Diabetic retinopathy isn’t just a complication of diabetes-it’s the leading cause of preventable vision loss in adults under 65. If you or someone you care about has diabetes, ignoring eye health isn’t an option. But here’s the truth: not everyone needs an eye exam every year. And not every case needs laser surgery or injections. The right approach depends on your risk, your numbers, and your history.
What Is Diabetic Retinopathy, Really?
Diabetic retinopathy happens when high blood sugar damages the tiny blood vessels in the retina-the light-sensitive layer at the back of your eye. At first, you won’t notice anything. No pain. No blurry vision. That’s why it sneaks up on so many people. By the time symptoms show up, damage might already be advanced.
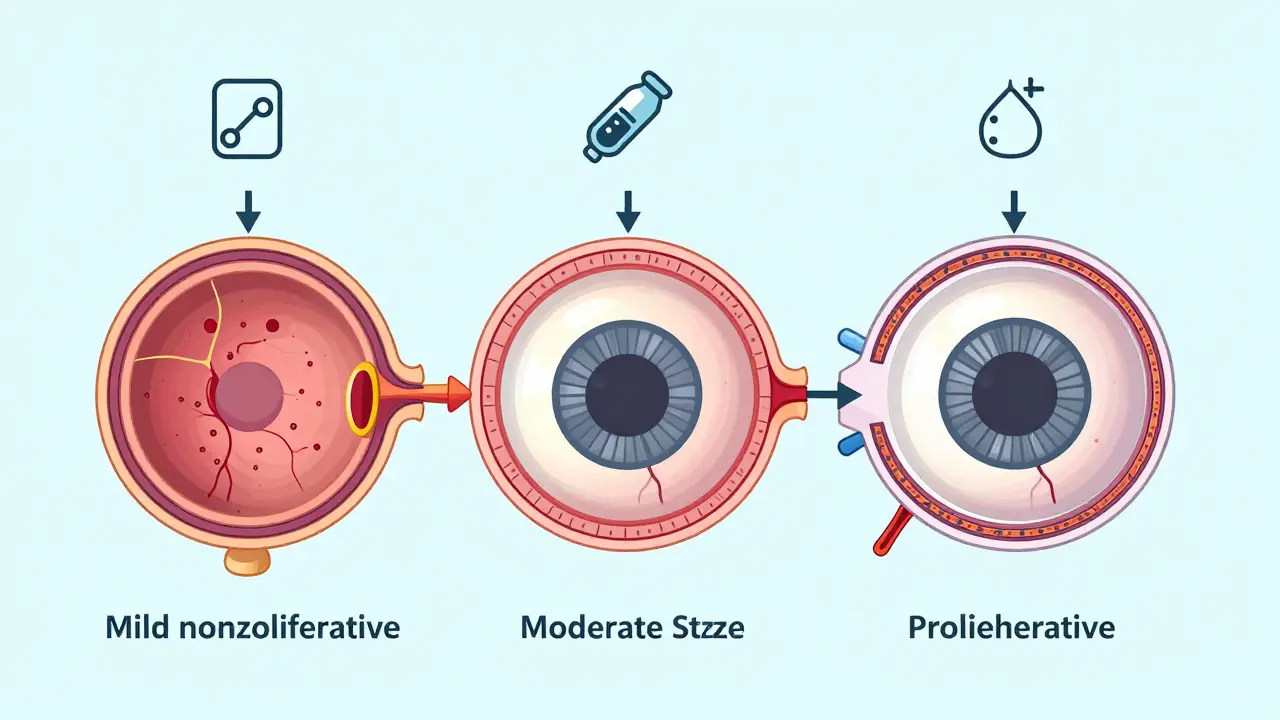
The condition progresses in stages. It starts as mild nonproliferative diabetic retinopathy (NPDR), where small vessels leak fluid. Then it can move to moderate or severe NPDR, with more widespread damage. The scariest stage is proliferative diabetic retinopathy (PDR), where the eye tries to grow new blood vessels-weak, fragile ones that bleed easily and can scar the retina, pulling it loose. Diabetic macular edema (DME), a swelling in the central part of the retina, can happen at any stage and is the most common cause of vision loss.
Here’s what the numbers say: about 1 in 3 people with diabetes have some form of retinopathy. And while that sounds alarming, up to 98% of severe vision loss from diabetic retinopathy can be prevented with timely screening and treatment. That’s not a guess-it’s backed by decades of clinical research.
When Should You Get Screened? It’s Not One-Size-Fits-All
For years, the rule was simple: get your eyes checked every year. But that’s outdated. Today, screening is personalized. Your risk level determines how often you need an exam.
For people with type 2 diabetes, if you’ve had two straight clean screenings with no signs of retinopathy and your HbA1c is under 7%, blood pressure is controlled, and you have no kidney issues, you can safely wait 2 to 4 years between screenings. A 2022 review of over 100,000 patients found no increase in vision-threatening cases when low-risk patients were screened every 3 years instead of every year.
For type 1 diabetes, screening starts 3 to 5 years after diagnosis. If you’ve had no retinopathy for 3+ years and your diabetes is well-controlled, you can extend intervals to every 2 years. The DCCT/EDIC study showed that intensive glucose control cuts the risk of retinopathy by 76% in type 1 patients-so if your numbers are good, you don’t need to be in the eye doctor’s chair every 12 months.
But if you have even mild retinopathy? That changes everything. Moderate NPDR means you need to see an ophthalmologist every 3 to 6 months. Severe NPDR? You need to be seen within 3 months. Proliferative retinopathy? That’s an emergency-get evaluated within 30 days.
There’s a tool called RetinaRisk that helps doctors calculate your personal risk. It uses your HbA1c, how long you’ve had diabetes, your blood pressure, and kidney function to predict your chance of progression. One study found this method reduces unnecessary screenings by 59% without missing a single case of sight-threatening disease.
What Does a Screening Actually Involve?
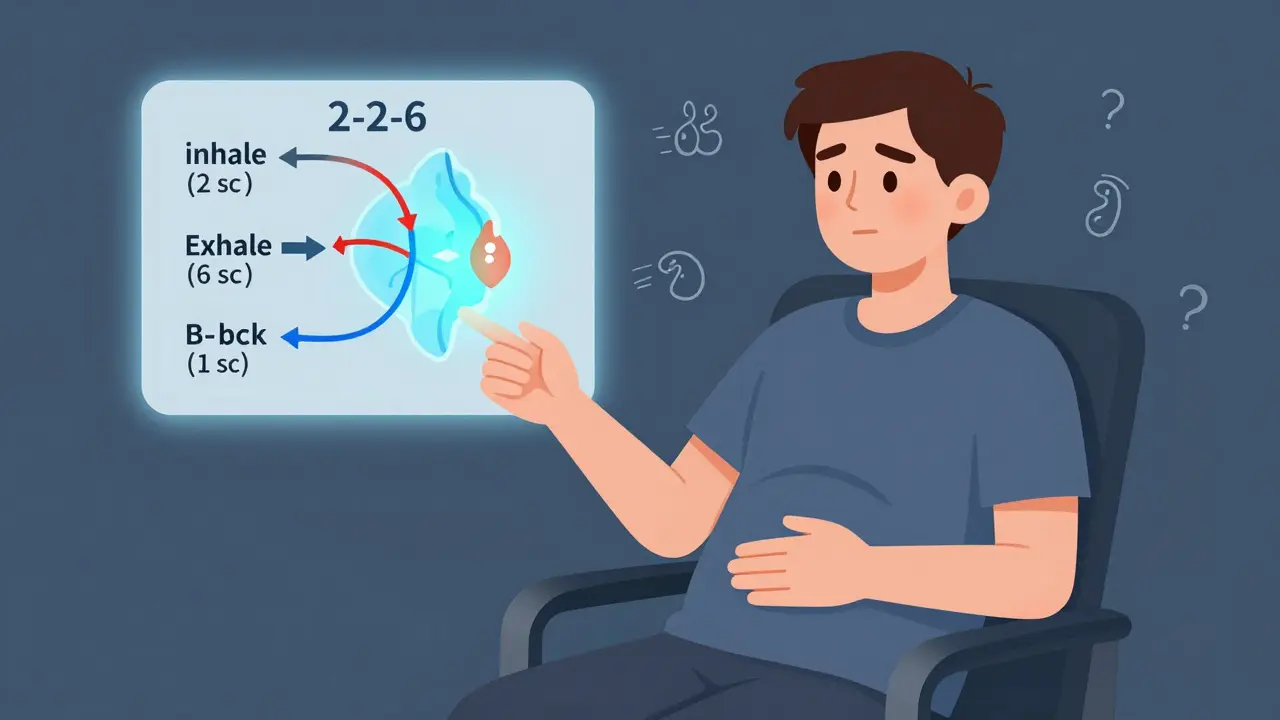
A standard diabetic eye screening isn’t a quick glance. It’s a detailed digital photo of your retina. Most clinics use mydriatic fundus photography-drops to widen your pupils, then a camera takes two or more high-res images of each eye. The images are graded using the International Clinical Diabetic Retinopathy Scale, which has five levels from no retinopathy to proliferative disease.
Some clinics now use AI-powered systems. Google’s DeepMind algorithm, for example, analyzes images with 94.5% accuracy in spotting sight-threatening changes. The FDA-cleared IDx-DR system lets primary care providers run screenings in their offices. In rural areas where ophthalmologists are scarce, telemedicine programs have boosted screening coverage from 50% to over 90% in some regions.
Don’t be fooled by smartphone adapters like D-Eye. While they’re convenient and 89% accurate, they’re not a replacement for full digital imaging if you’re at moderate or high risk. They’re best for initial checks in low-risk patients or in places with no access to traditional screening.

Treatment Options: From Injections to Surgery
If your screening finds something serious, you’re not out of options. In fact, most cases can be managed without surgery.
For diabetic macular edema (DME), the first-line treatment is anti-VEGF injections. Drugs like aflibercept, ranibizumab, and bevacizumab block the protein that causes leaking blood vessels. Most patients get monthly shots for 3 to 6 months, then spacing them out. Studies show these injections improve vision in over 80% of patients with DME.
Focal laser therapy is still used in some cases-especially if injections aren’t available or affordable. It seals off leaking vessels but doesn’t reverse damage. It’s less common now, but still effective for specific patterns of swelling.
For proliferative retinopathy, panretinal photocoagulation (PRP) laser treatment is the gold standard. It doesn’t restore vision, but it stops new abnormal vessels from forming and reduces the risk of severe bleeding by over 50%. If there’s already a lot of scar tissue or bleeding inside the eye, you might need a vitrectomy-a surgical procedure to remove the cloudy vitreous gel and repair the retina.
Here’s what most people don’t realize: the best treatment is prevention. Tight blood sugar control, managing blood pressure, and keeping cholesterol in check do more than anything else to slow or even stop retinopathy from getting worse. The UKPDS study showed that lowering HbA1c from 8.5% to 7% reduced retinopathy progression by 25% over 10 years.
Why Skipping Screenings Can Be Dangerous
Some patients avoid eye exams because they feel fine. Others can’t afford them. Some clinics push annual visits even when they’re not needed, creating burnout.
But here’s the risk: rapid progression can happen. A patient with HbA1c above 9%, uncontrolled blood pressure, or kidney disease can go from no retinopathy to sight-threatening disease in less than a year. One Reddit user shared how their clinic pushed for biennial screenings despite an HbA1c of 8.5%-and they developed macular edema within 14 months. That’s not rare.
On the flip side, a 2022 NHS survey of over 12,000 patients found 87% were happy with risk-based screening. They saved time, money, and stress. But 13% worried they’d miss something. That’s why clear communication matters. If your doctor changes your screening schedule, they should explain why-and give you a clear red flag list: blurred vision, floaters, dark spots, sudden vision loss-call immediately.
What You Can Do Right Now
You don’t need to wait for your next appointment to protect your vision.
- Keep your HbA1c under 7% if possible. Even small drops help.
- Get your blood pressure checked every visit. Aim for below 140/90.
- Ask your doctor about your kidney function. Microalbuminuria is a red flag for eye damage.
- Don’t ignore changes in your vision-even if they come and go.
- Know your screening history. Keep a log of your last exam and what was found.
- If you’re in a rural area, ask if telemedicine screening is available.
The goal isn’t to scare you. It’s to empower you. Diabetic retinopathy doesn’t have to steal your sight. With the right screening schedule and timely care, most people keep their vision for life.
What’s Changing in 2025?
Screening is getting smarter. AI tools are now part of routine care in many clinics. The American Diabetes Association’s 2024 guidelines strongly recommend risk-based intervals over fixed ones. More insurers are covering telemedicine screenings. And new point-of-care devices are making it easier for primary care doctors to catch problems early.
The World Health Organization estimates that if risk-stratified screening is adopted globally, we could prevent 2.5 million cases of blindness by 2030. But that only works if people get screened-and if doctors follow the evidence, not outdated habits.
The message is clear: don’t skip your eye check. But don’t assume every year is necessary. Work with your care team to find your personal schedule. Your eyes will thank you.
How often should I get screened for diabetic retinopathy if I have type 2 diabetes and no retinopathy?
If you have type 2 diabetes, no signs of retinopathy, and your HbA1c is below 7%, blood pressure is controlled, and you have no kidney disease, you can safely wait 2 to 4 years between screenings. After two consecutive clean exams, many guidelines recommend extending to every 3 years. But if your HbA1c is above 8% or you have other risk factors, annual screening is still advised.
Can diabetic retinopathy be reversed?
Early damage from diabetic retinopathy can sometimes stabilize or improve with better blood sugar control and treatment. Diabetic macular edema often responds well to anti-VEGF injections, with many patients regaining lost vision. However, once scar tissue forms or the retina detaches, the damage is permanent. That’s why early detection is critical-treatment stops progression, but it can’t undo advanced damage.
Are eye injections for diabetic retinopathy painful?
The injections are done with numbing drops, so you’ll feel pressure but not sharp pain. Most people describe it as a brief discomfort, like a pinch or a scratch. The whole process takes under 10 minutes. Some mild redness or floaters afterward are normal and fade within a day or two. Serious complications like infection are rare-less than 1 in 1,000 injections.
Can I skip eye exams if I’m not having vision problems?
Yes, you can skip exams only if your risk is low and your doctor confirms it’s safe. Diabetic retinopathy often causes no symptoms until it’s advanced. Many people with moderate or even severe retinopathy report no vision changes. That’s why regular screening-even when you feel fine-is the only reliable way to catch it early. Don’t rely on how your eyes feel.
Does insurance cover diabetic eye screenings?
In most cases, yes. In the U.S., Medicare and most private insurers cover annual diabetic eye exams under preventive benefits. Some plans now cover extended intervals for low-risk patients. In the UK, the National Health Service provides free screening for all people with diabetes. If you’re unsure, ask your provider or insurance company for your coverage under "diabetic retinopathy screening" or "diabetic eye exam."
What happens if I don’t get screened?
Without screening, diabetic retinopathy can progress silently. By the time you notice blurred vision, floaters, or blind spots, you may already have irreversible damage. Studies show that people who skip screenings are 5 times more likely to lose vision than those who follow recommended intervals. In low-income communities, lack of screening is the biggest reason for preventable blindness in people with diabetes.
Next Steps: What to Do Today
If you haven’t had an eye exam in over a year, call your eye doctor or primary care provider. Ask if you’re eligible for a risk-based screening schedule. If you’re already under care, review your last report. Did they mention NPDR? DME? What’s your HbA1c? Write it down.
If you’re a caregiver or family member, help your loved one track their numbers and appointments. Set phone reminders. Don’t let good intentions turn into missed screenings.
Diabetic retinopathy doesn’t have to be a death sentence for your vision. With the right knowledge, the right schedule, and timely treatment, you can keep seeing clearly-for years to come.




14 Comments