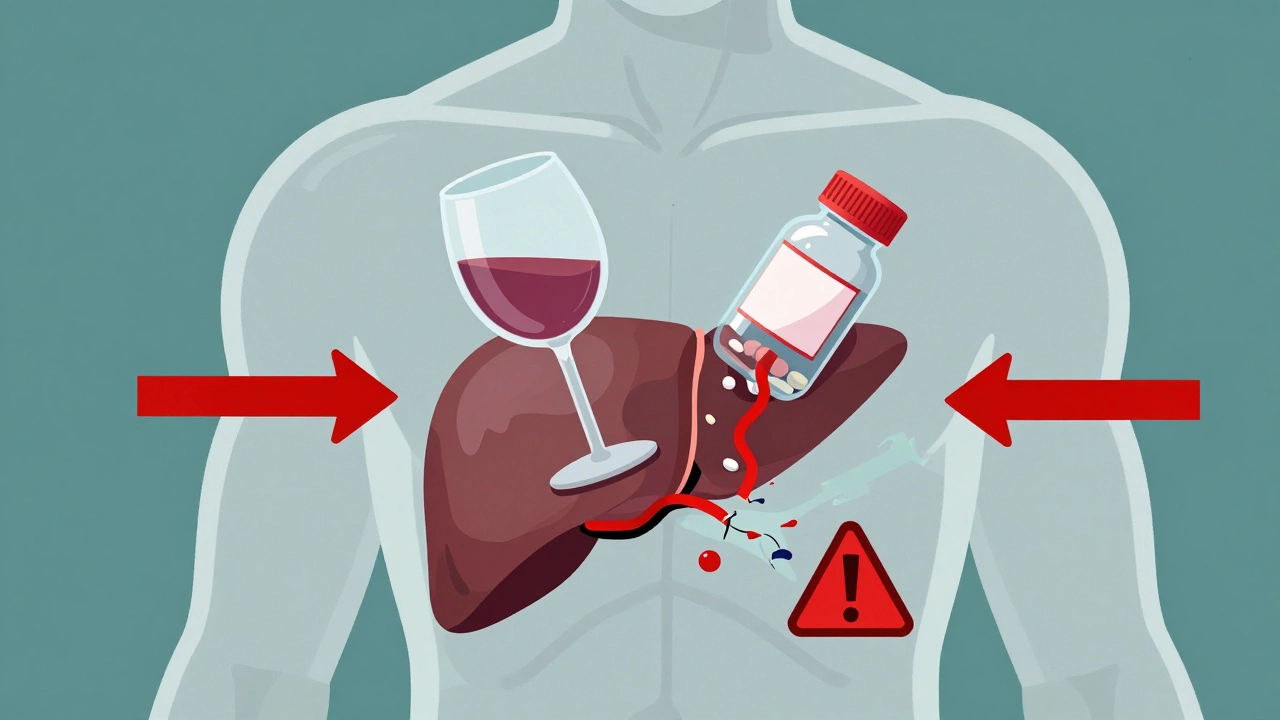
Combining alcohol with prescription medications isn’t just a bad idea-it can kill you. Every year, over 2,300 people in the U.S. die from alcohol-drug interactions, many of them older adults who didn’t realize their daily wine or beer was turning their medicine into a silent threat. This isn’t about binge drinking or street drugs. It’s about the pill you take for anxiety, pain, or sleep-and the glass of wine you have with dinner. These two things, taken together, can shut down your breathing, wreck your liver, or send you into a coma-even if you’re following your doctor’s orders exactly.
How Alcohol Changes How Your Medicines Work
Alcohol doesn’t just mix with drugs. It changes how your body handles them. There are two main ways this happens: pharmacokinetic and pharmacodynamic interactions.Pharmacokinetic interactions mess with how your body breaks down the drug. Most medications and alcohol are processed by the same liver enzymes, especially the CYP450 family. When you drink regularly, your body starts making more of these enzymes to handle the alcohol. That means drugs like propranolol (used for high blood pressure) get broken down too fast-your dose becomes useless. You might feel like the medication isn’t working, so you take more. That’s when things go wrong.
On the flip side, having even one drink right before taking a pill can slow down enzyme activity. That causes the drug to build up in your blood. Warfarin, a blood thinner, is a classic example. One drink can raise its levels by up to 35%, increasing your risk of dangerous bleeding. You don’t need to be drunk. Just one beer with your evening pill can be enough.
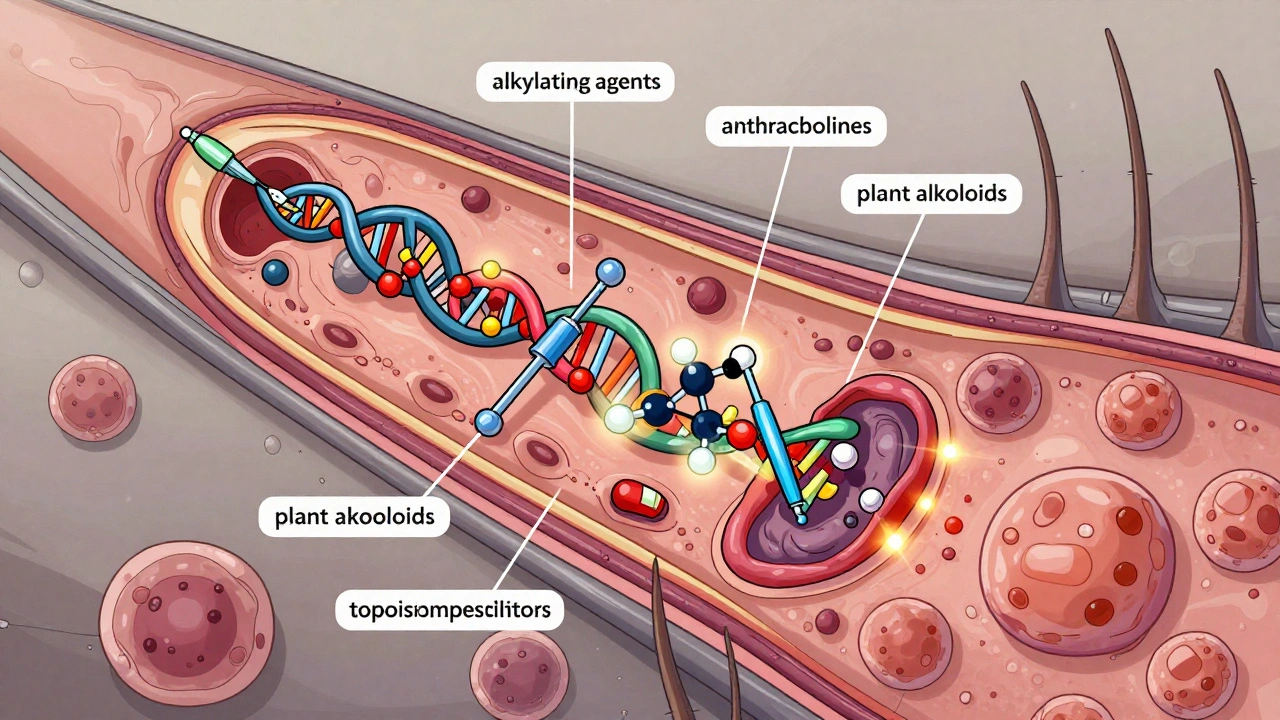
Pharmacodynamic interactions are even scarier. This is when alcohol and the drug amplify each other’s effects. Think of it like stacking two heavy weights on a scale. Benzodiazepines like Xanax or Valium already slow down your brain. Alcohol does the same. Together, they can depress your breathing to the point where you stop breathing entirely. Studies show this combo increases sedation by 400% compared to either substance alone. And it doesn’t take much. A blood alcohol level of just 0.02%-that’s one standard drink-can double your risk of a fatal crash if you’re also on opioids like oxycodone.
High-Risk Medications: What to Avoid With Alcohol
Some medications are deadly when mixed with alcohol. Here are the top offenders:- Opioids (oxycodone, hydrocodone, morphine): These are the biggest killers. Alcohol and opioids together suppress your respiratory system. The CDC says this combo causes 26% of all prescription drug overdose deaths. Even a single drink can push you over the edge.
- Benzodiazepines (alprazolam, diazepam, lorazepam): Used for anxiety and sleep, these drugs make you drowsy. Alcohol makes that drowsiness extreme. In older adults, this combo increases fall risk by 50%. One study found 78% of falls in nursing homes involving sedatives happened within six hours of alcohol use.
- Acetaminophen (Tylenol): This common painkiller turns toxic when mixed with alcohol. Your liver turns acetaminophen into a harmful byproduct. Alcohol pushes your liver to make even more of it. For regular drinkers, just a few doses of Tylenol can cause acute liver failure. The FDA says 1 in 200 regular users who drink alcohol while taking acetaminophen end up in the hospital with liver damage.
- NSAIDs (ibuprofen, naproxen): These pain relievers already irritate your stomach lining. Alcohol does the same. Together, they can cause severe bleeding in your digestive tract. Heavy drinkers who take NSAIDs have a 300% higher risk of gastrointestinal bleeding.
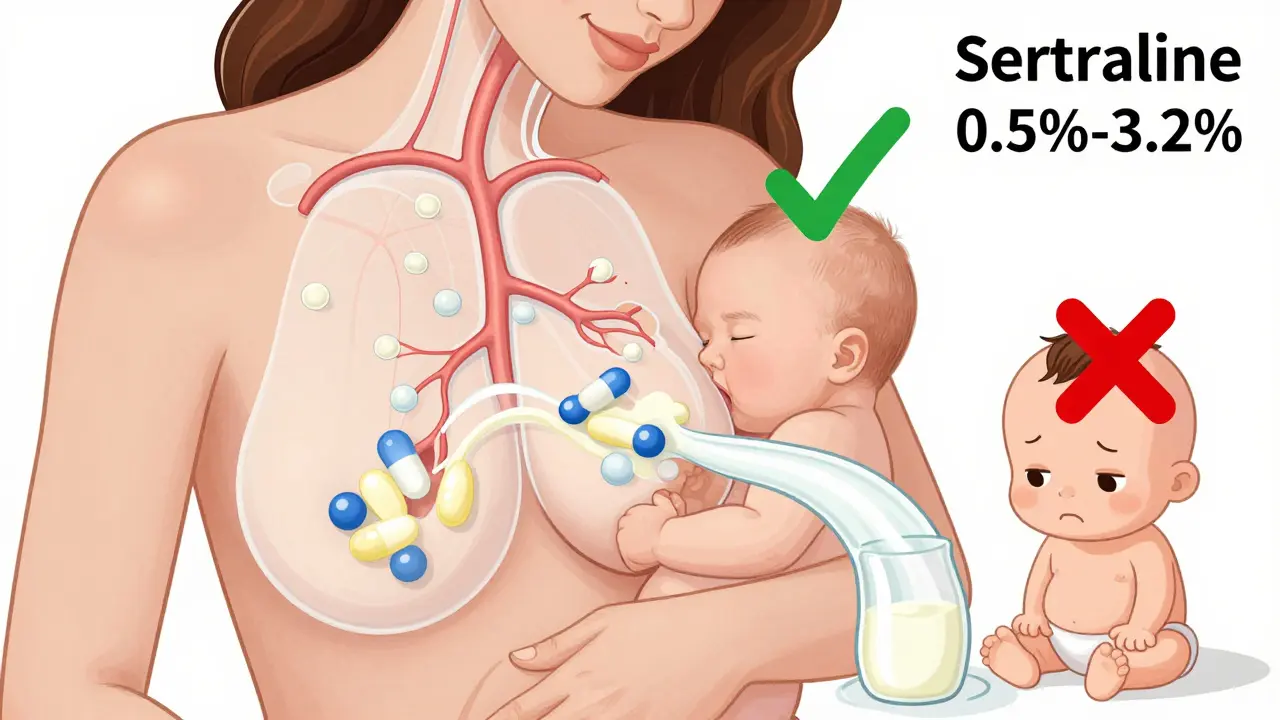
- Antidepressants (SSRIs like sertraline, fluoxetine): While not usually deadly, alcohol makes drowsiness and dizziness worse. In people over 65, this increases fall risk by double. One study found 35% of older adults on SSRIs experienced dangerous drowsiness even with just one drink a day.
- Antibiotics (isoniazid): Not all antibiotics are risky, but isoniazid (used for tuberculosis) can cause liver damage when mixed with alcohol. About 15% of users develop serious toxicity.
Who’s at Greatest Risk?
Not everyone is equally vulnerable. Certain groups face much higher danger:- Adults over 65: Your liver processes alcohol and drugs slower. You also tend to take more medications. Older adults experience 3.2 times more severe interactions than younger people.
- Women: Women have less body water than men, so alcohol concentrates more in their blood. This means the same amount of alcohol affects them 20% more than men.
- People with liver disease: If your liver is already damaged from hepatitis, fatty liver, or long-term drinking, even small amounts of alcohol can trigger severe reactions with medications like acetaminophen. Your risk of liver failure jumps fivefold.
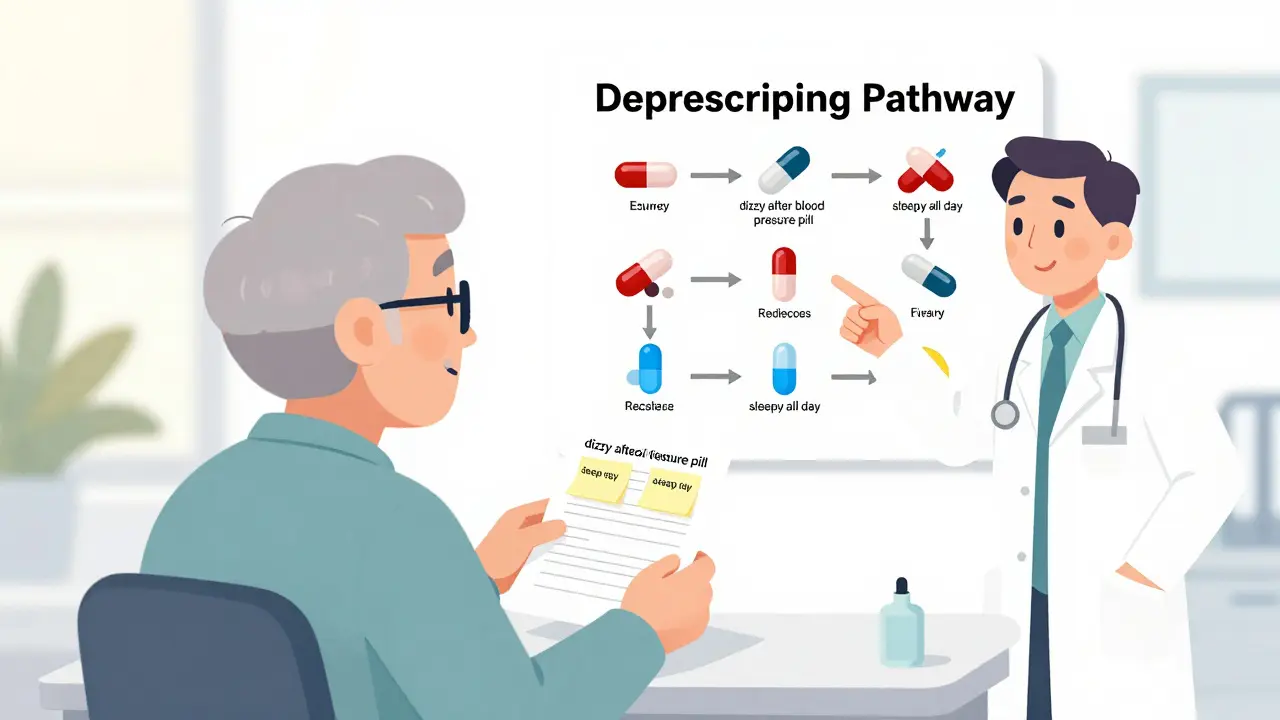
- People taking multiple medications: The more drugs you take, the more chances for interaction. Polypharmacy (taking five or more meds) is common in older adults-and it’s a recipe for disaster when alcohol is added.

Why Doctors and Pharmacists Often Don’t Warn You
You’d think your doctor would tell you. But they often don’t. A 2023 study found that 68% of patients prescribed benzodiazepines were never warned about alcohol risks. Many doctors assume patients know-or don’t drink. Others simply forget. A survey of primary care physicians showed 43% couldn’t correctly identify all the high-risk drug classes.Pharmacists are often the last line of defense. But even they’re not always alerted. Only 38% of benzodiazepine prescriptions include an explicit alcohol warning on the label, according to an FDA audit. That means you’re left guessing.
Some patients have had life-saving experiences because a pharmacist stepped in. One Google Review from a Walgreens customer said: “My pharmacist refused to fill my lorazepam prescription when I admitted to regular drinking-probably saved my life.” That kind of intervention is rare, though. Most pharmacies don’t have time or systems to screen every patient.
What You Can Do Right Now
You don’t need to be a medical expert to protect yourself. Here’s what works:- Check your medication labels. Look for the words “avoid alcohol” or “may cause drowsiness.” About 65% of high-risk prescriptions have this warning-but many don’t.
- Ask your pharmacist. Don’t just pick up your prescription. Ask: “Is it safe to drink alcohol with this?” Use the four-question screening tool recommended by the Annals of Internal Medicine: “Do you drink alcohol? How often? How much? Have you noticed any side effects when you drink and take your meds?”
- Use a free app. The NIAAA’s “Alcohol Medication Check” app lets you scan your prescription barcode or search by name. It cross-references over 2,300 medications and gives you a risk level: red, yellow, or green.
- Be honest. If you drink-even one glass of wine a night-tell your doctor. They can’t help if they don’t know.
- Use visual aids. A 2023 GoodRx study showed patients who saw color-coded risk charts (red = dangerous, yellow = caution, green = safe) understood their risks 47% better than those who only read text.

The Bigger Picture: Why This Problem Is Getting Worse
The market for drug interaction software is booming-projected to hit $2.8 billion by 2030. Hospitals like the VA now use real-time systems that flag alcohol-drug risks before a prescription is filled. In places with full implementation, adverse events dropped by 28%.But outside of hospitals, progress is slow. Only 32% of private practices use these tools. New regulations like the 2022 Alcohol-Drug Interaction Labeling Act are supposed to fix that, requiring clear warnings on high-risk prescriptions. But enforcement is patchy.
Meanwhile, new dangers are emerging. The rise of cannabis use means some people are now mixing alcohol, prescription drugs, and marijuana. One expert warns this triple interaction could affect 14 million Americans. The data isn’t fully in yet-but the risk is real.
Bottom Line: When in Doubt, Skip the Drink
There’s no safe gray area with high-risk medications. If you’re on opioids, benzodiazepines, or acetaminophen, alcohol has no place in your routine. Even one drink can tip the balance from manageable to deadly.For lower-risk meds, like some antibiotics or blood pressure drugs, occasional light drinking might be okay-but only if your doctor says so. And even then, don’t assume it’s safe. Your body changes. Your meds change. Your drinking habits change. What was fine last year might not be today.
The truth is, this isn’t about willpower or discipline. It’s about information. Too many people die because they didn’t know. You don’t have to be one of them. Ask. Check. Pause. Your life depends on it.
Can I have one drink with my prescription painkiller?
No. Even one drink with opioids like oxycodone or hydrocodone can double your risk of fatal respiratory depression. Blood alcohol levels as low as 0.02%-equivalent to one standard drink-are enough to make these drugs deadly. There is no safe amount.
Is it safe to drink wine with my antidepressant?
It’s not recommended. While SSRIs like sertraline aren’t usually deadly with alcohol, the combination increases drowsiness, dizziness, and impaired coordination. For people over 65, this doubles fall risk. Even one glass of wine can make you unsteady. If you’re on an SSRI, skip alcohol-or talk to your doctor first.
What should I do if I accidentally mixed alcohol with my medication?
If you feel unusually drowsy, confused, have trouble breathing, or feel like you might pass out, call emergency services immediately. Don’t wait. Don’t try to sleep it off. Alcohol-drug interactions can progress rapidly. If you’re unsure but feel off, contact your pharmacist or poison control center right away.
Do all medications have alcohol warnings on the label?
No. Only about 38% of benzodiazepine prescriptions and 65% of high-risk medications include clear alcohol warnings. Many labels say “may cause drowsiness” without mentioning alcohol. Never assume safety based on the label alone. Always ask your pharmacist.
Can I drink alcohol if I take my medication only once a week?
It depends on the drug. For medications like acetaminophen or warfarin, even occasional use with alcohol can be dangerous. The risk isn’t about frequency-it’s about how your body processes the drug at the time you drink. If you’re on a weekly medication with known alcohol interactions, avoid alcohol entirely unless your doctor gives you a clear, written green light.
Are there any medications that are safe with alcohol?
Some, like amoxicillin or most antihistamines, have minimal interaction risk. But “minimal” doesn’t mean “safe.” Even these can cause drowsiness or upset stomach when mixed. The safest approach is to assume alcohol interacts with any prescription unless your doctor or pharmacist confirms otherwise. Never rely on internet rumors or old advice.




16 Comments